





 |
|||||
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
||
Meet Challenges
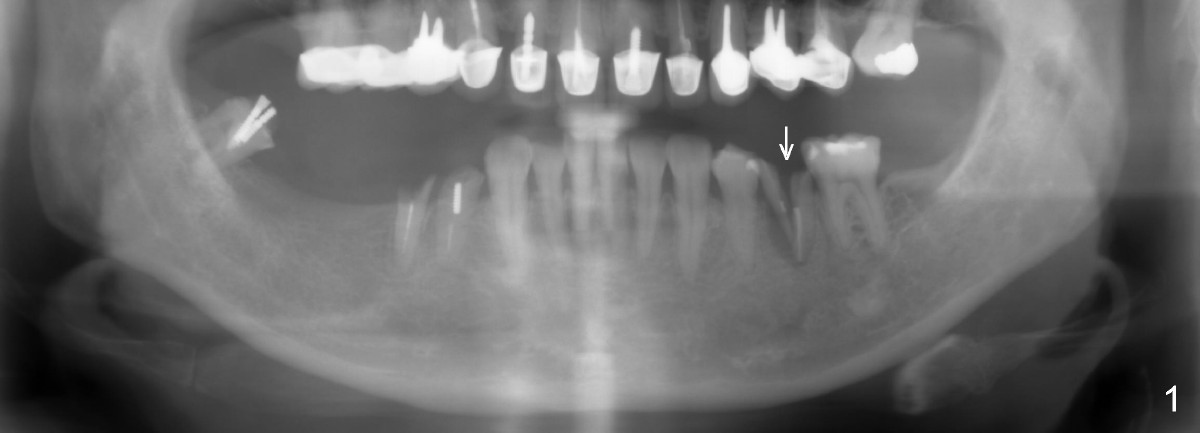
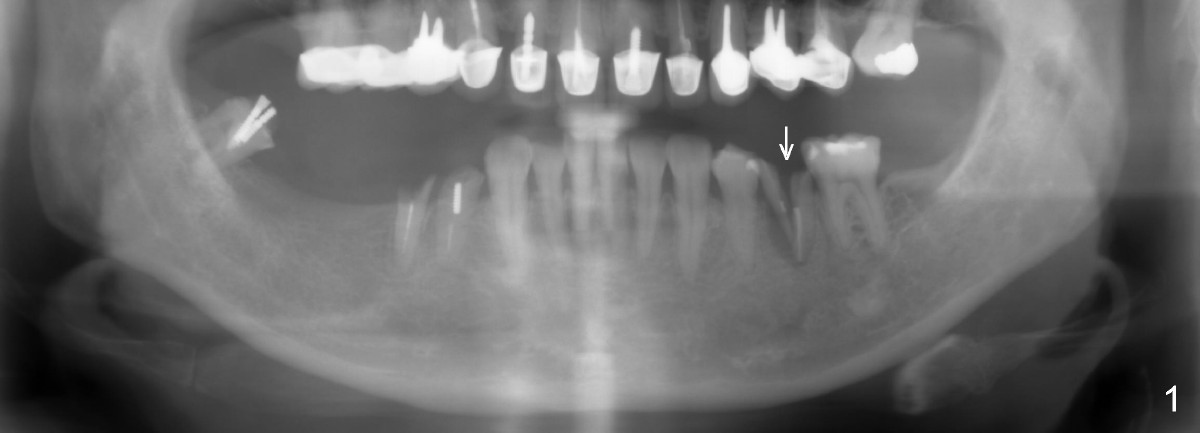
A 54-year-old lady has poor dentition. She seeks treatment because of pain associated with tooth fracture in the lower left 2nd premolar (Fig.1 arrow). The best option seems to be extraction and immediate implant. Thorough curettage after extraction is a key to get rid of infection.
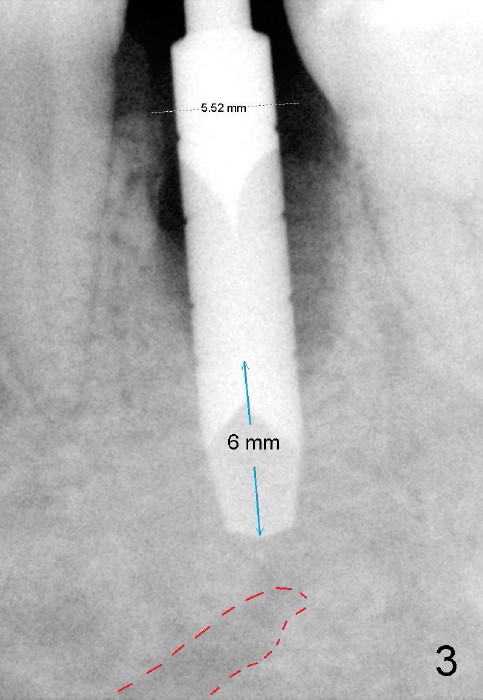
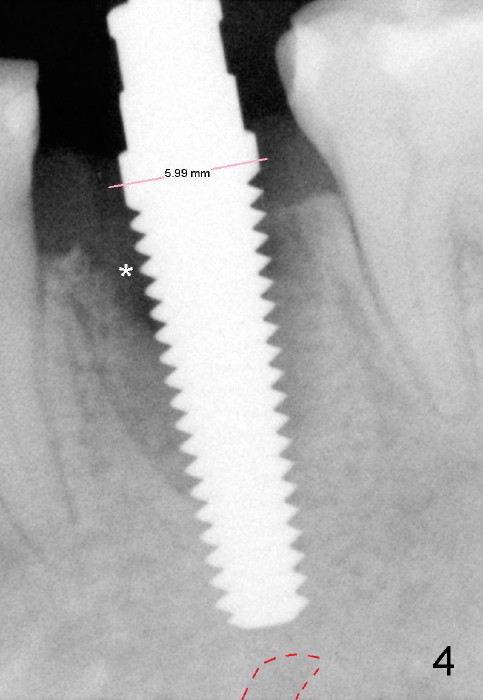
To avoid injury to the mental loop (Fig.2 dashed line), the depth of initial osteotomy is tightly controlled apical to the bottom of the socke. Accurate measuring is the 2nd important measure to assure no or minimal neurological trauma. The wide socket (due to infection) allows to place an implant as wide as 7 mm.
