.jpg)





 |
 |
 |
||
 |
 |
.jpg) |
||
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
 |
||||
Why Miss Nerve?
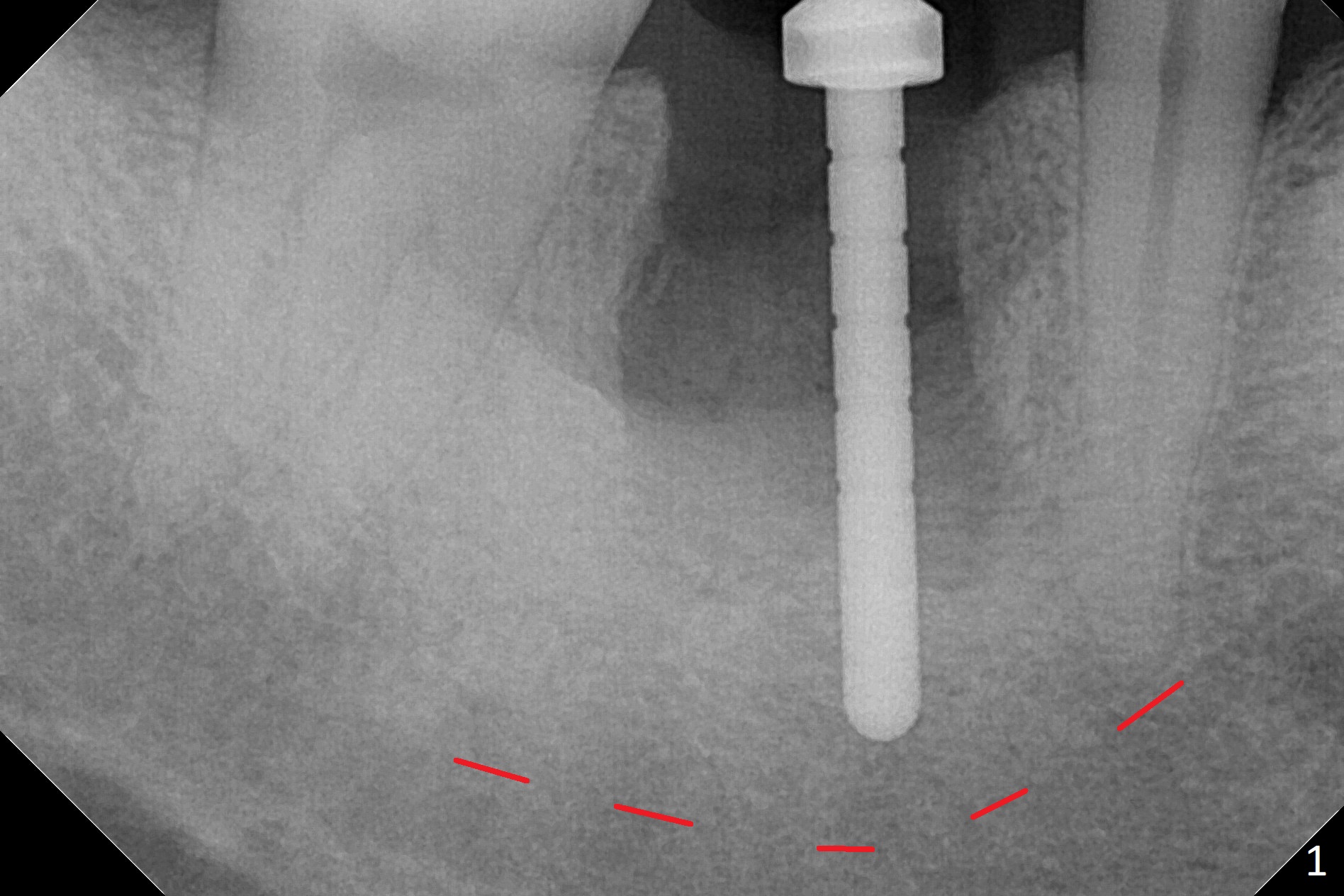
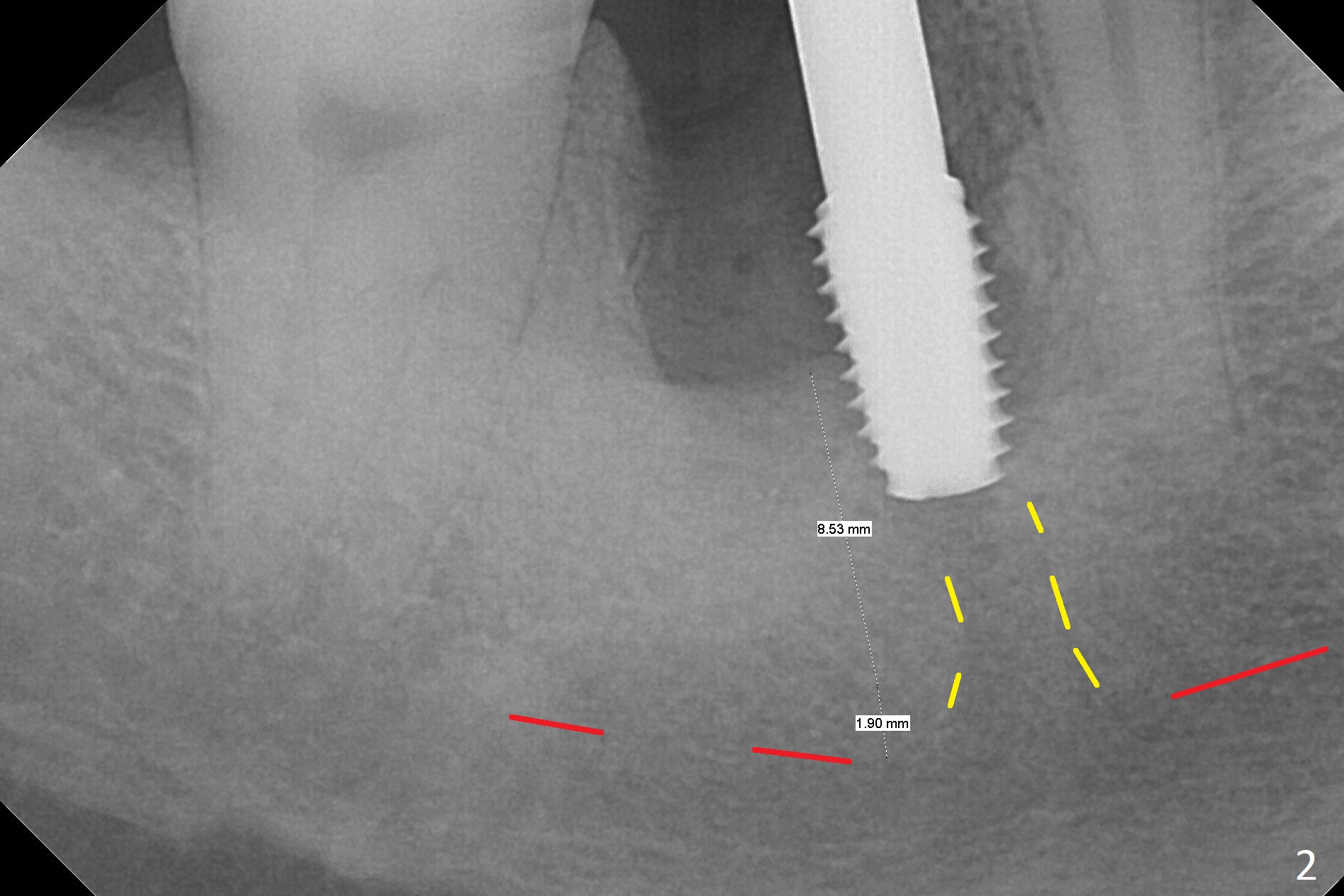
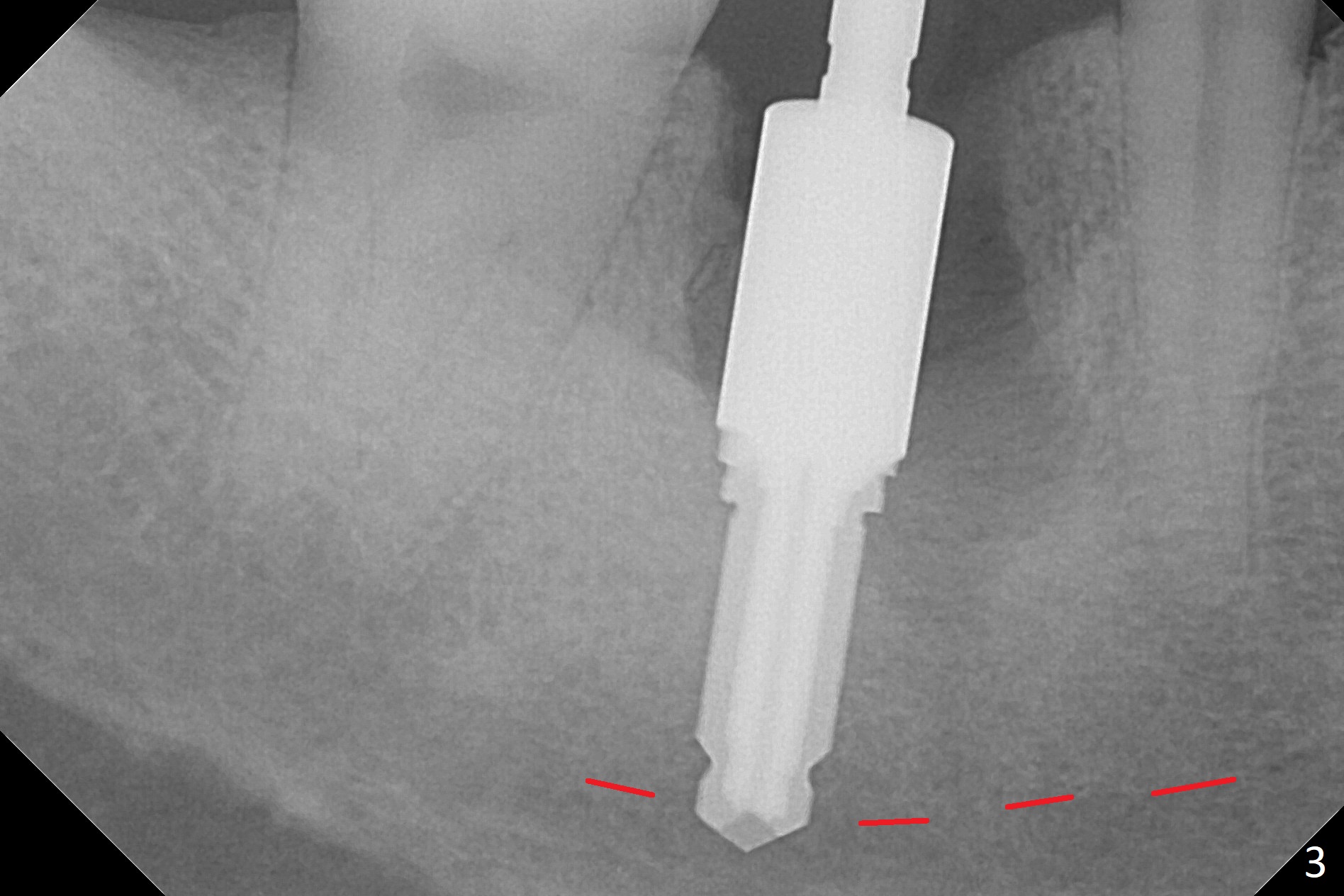
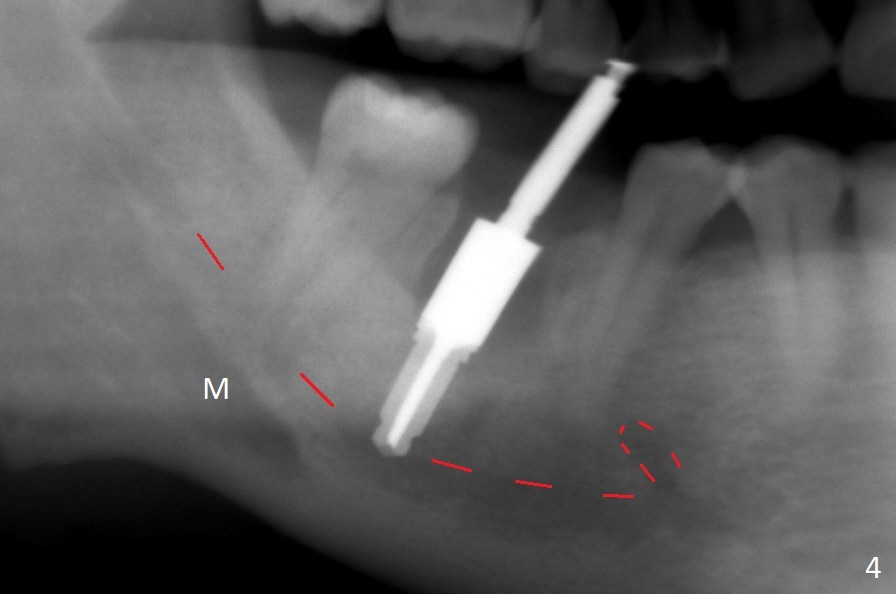
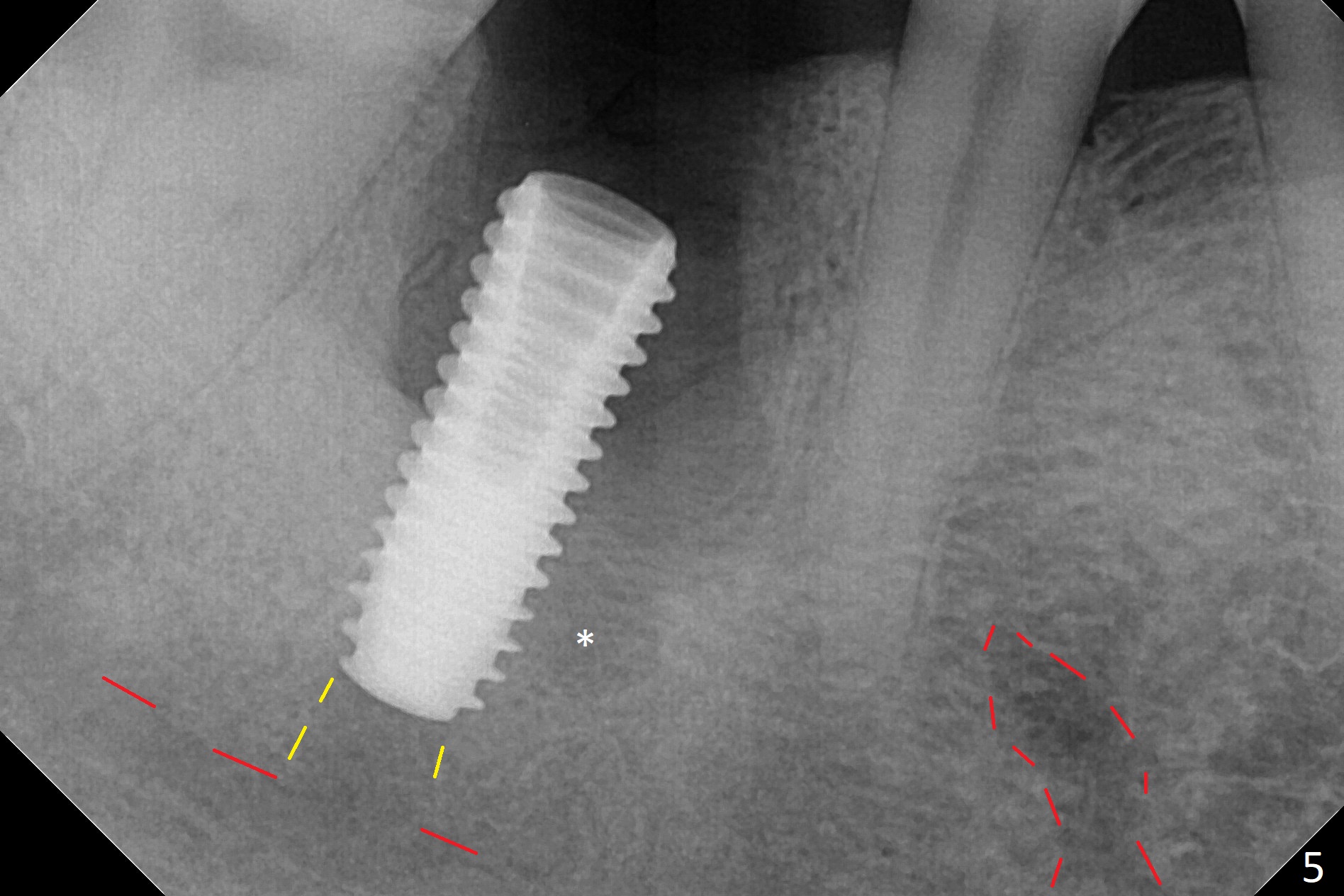
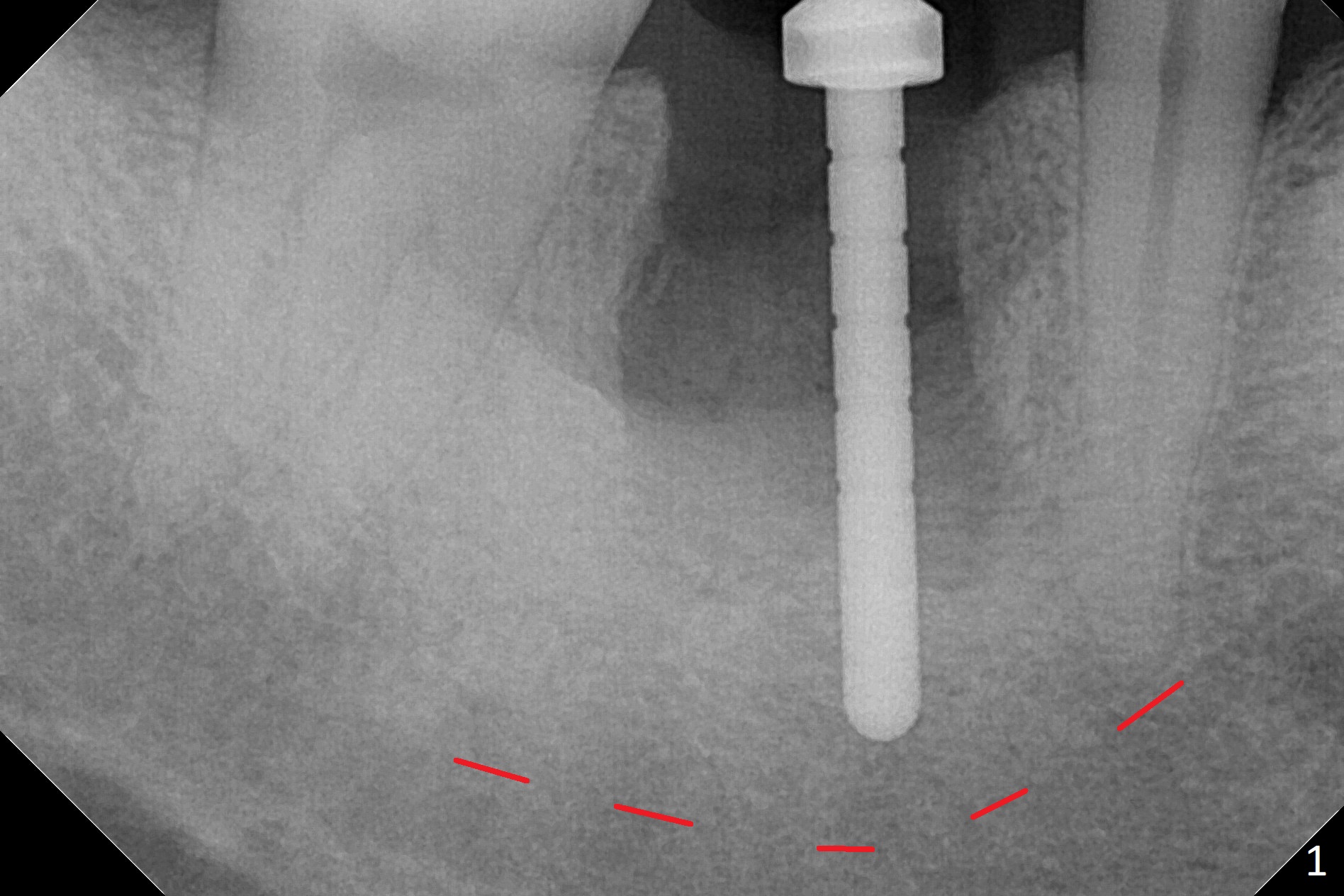
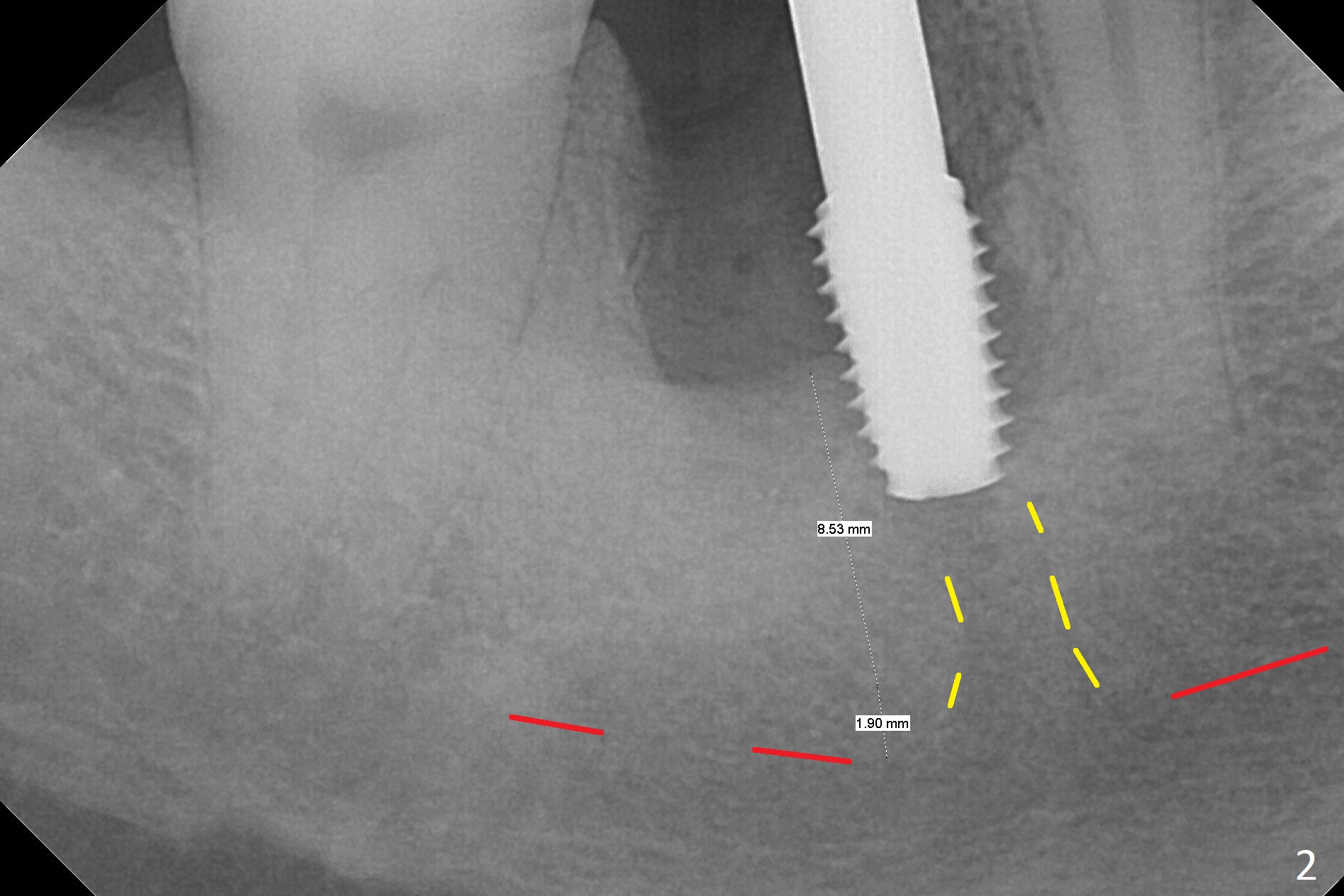
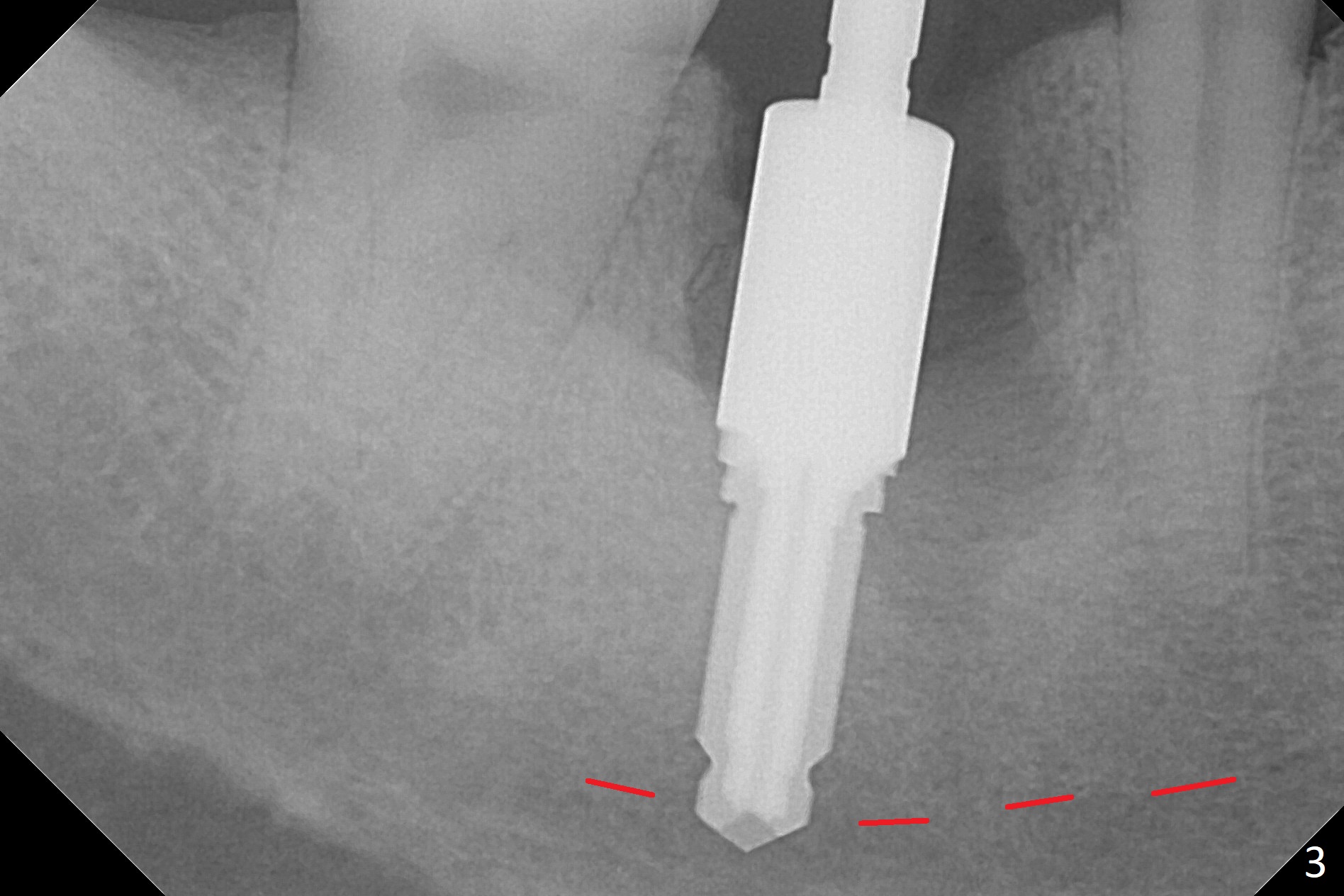
