
 |
 |
 |
 |
|
 |
 |
 |
 |
|
Septum Placement of Immediate Implant
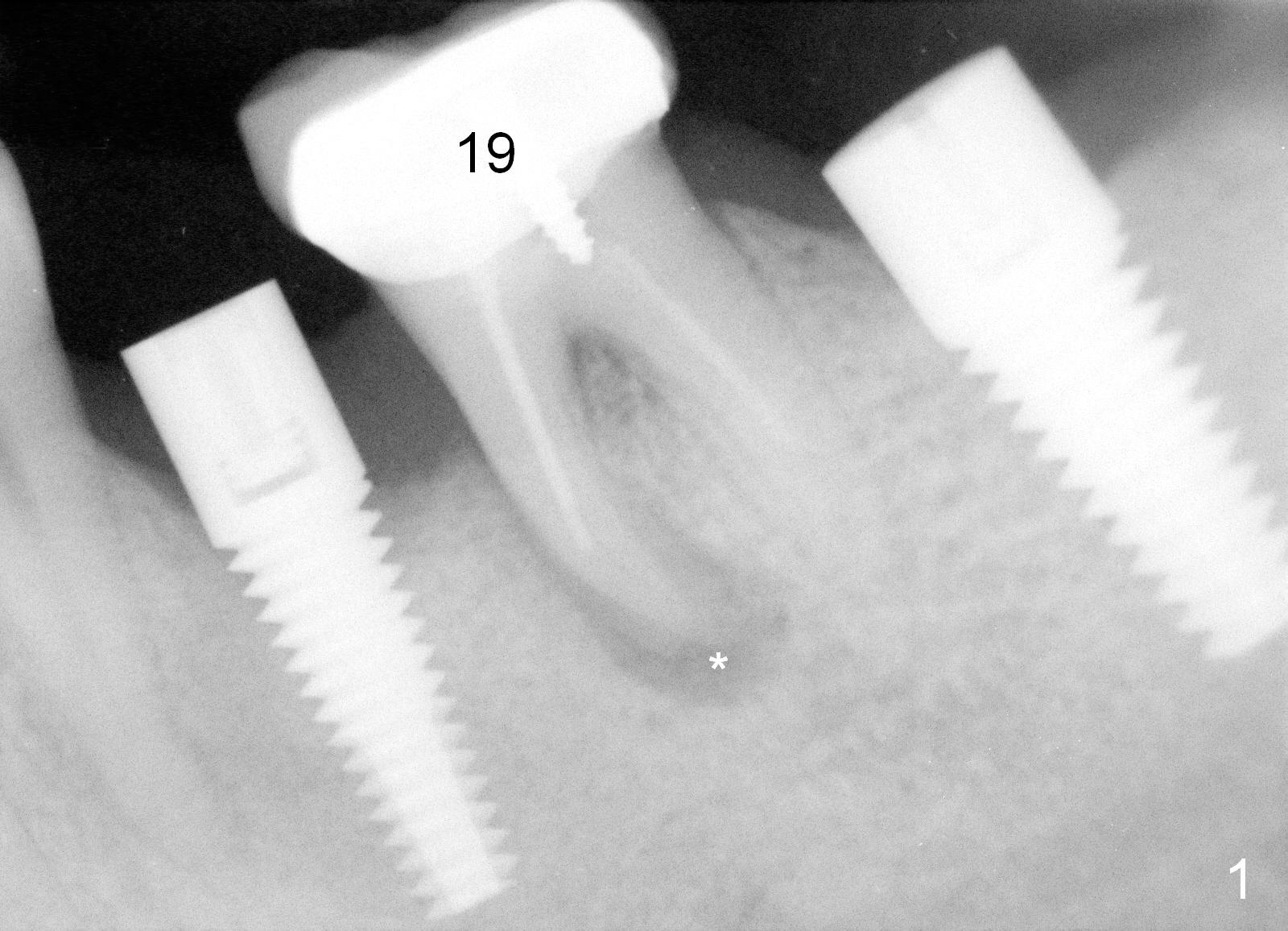
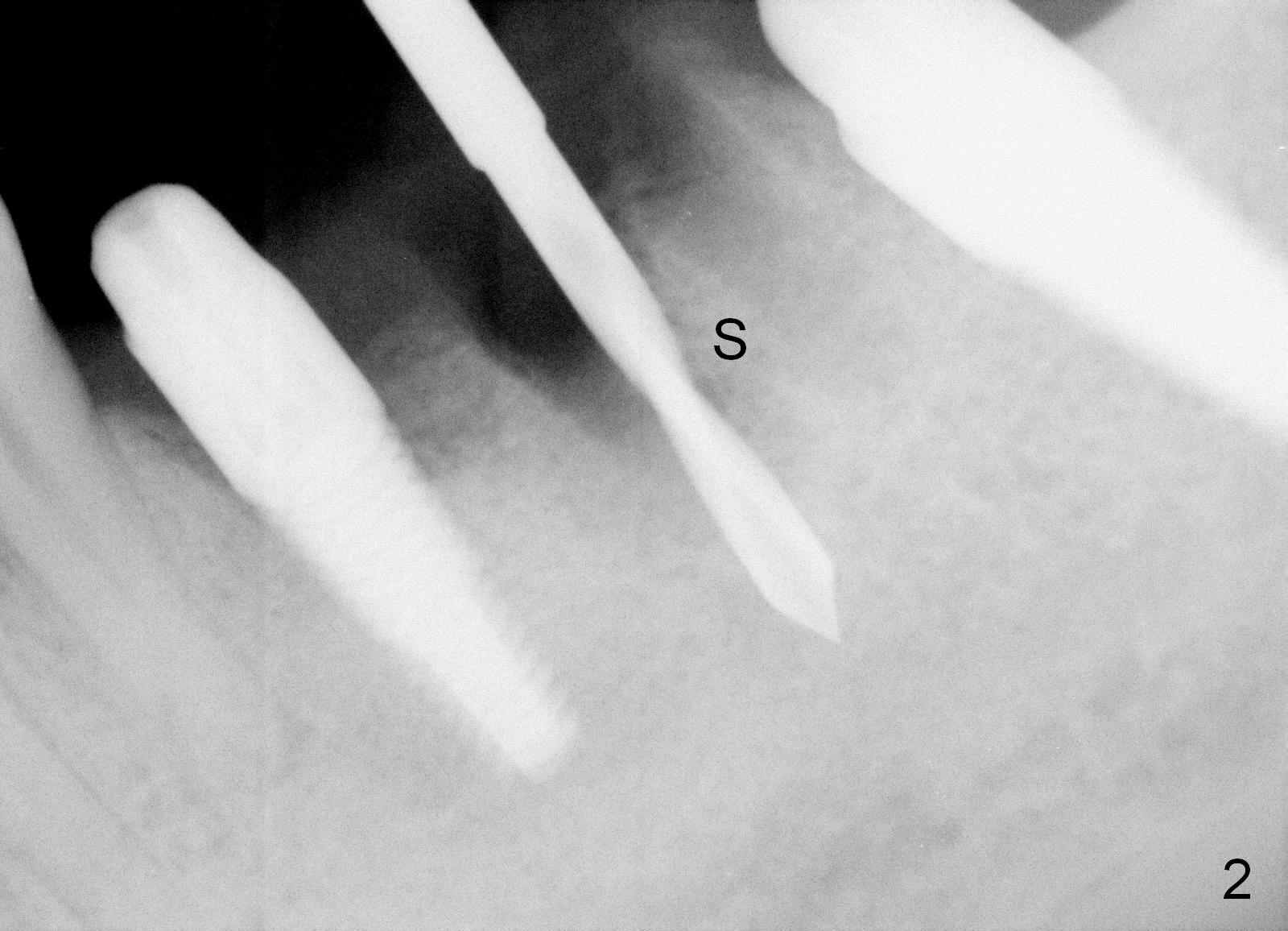
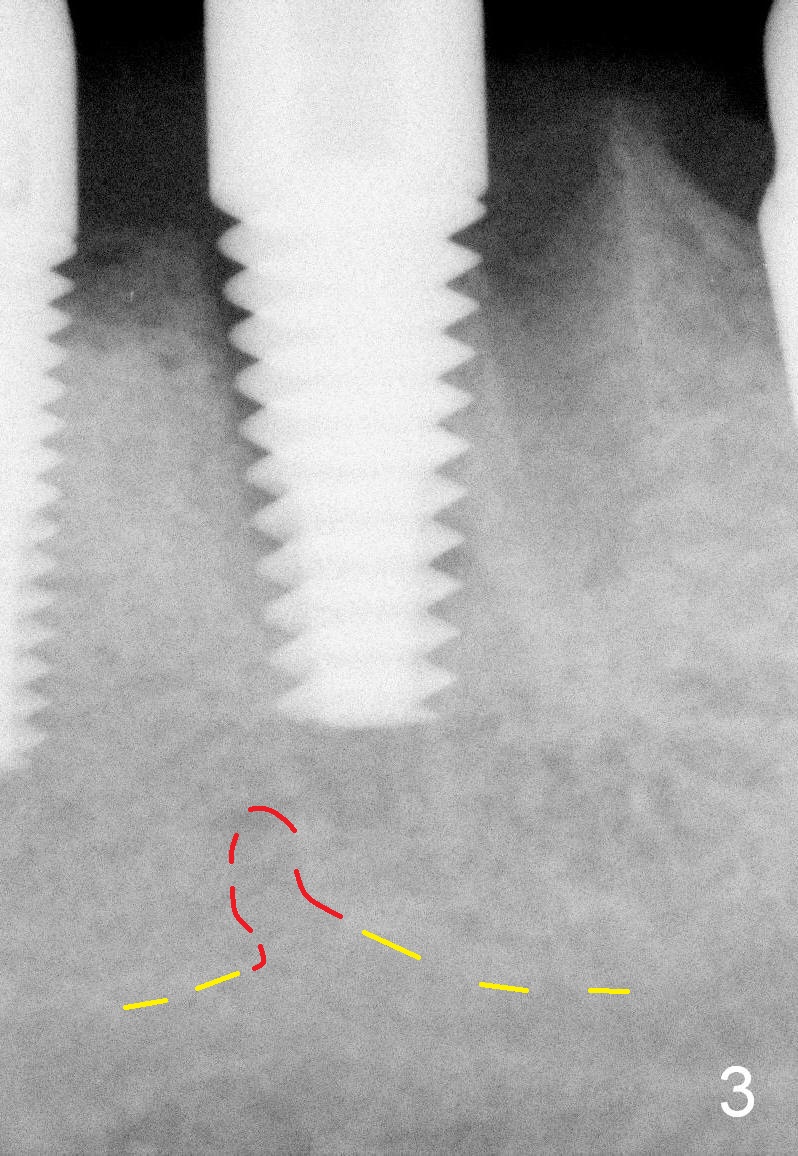
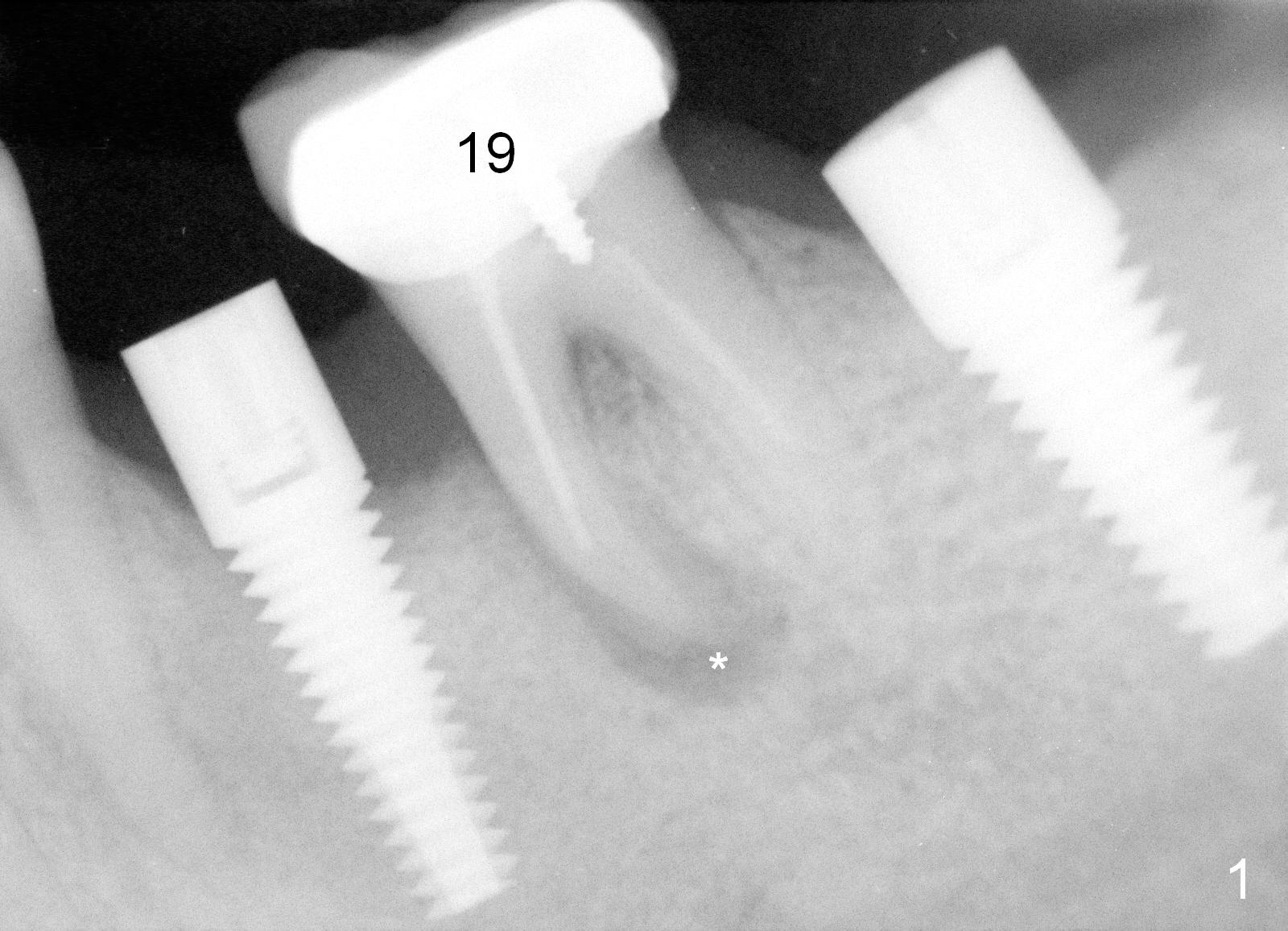
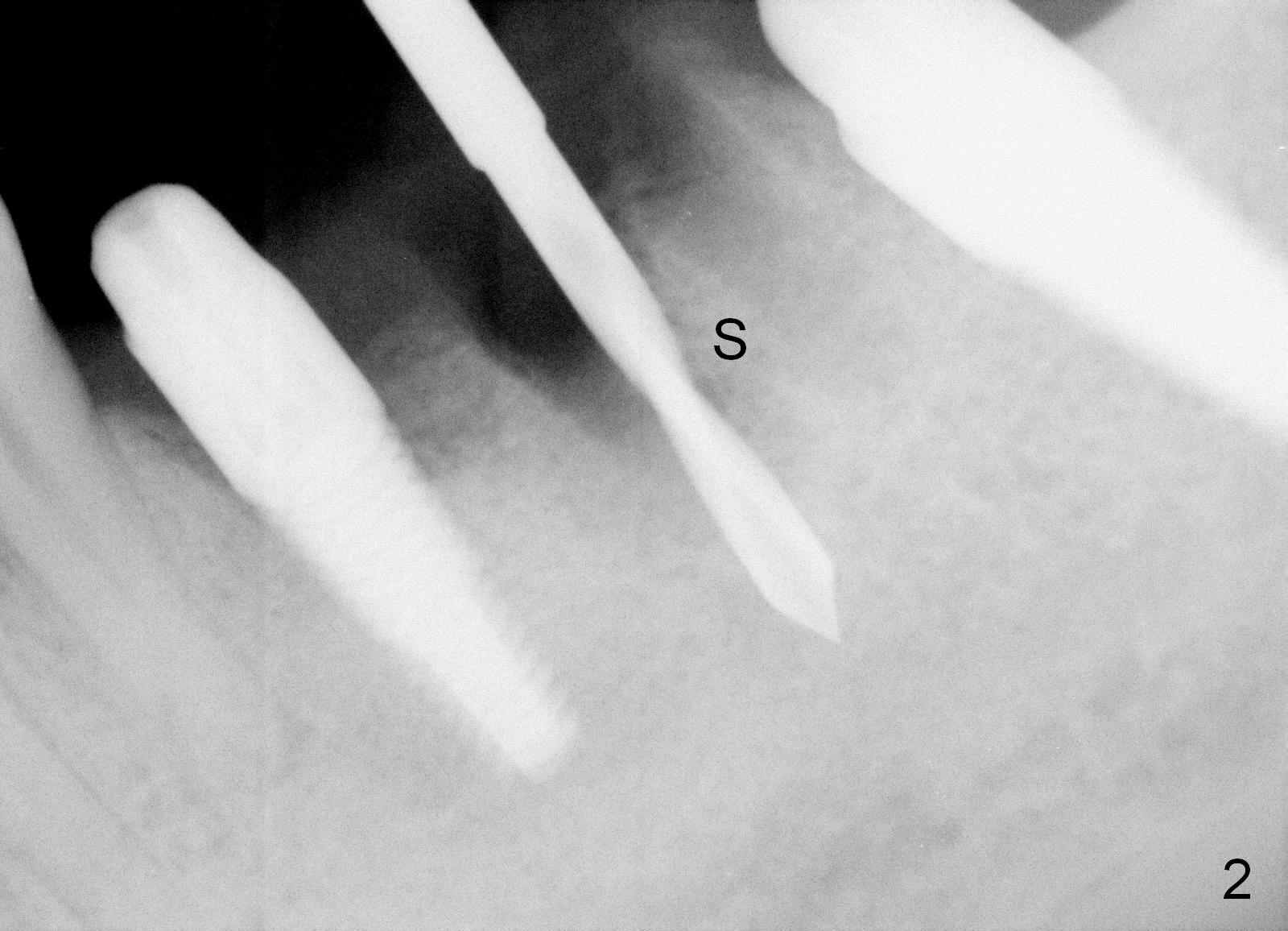
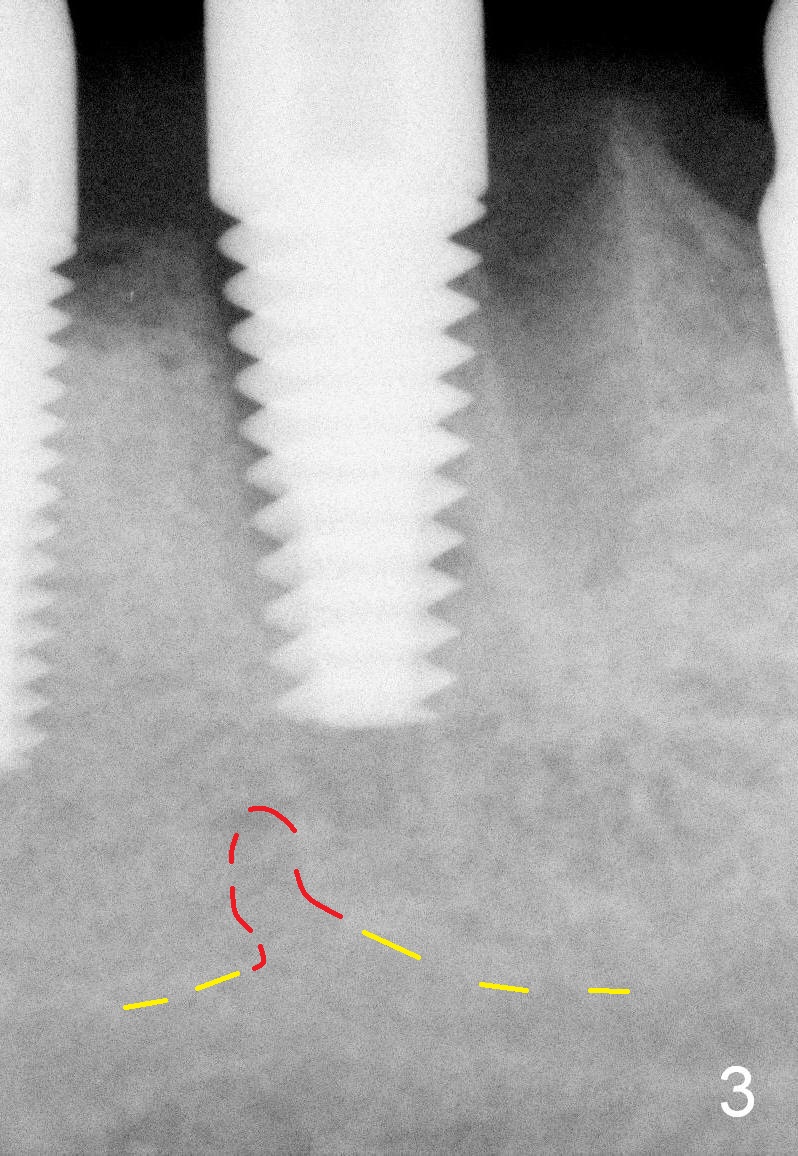