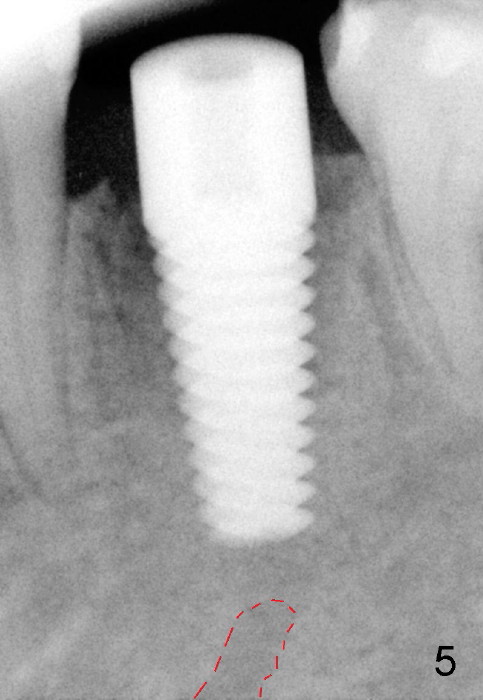
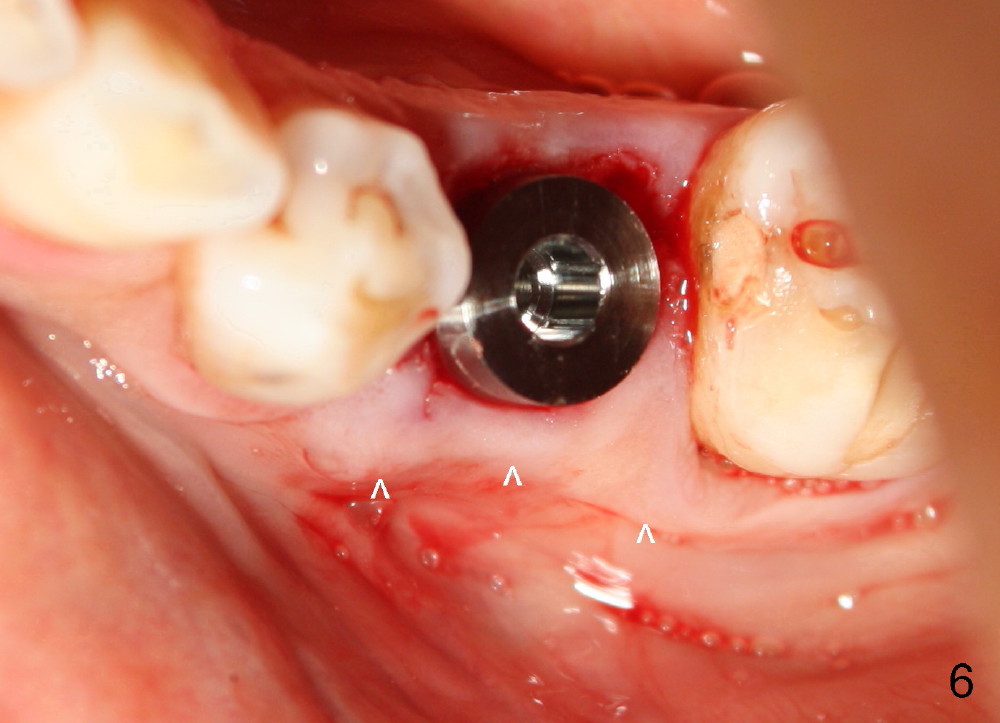
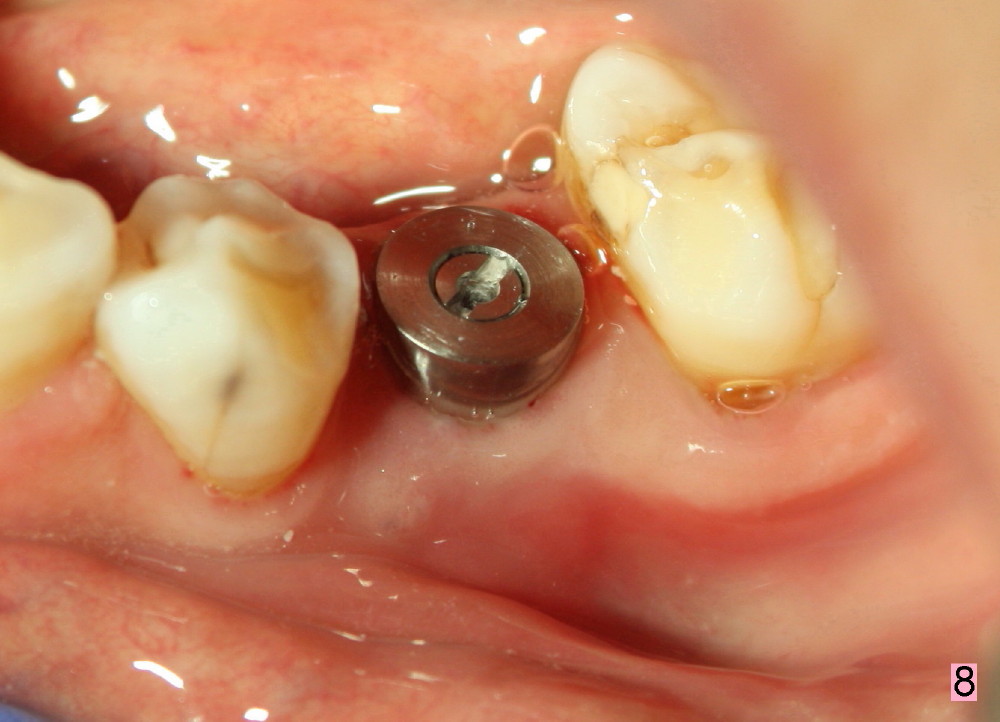
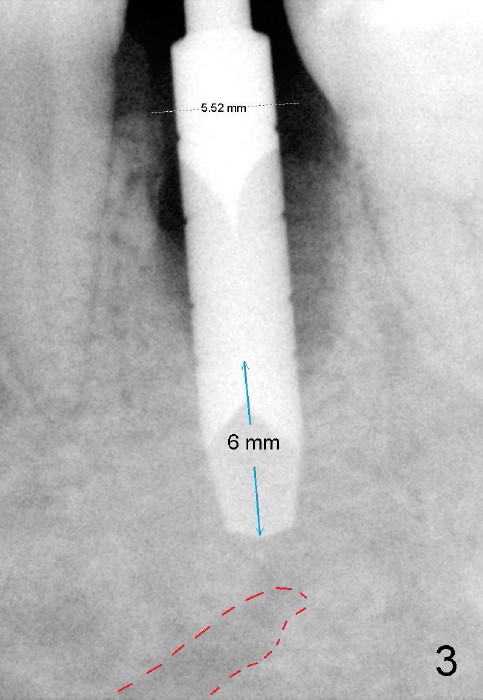
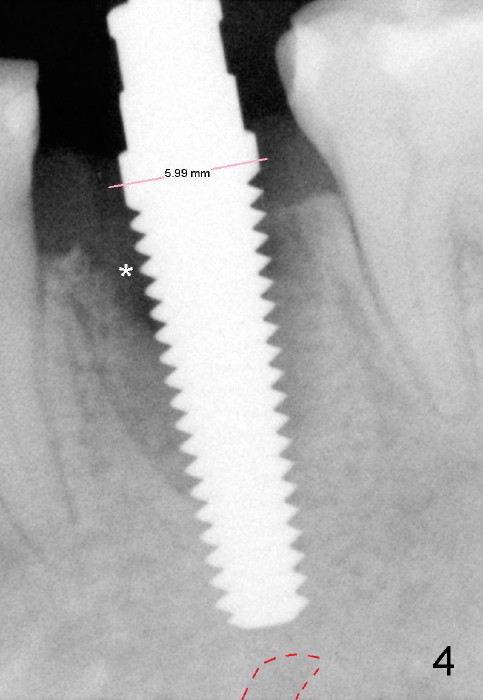
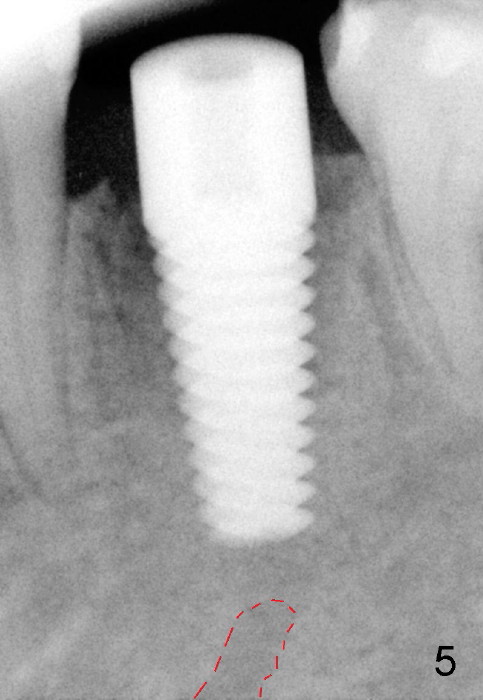
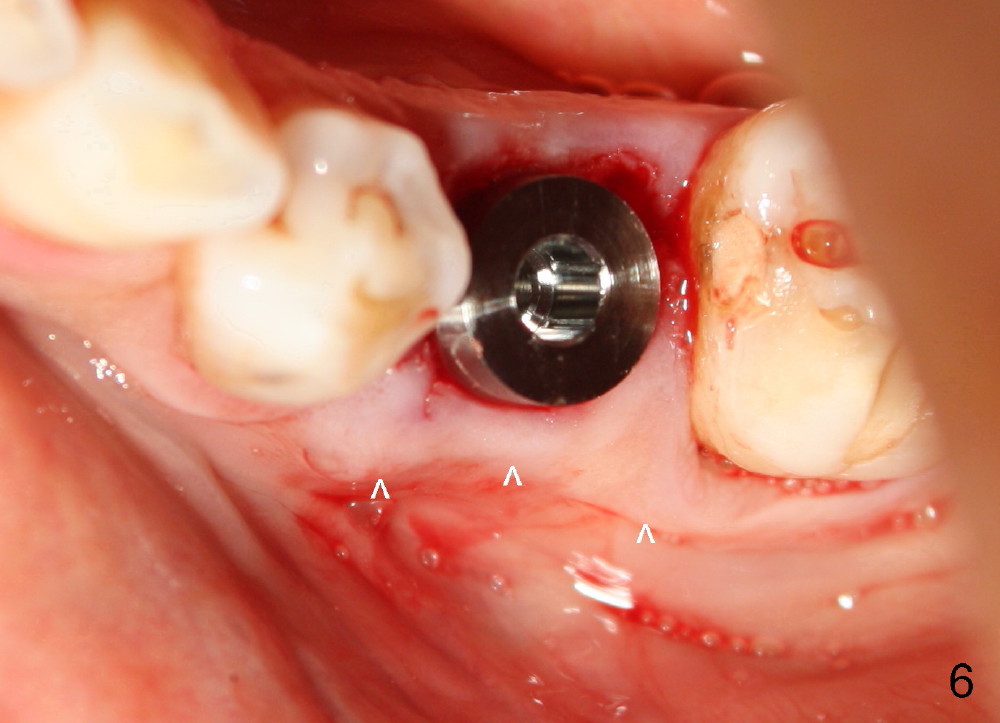