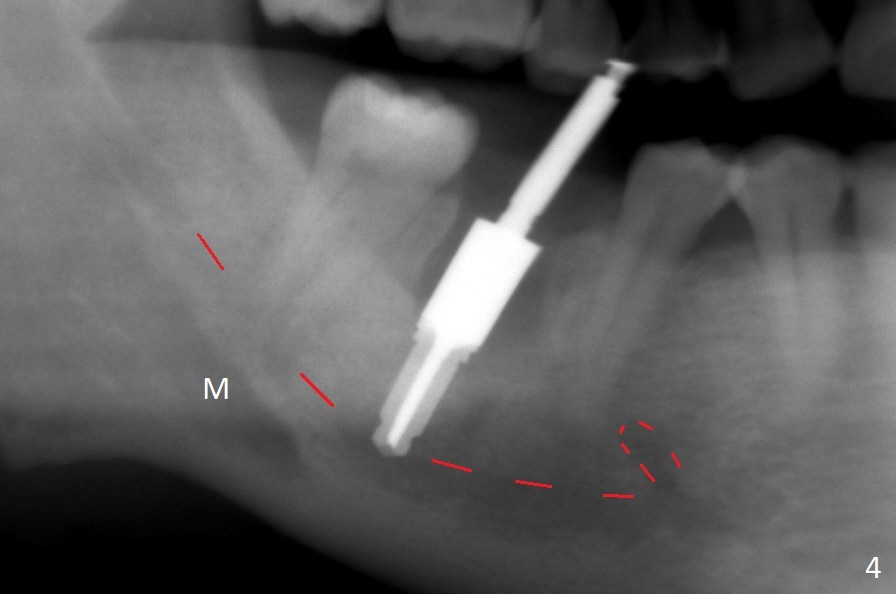
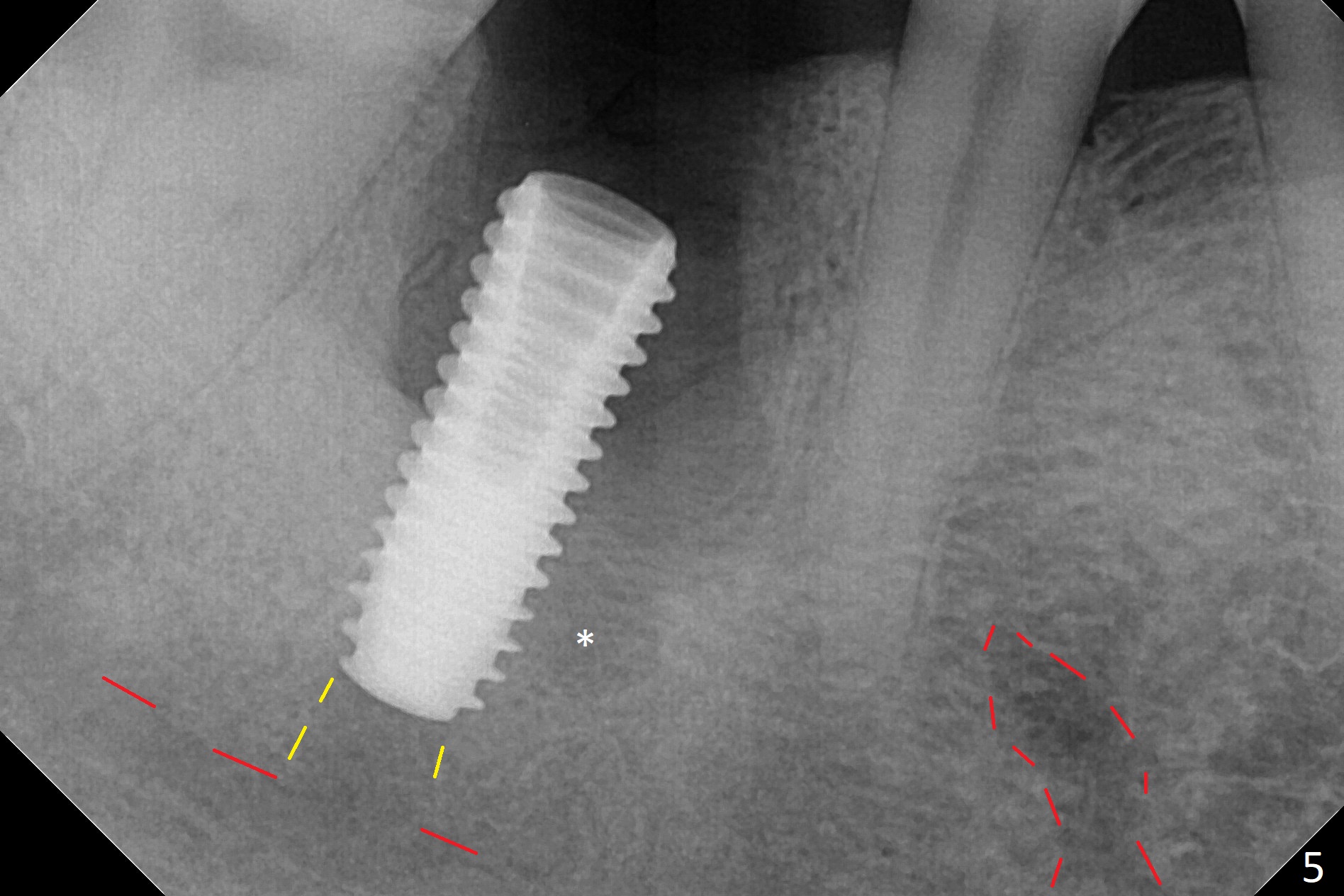
After the tooth #30 is extracted, the socket is 18 mm deep and the lingual plate is 4 mm tall. With hemorrhage, visibility of the socket, especially the bottom, is poor. The septum is almost completely defective. Following removal of the most buccal portion of the septum, osteotomy is initiated as buccal as possible, but it is mesial (Fig.1). In spite of effort to move the osteotomy distal, the osteotomy remains mesial and superficial (Fig.2 with 5 mm tap drill). Pain control is poor with infiltration. It appears that the smaller osteotomy (Fig.2 yellow line) may have extended close to the superior border of the Inferior Alveolar Canal (red line). It appears that there is 8.5 mm bone distal with ~ 2 mm clearance. After mandibular block, a new osteotomy is made distal; when a 3.8 mm drill is being used, there is hemorrhage from the osteotomy with apparent violation of the Canal integrity (Fig.3,4). But hemostasis is achieved with gauze pressure. A 5x13 mm implant is placed superficially (Fig.5) with a trace of the previous osteotomy (yellow line) and deep space created by the mesial osteotomy (*). Apparently the pathological and iatrogenic defects are filled with allograft (Fig.6 *). Guided surgery could have avoided the mesial osteotomy.