When the infection at the site of #20 is under control, the tooth #19 causes severe pain with mesial periapical radiolucency (Fig.1 *). Vertical mesial root fracture is confirmed at extraction. Osteotomy is initiated in the septum (Fig.2 S), but the apical end of the 2 mm pilot drill deviates to the mesial socket. A Lindamann bur is used to move osteotomy distal, but the implant (6x17 mm) is mainly placed in the mesial socket (Fig.3). An intraop drawback associated with the deviation is pain control. The nervous patient questions several times whether it is a good idea to place an implant in the infected site. Block anesthesia has to be administered. In fact lack of pain control may be also related to proximity to the Mental Loop (Fig.3 red dashed line). Fortunately no paresthesia occurs postop, since the implant is somehow placed lingually.
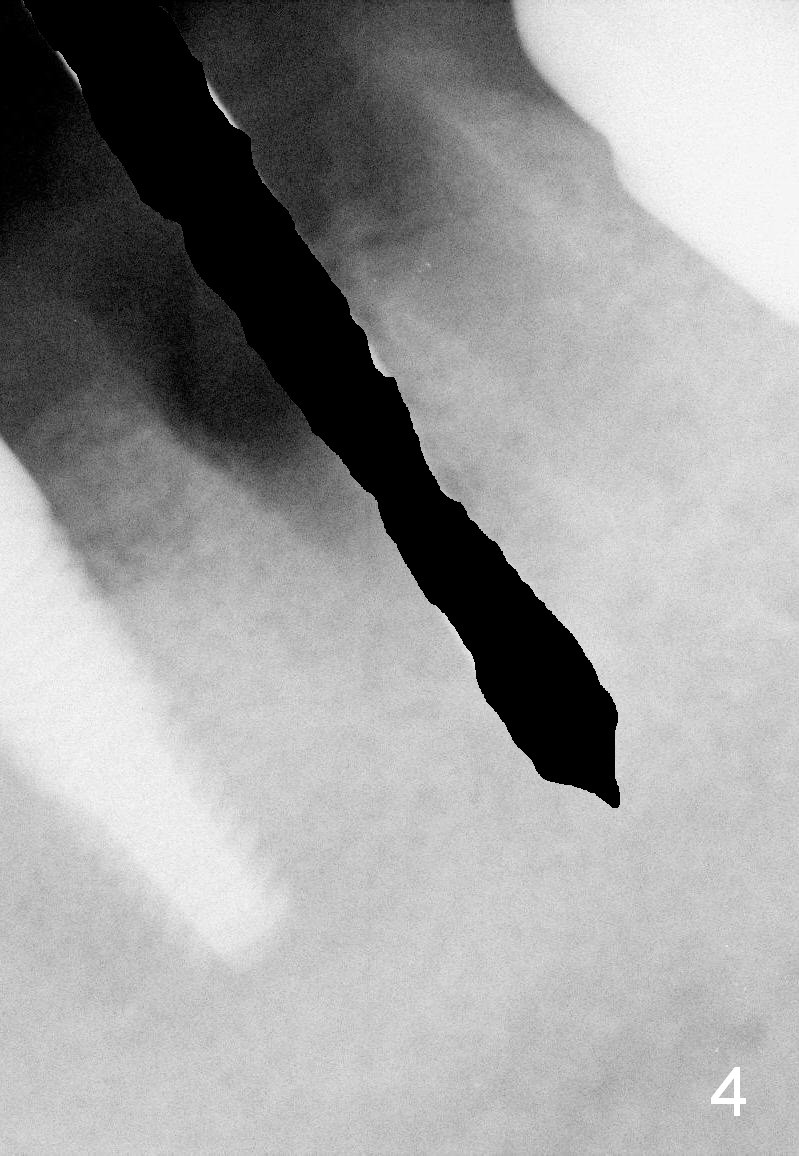
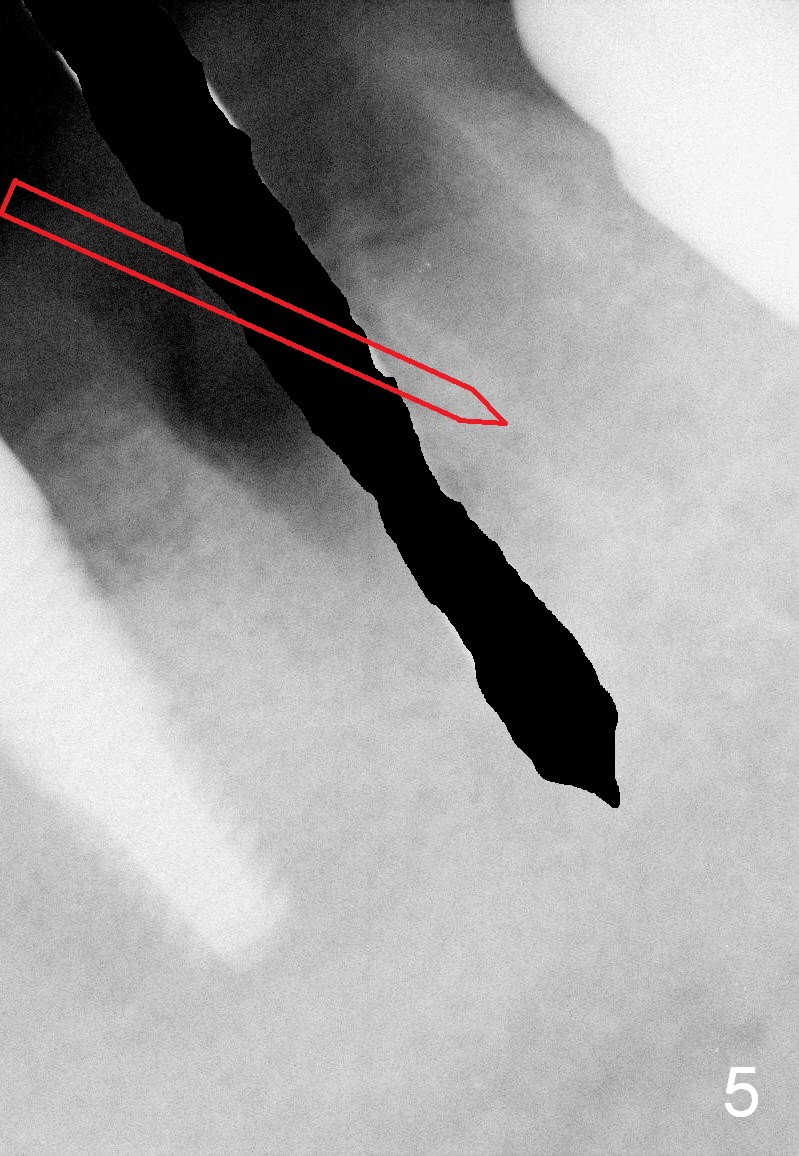
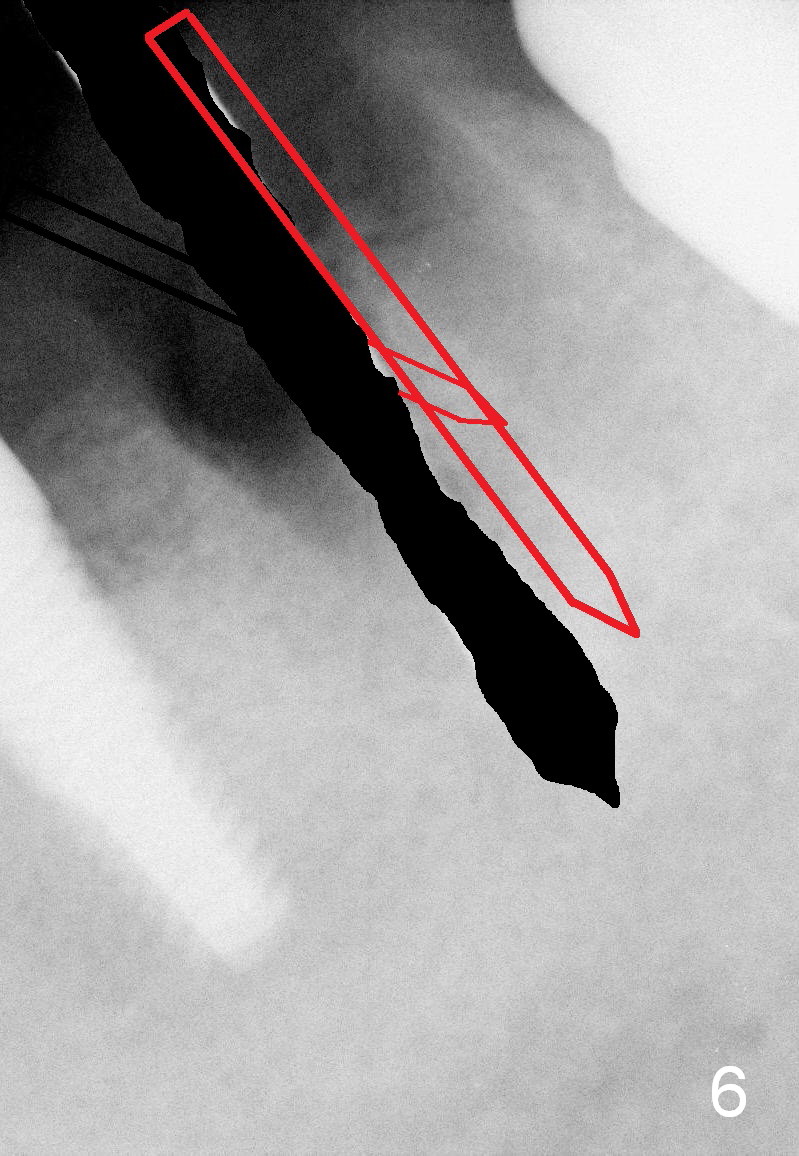