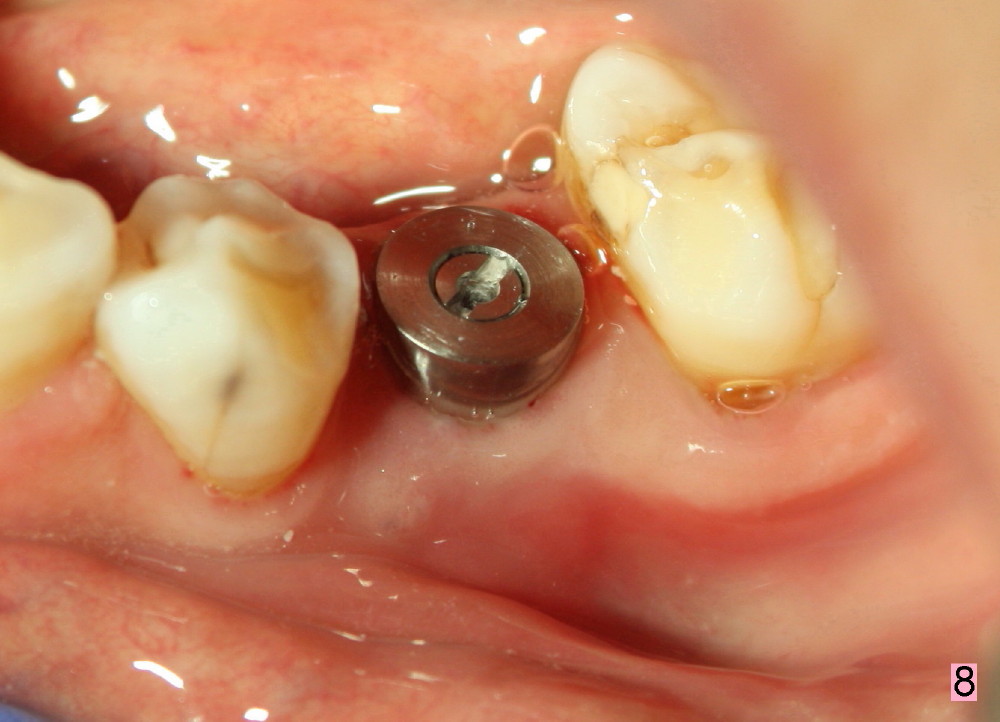
Taking multiple intraop X-ray is also necessary for depth adjustment (Fig.3-5). For example, when a 5x20 mm tap is inserted at the depth of 17 mm, it is close to the mental loop (Fig.4), whereas the binding to the bone is minimal. So a larger implant is to be placed at a shallower depth (Fig.5: 6x17 mm with insertion torque >60 Ncm). The shallower implant placement creates limited space for future abutment and crown (Fig.6,7). A short abutment will be used and the implant margin will be prepared as low as possible. As expected, the wound heals in a week (Fig.8).