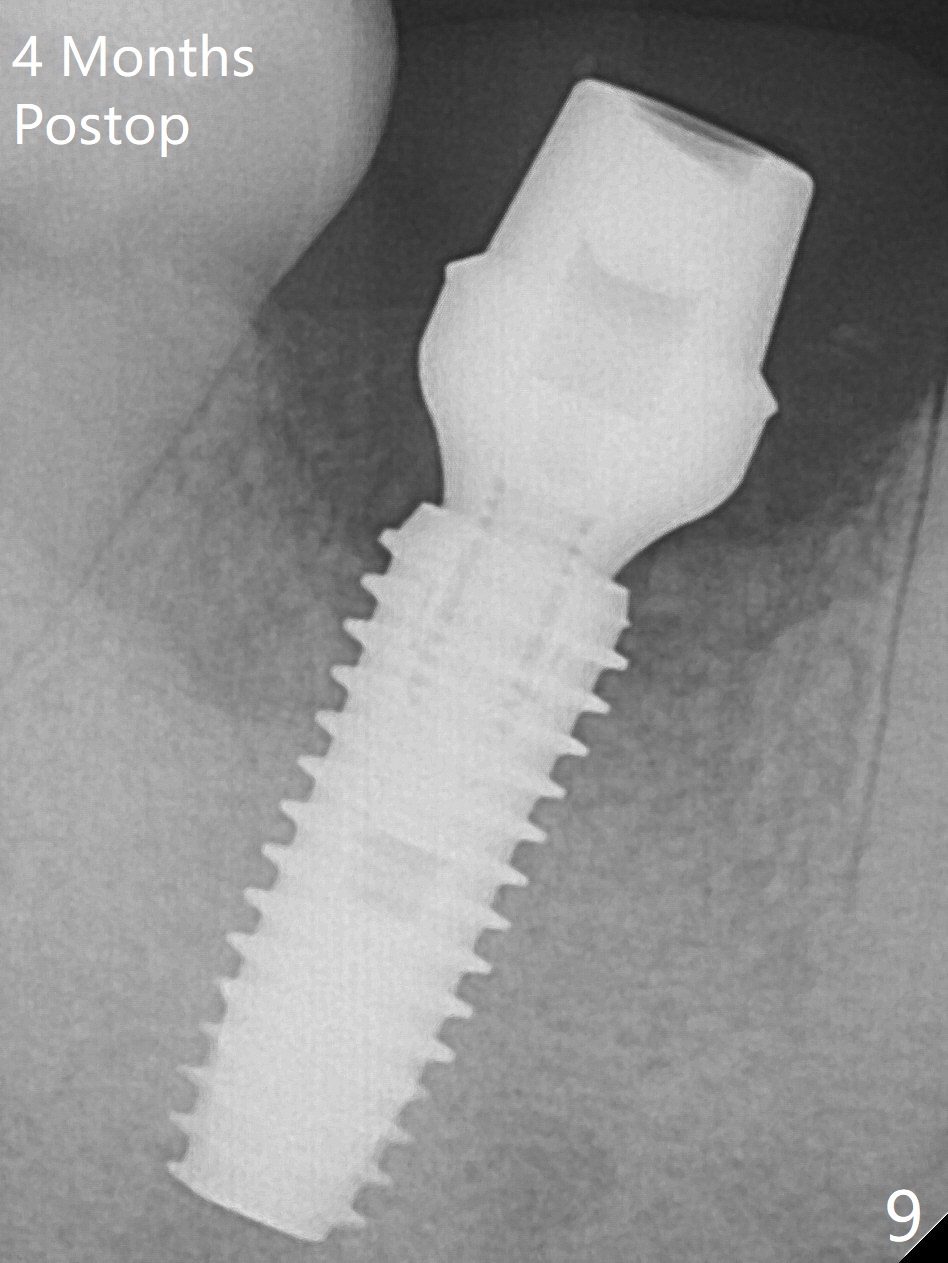
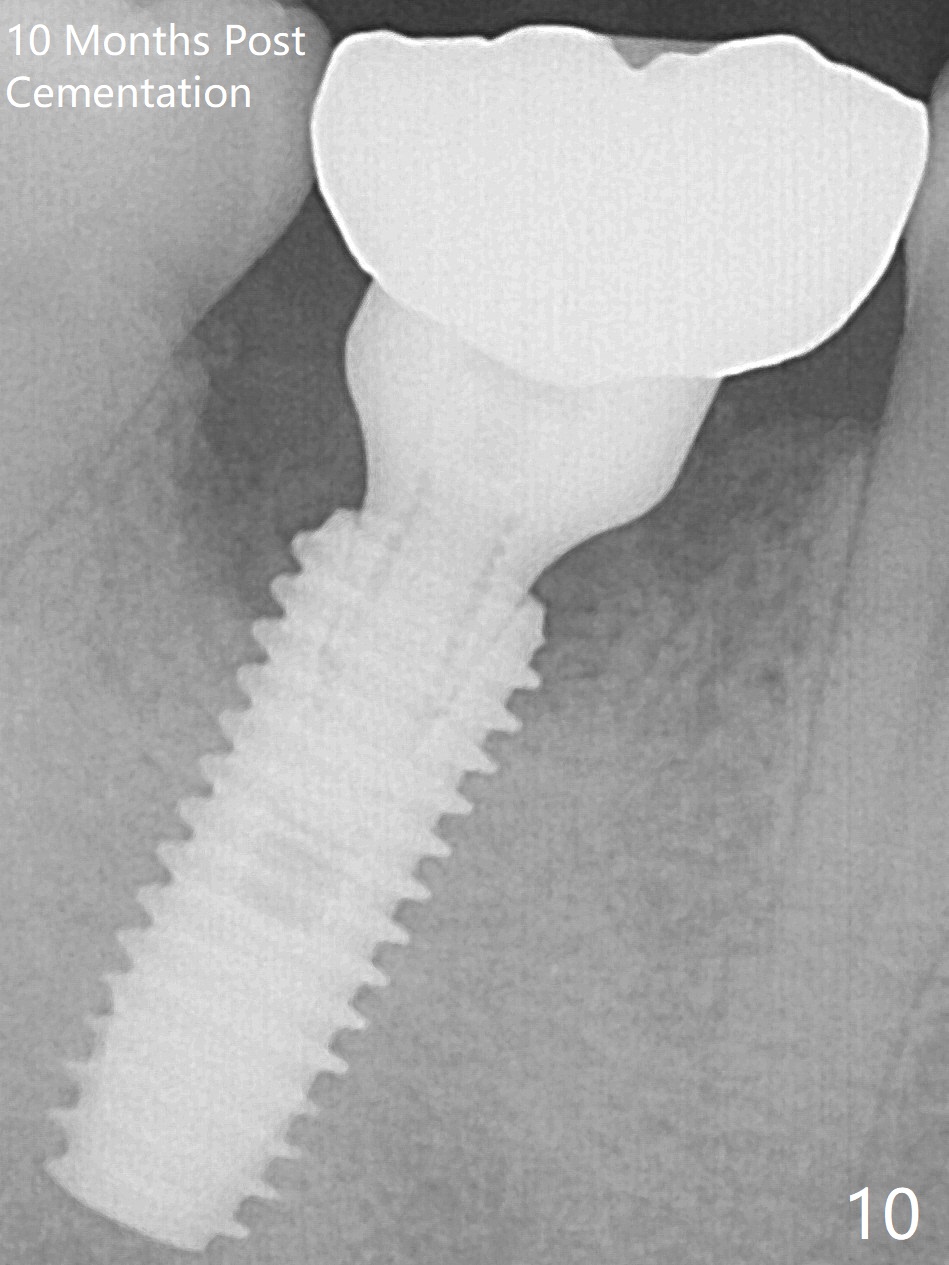