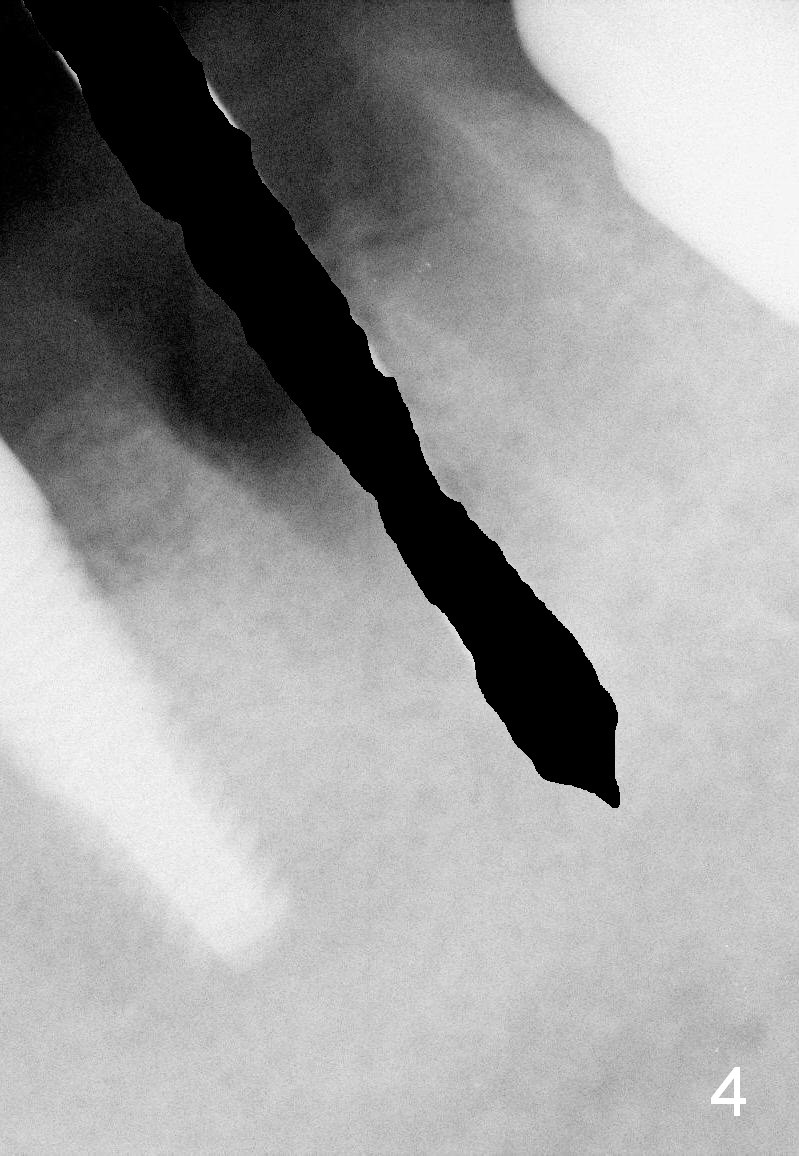
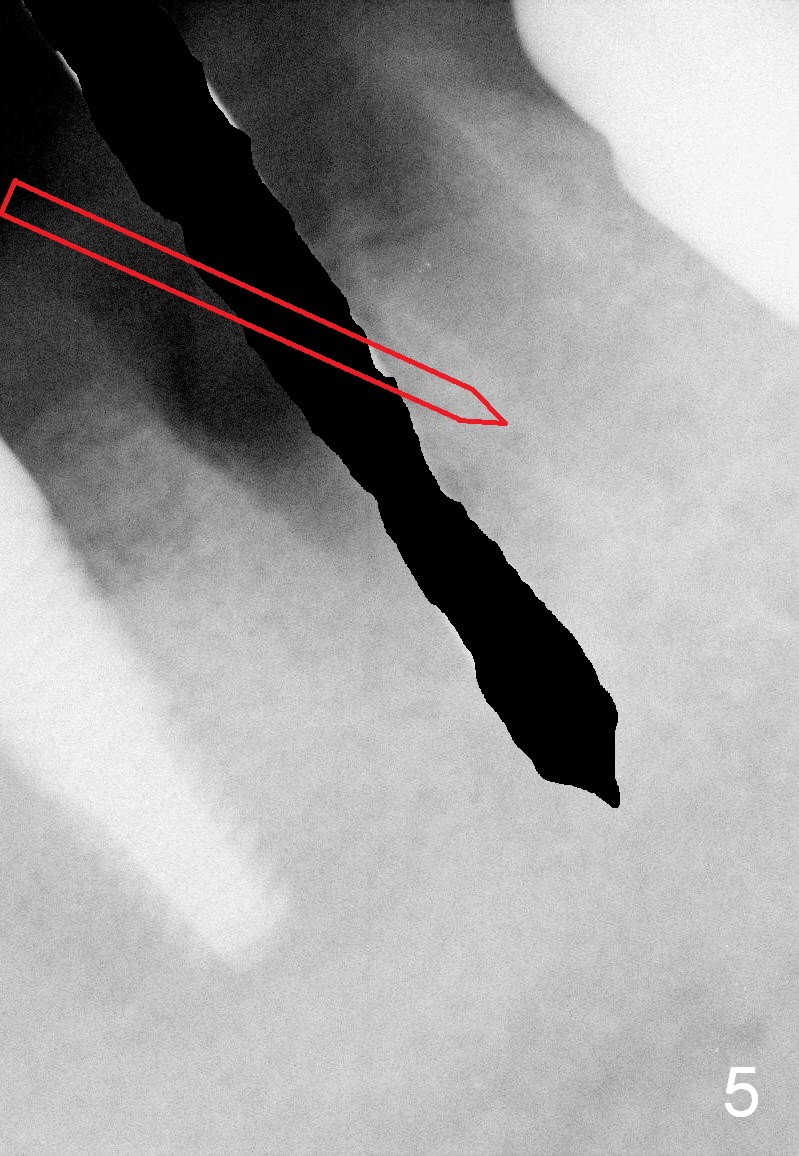
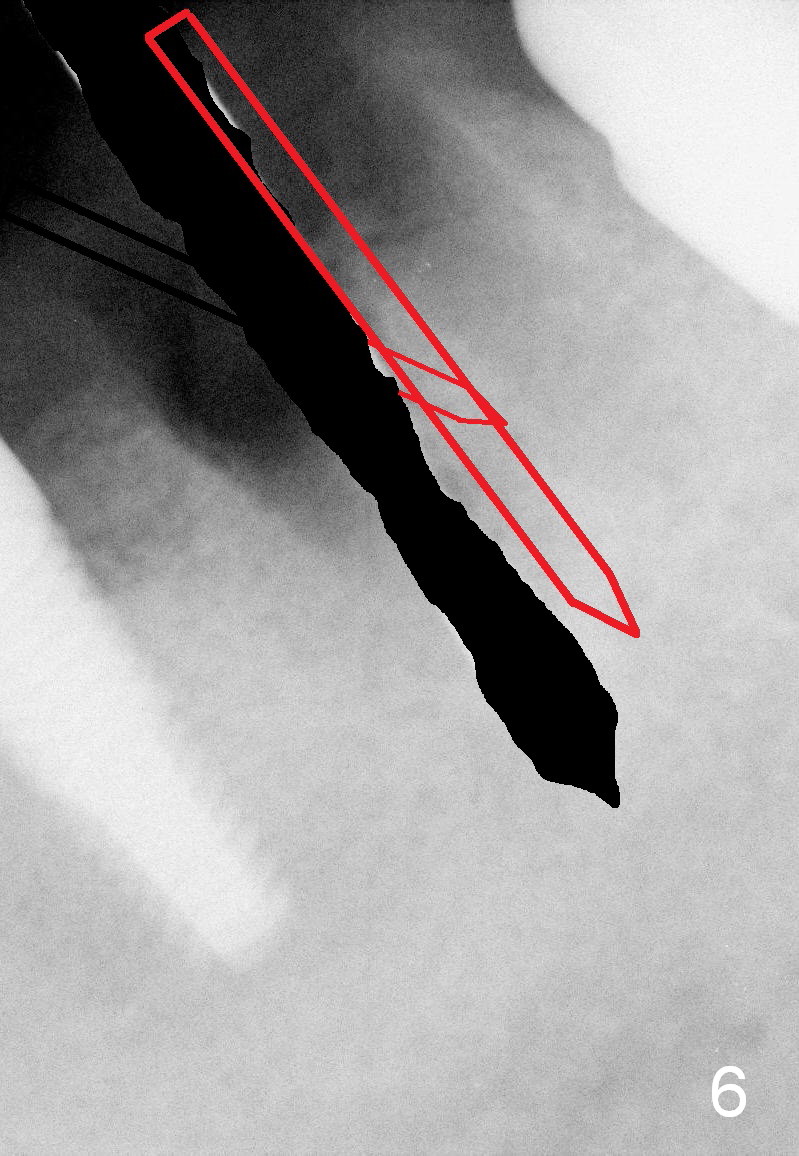
Implant placement in the distal socket is associated with poor restoration. To place the implant in the septum for this case, it would be the best to find a new entrance point in the septum oblique (Fig.5) after removal of the earlier drill (Fig.4). Once the entrance point is deep enough, the drill changes its axis and continues osteotomy (Fig.6 thicker red lines).
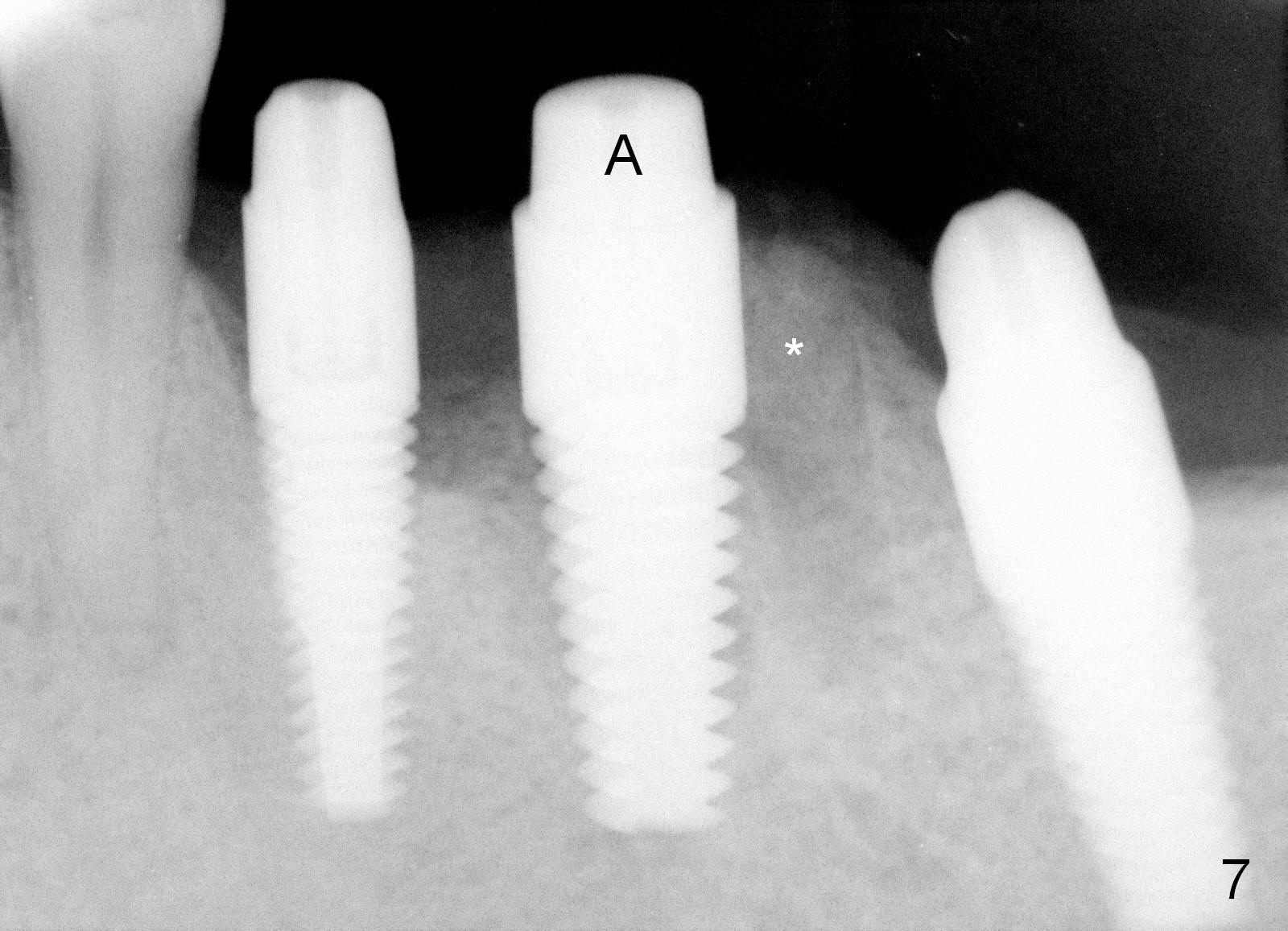
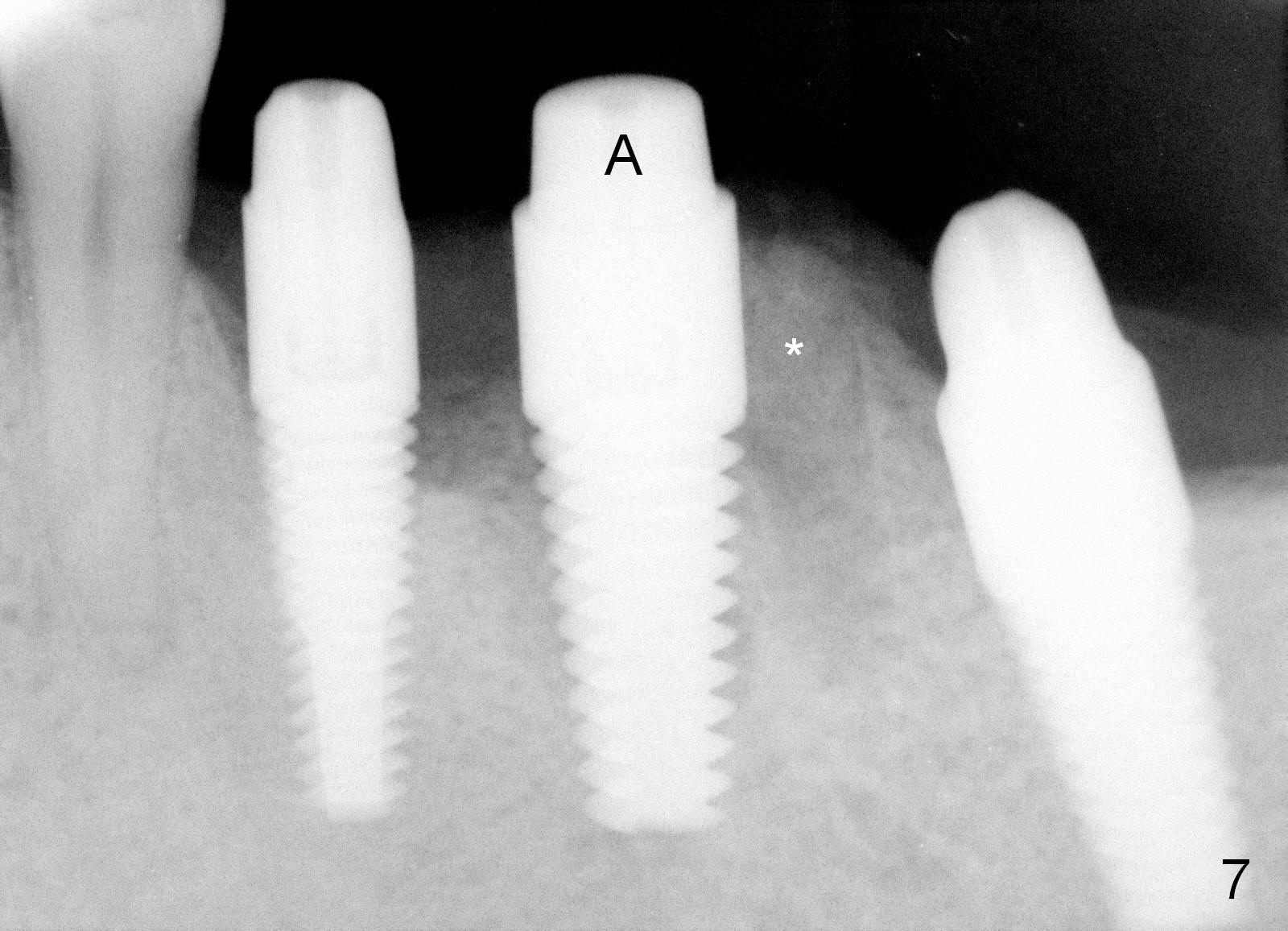
After placing the implant a little deeper, bone graft is placed in the distal socket (Fig.7 *). Three abutments are placed (A) in the 3 adjacent implants. Perio dressing is applied around these abutments to close the remaining gaps of #19 sockets.
Seven days postop, there is swelling distobuccal to the implant at the site of #19 (Fig.8) with minimal tenderness. One week later, there is no tenderness. The swelling may be due to packing graft. An immediate/early provisional is fabricated from #18 to #20. The implants at the sites of #18 and 20 have osteointegrated.
Return to Lower Molar Immediate Implant,
Posterior Immediate Provisional,
Dr.
Wu
Xin Wei, DDS, PhD, MS 1st edition 04/19/2015, last revision 04/20/2015