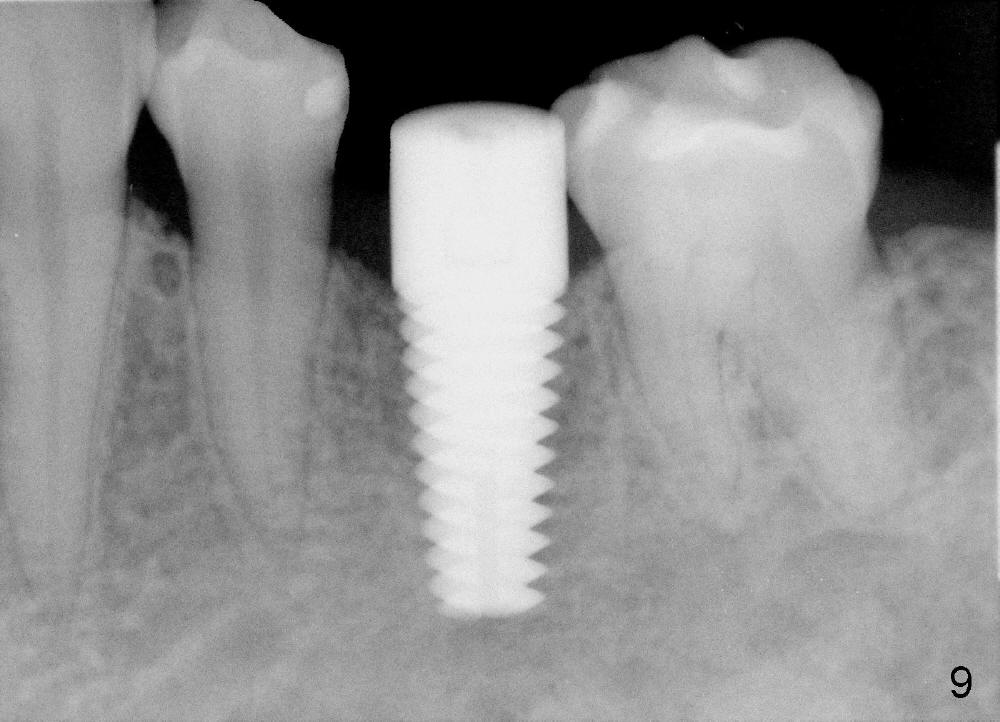
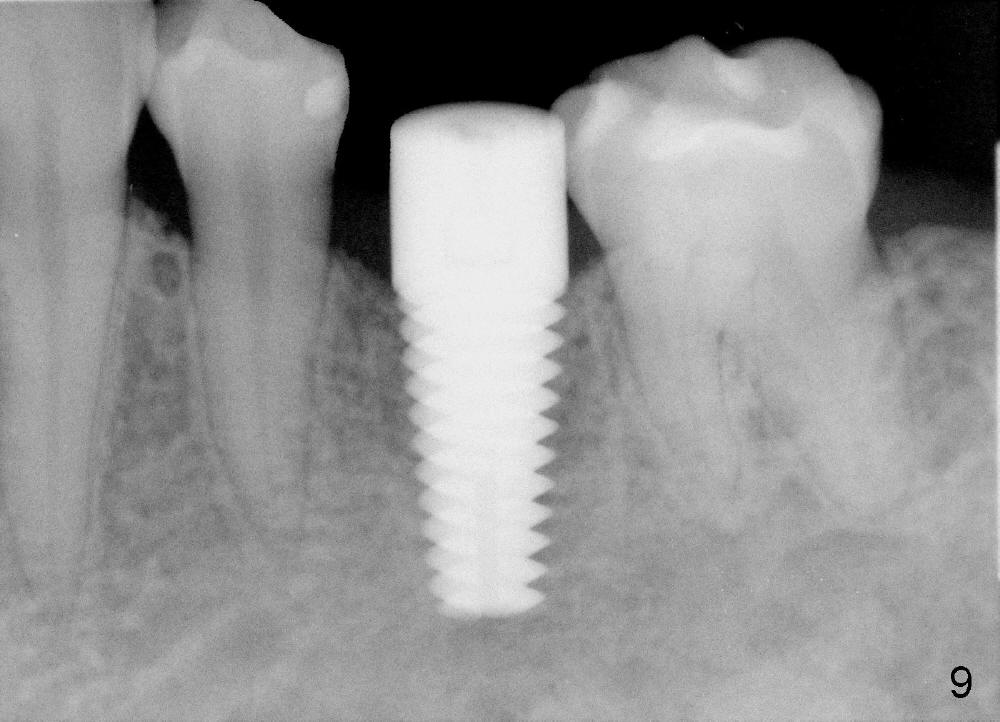
Six months postop, bone density around the implant increases (Fig.9). There is slight gingival recession buccal to the implant (Fig.10 arrow). A short abutment is placed and prepared short (Fig.11 A); the margin is prepared as low as possible in the implant (I).