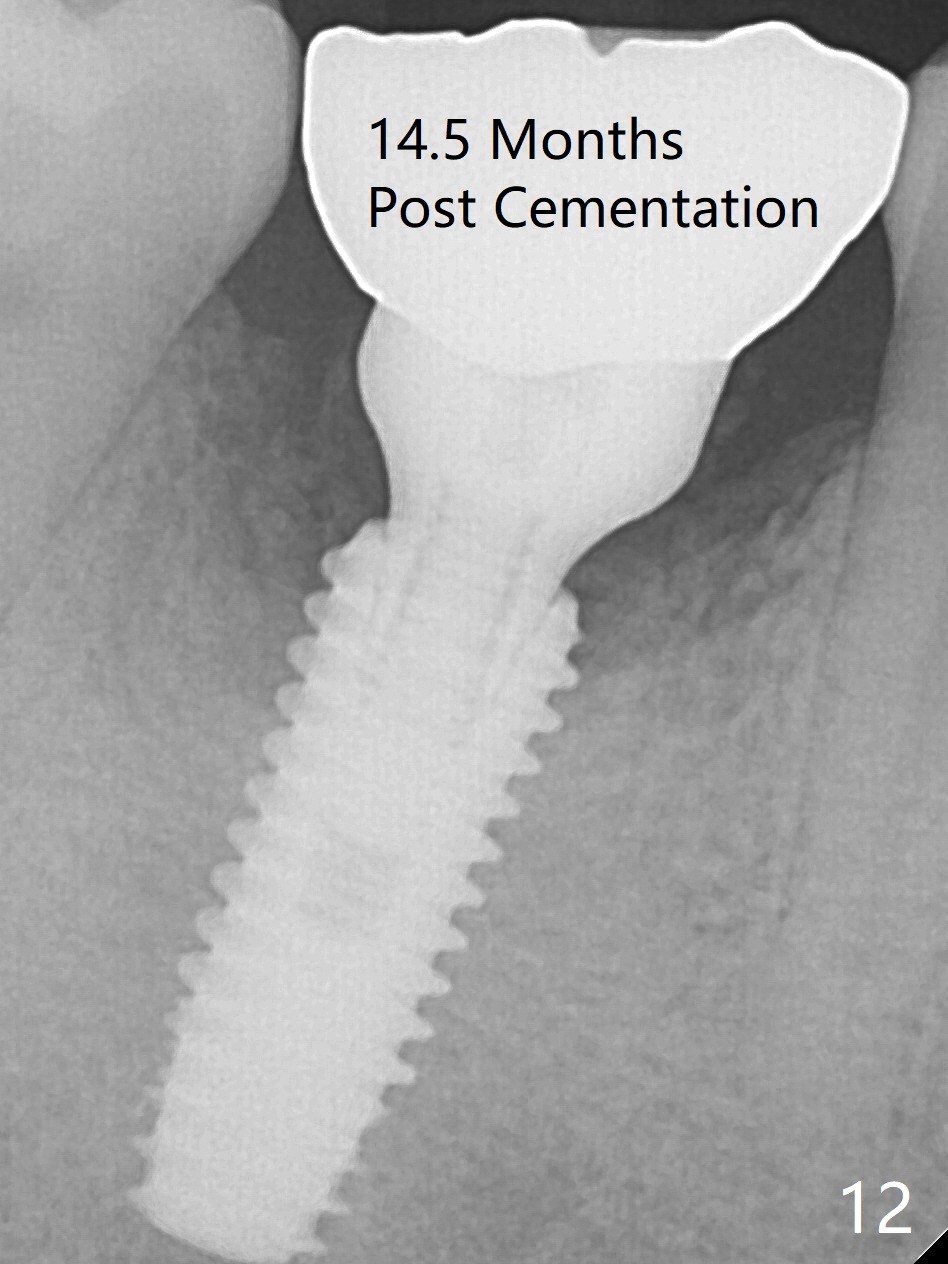
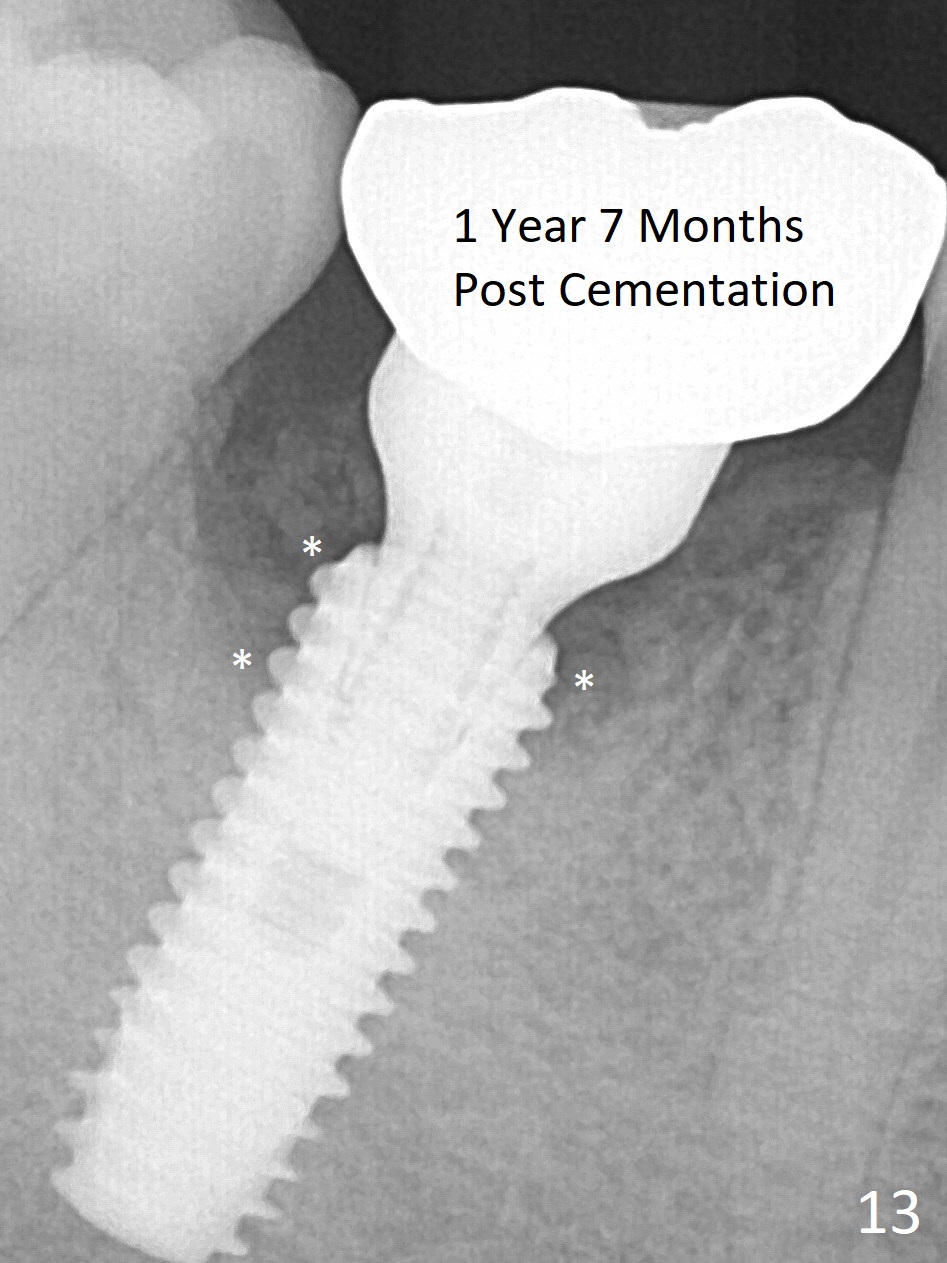