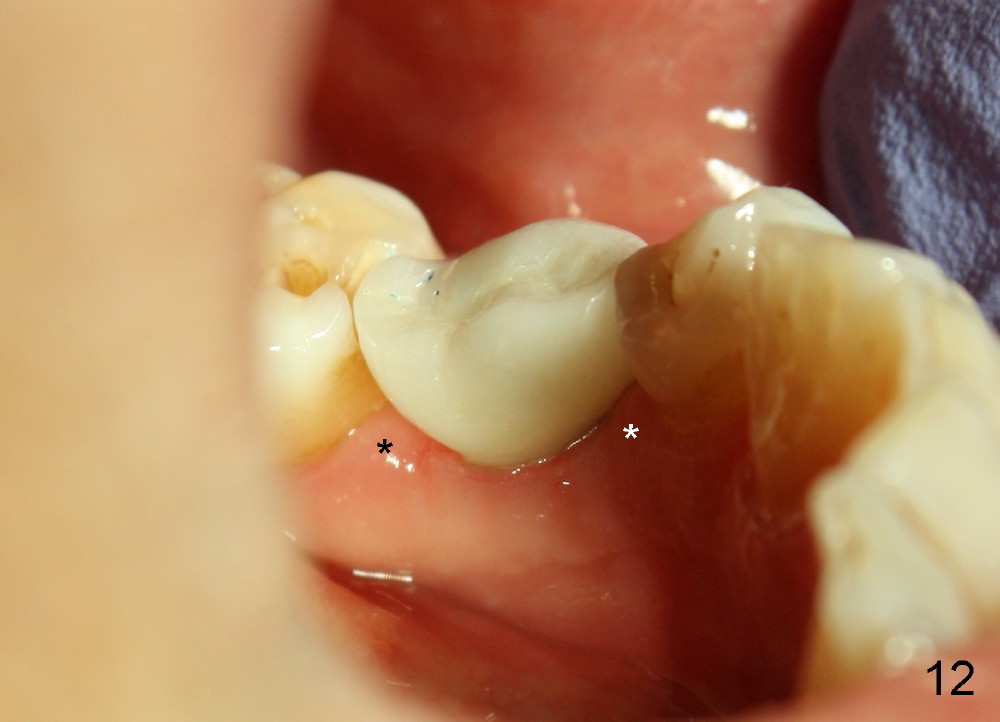
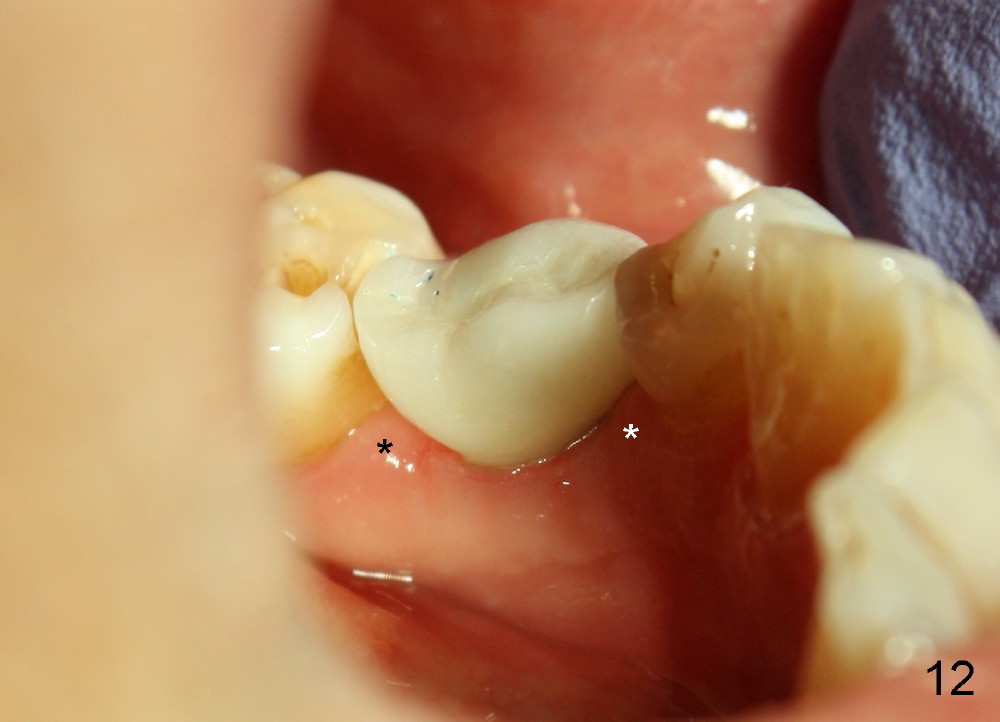
When the crown is bonded, the papillae (*) look basically normal lingually (Fig.12) and buccally (Fig.13).