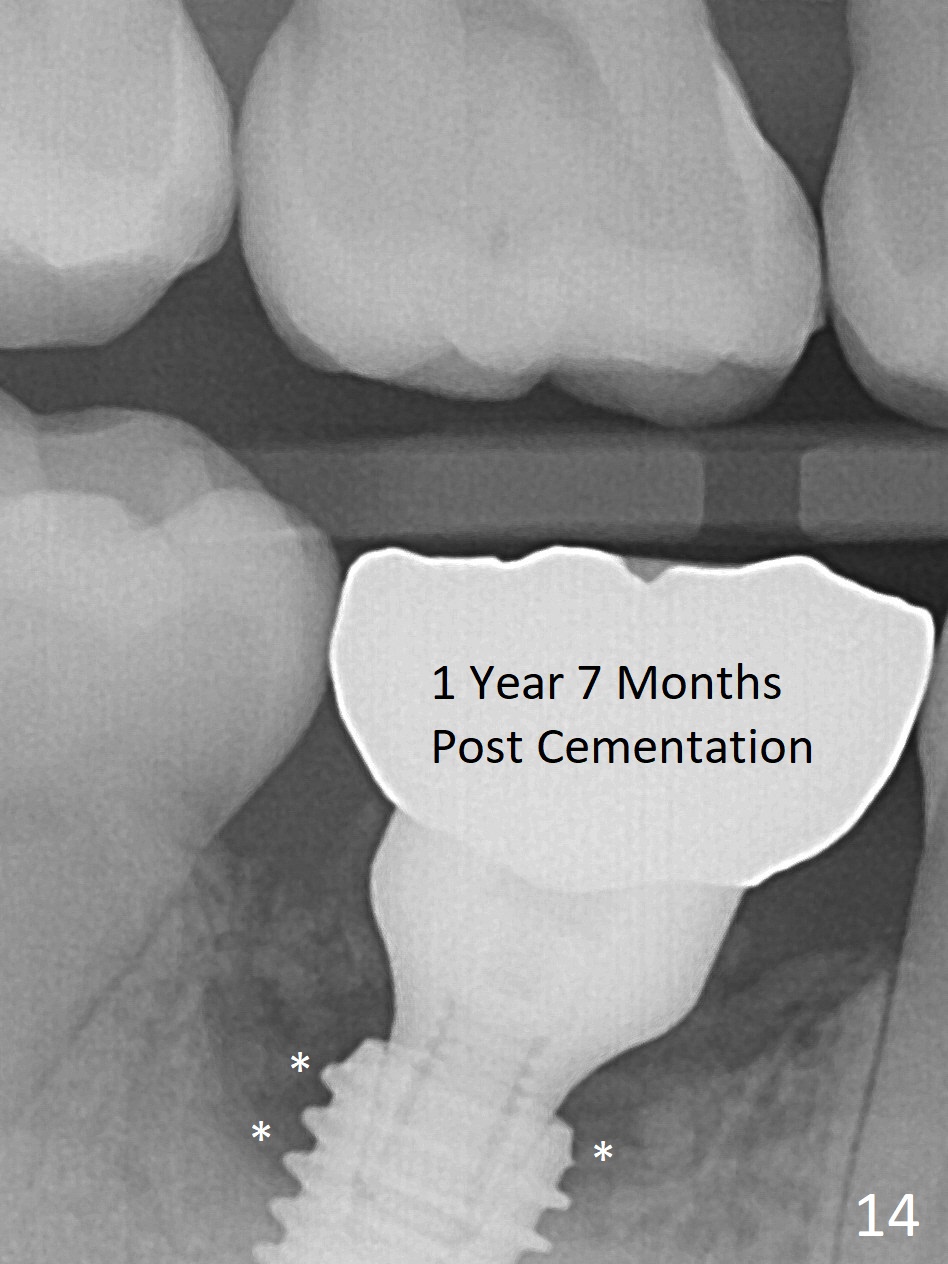
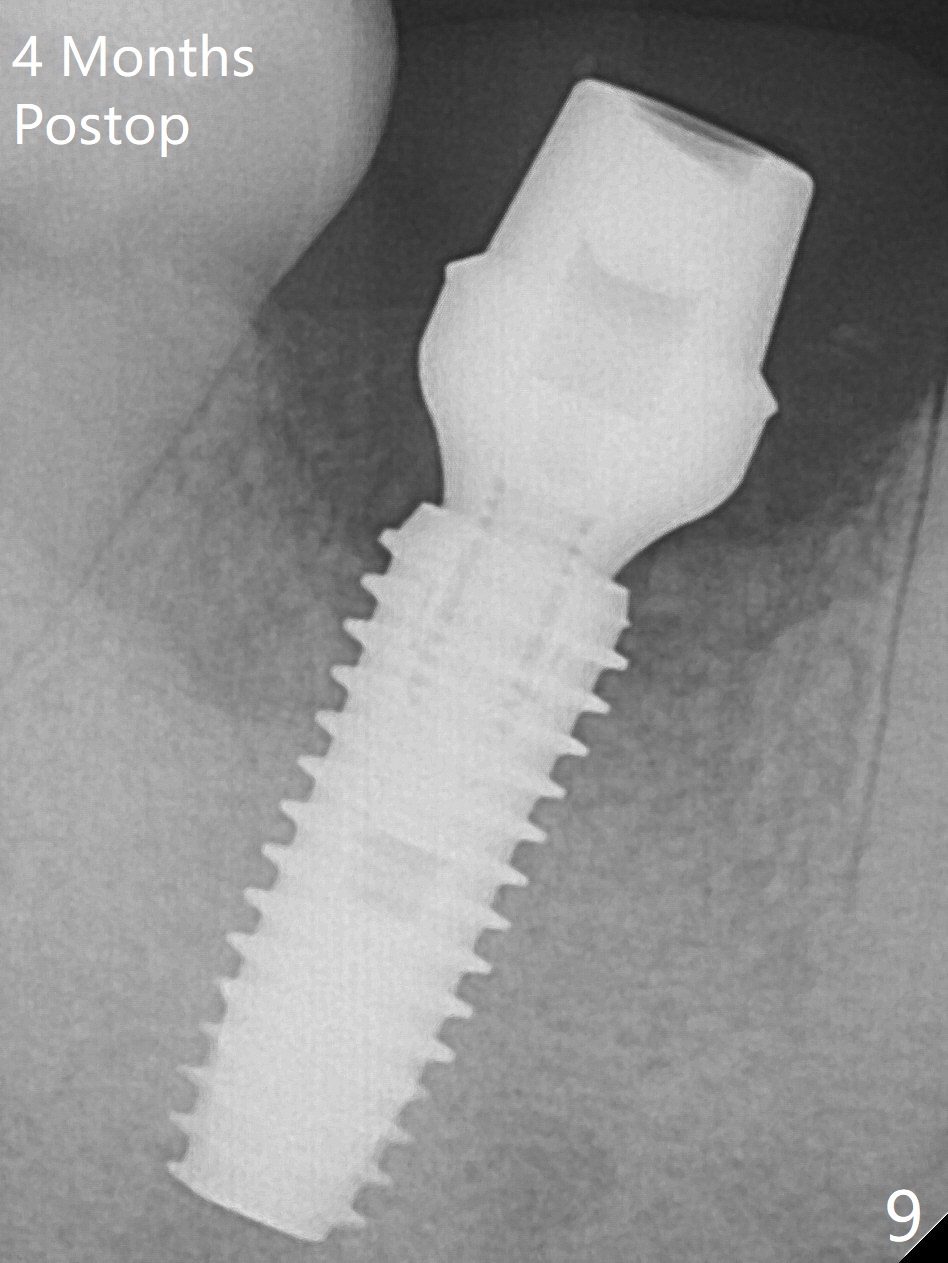
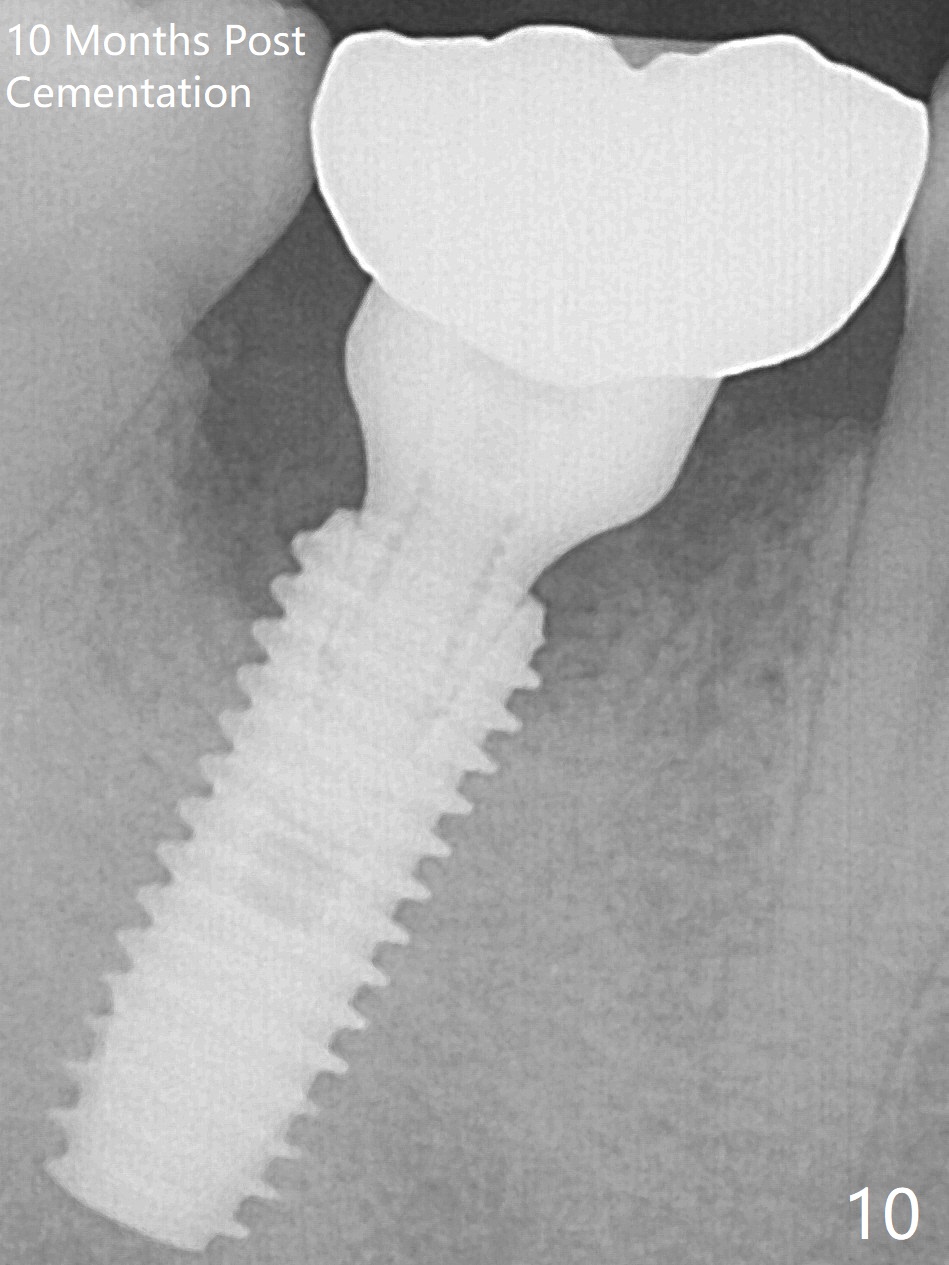