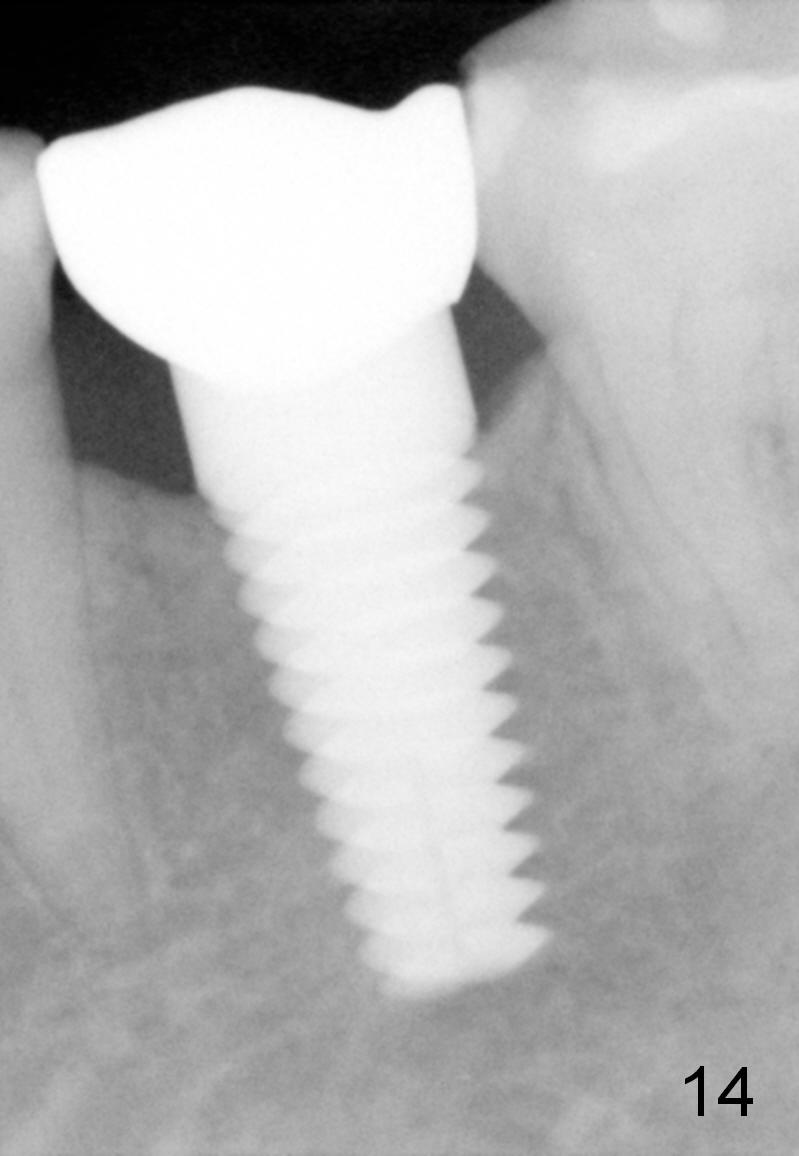
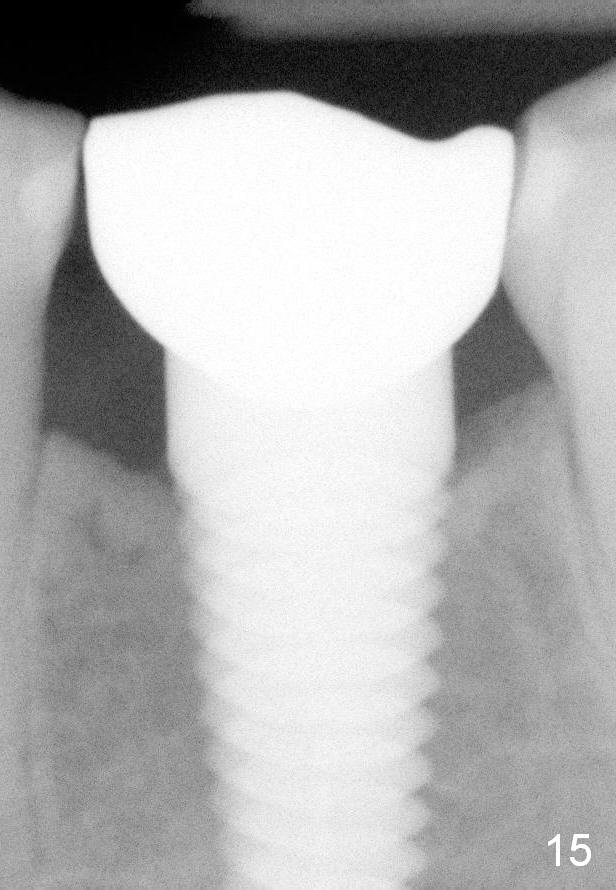
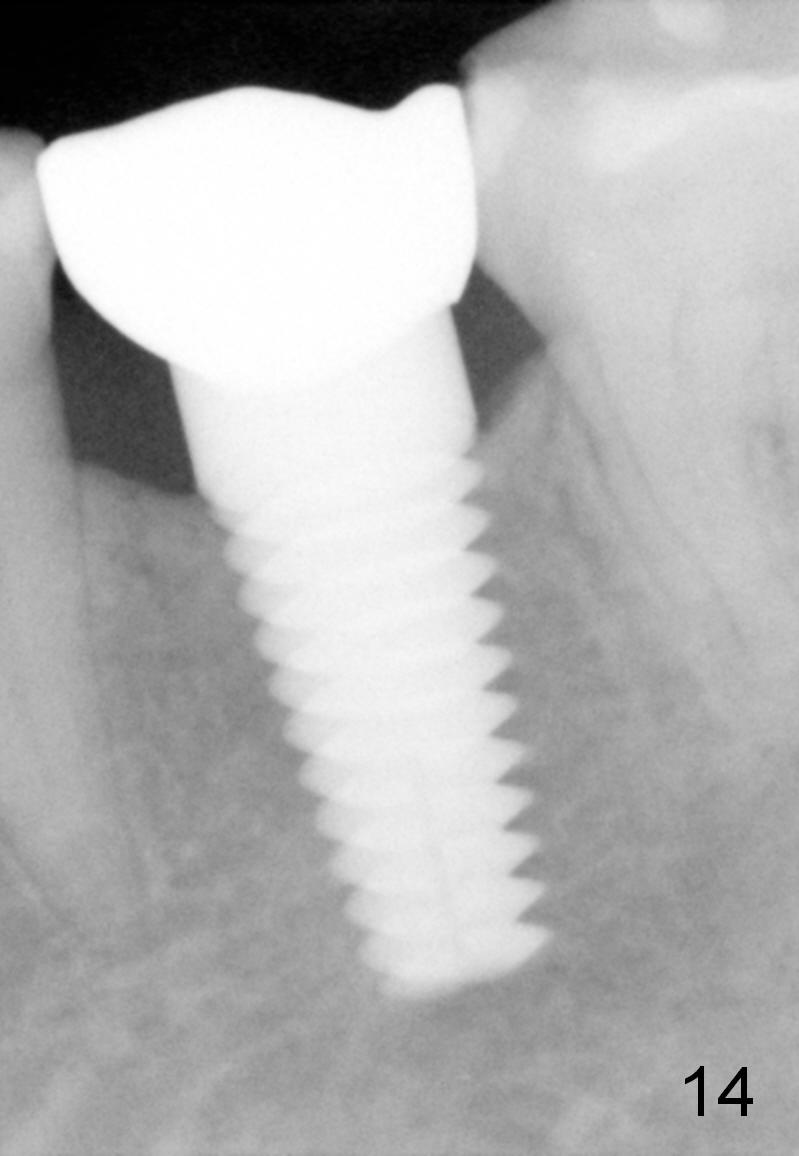
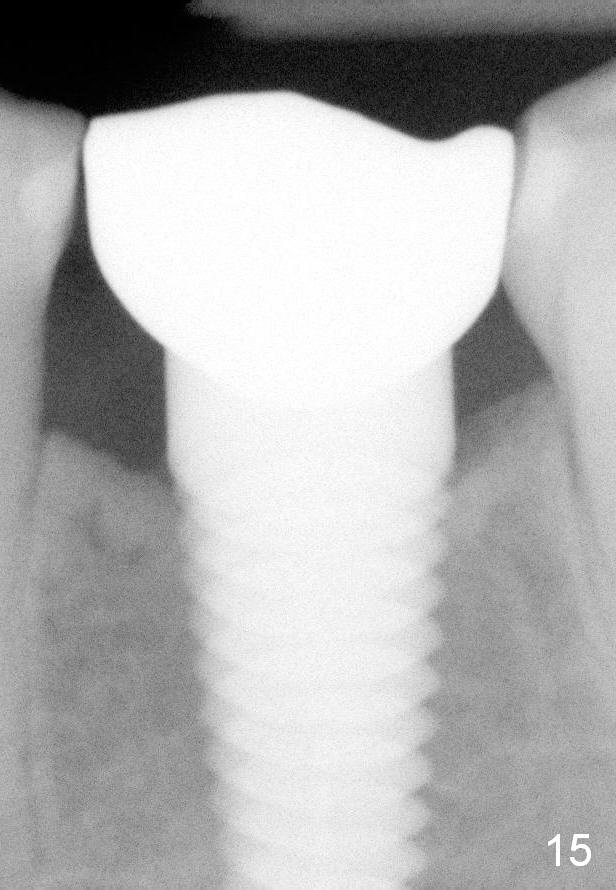
Eleven months post bonding (17 months postop), there is cortical bone formation at the mesial and distal crests (Fig.14). It remains the same 1 year 10 months post bonding (Fig.15). There is no bone loss 3 years 5 months post cementation (Fig.16). In fact the crestal cortical bone thickens.
Return to Lower Bicuspid Immediate Implant, 28/29, 30
Xin Wei, DDS, PhD, MS 1st edition 05/18/2014, last revision 04/04/2018