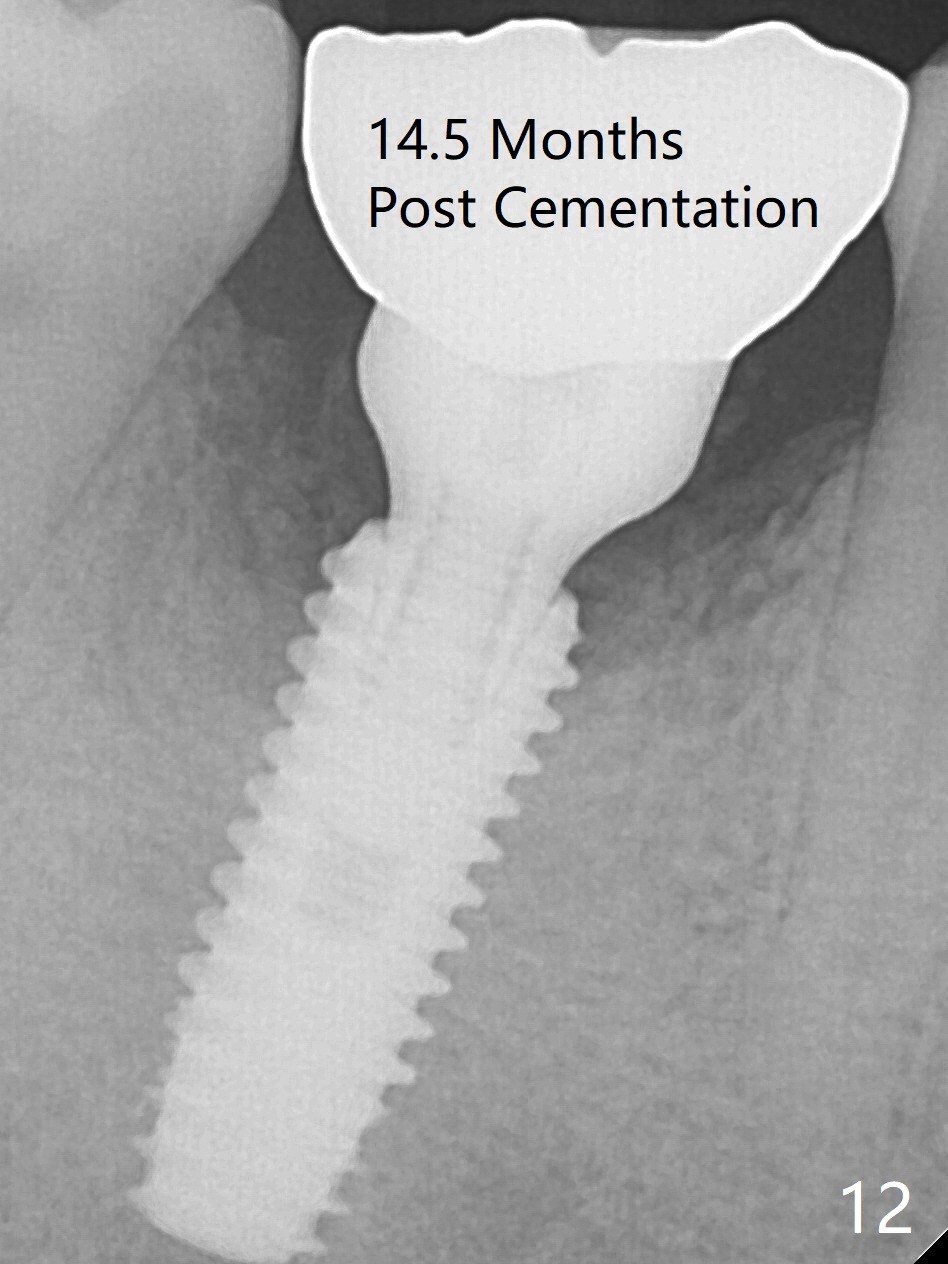
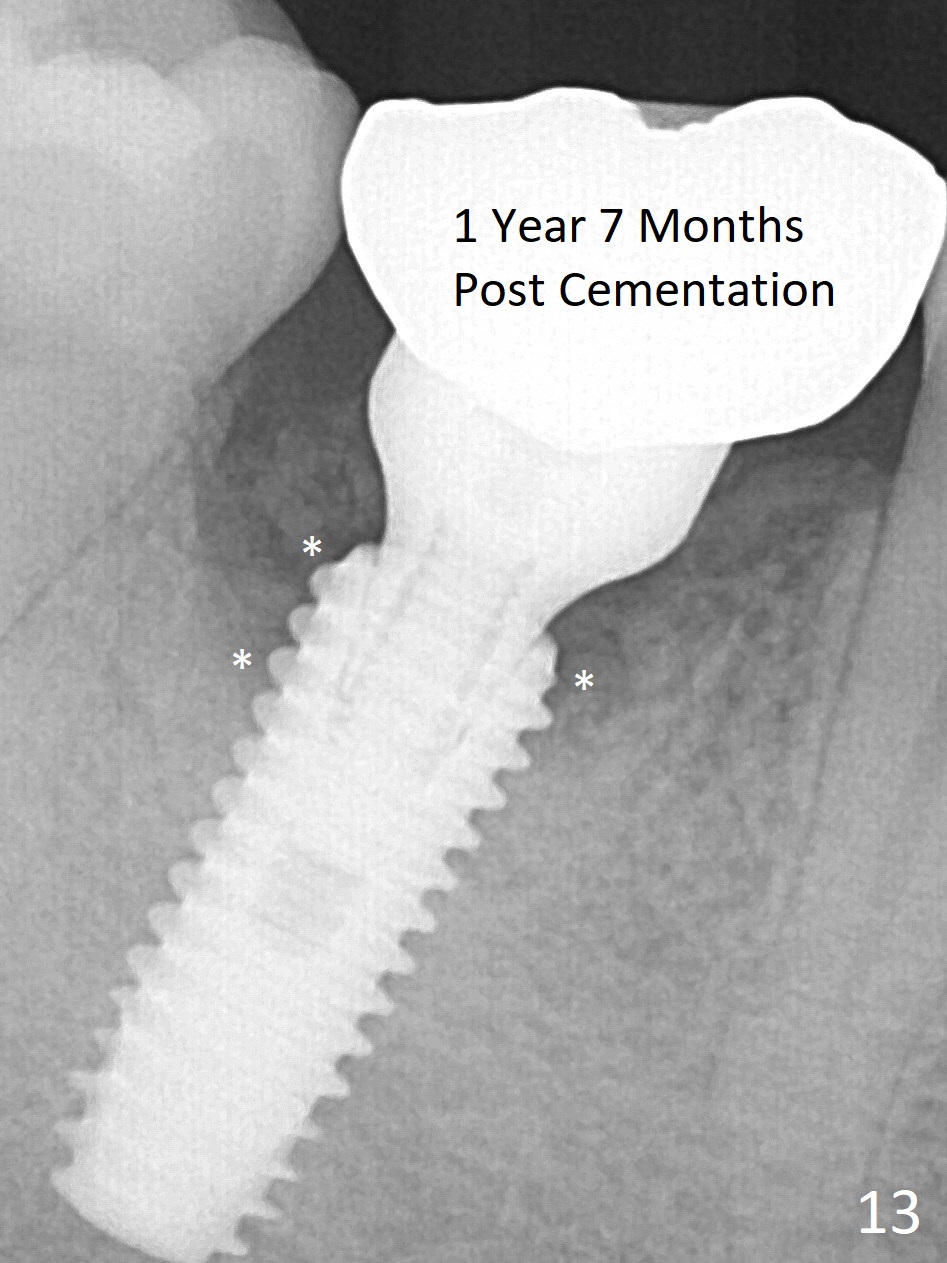
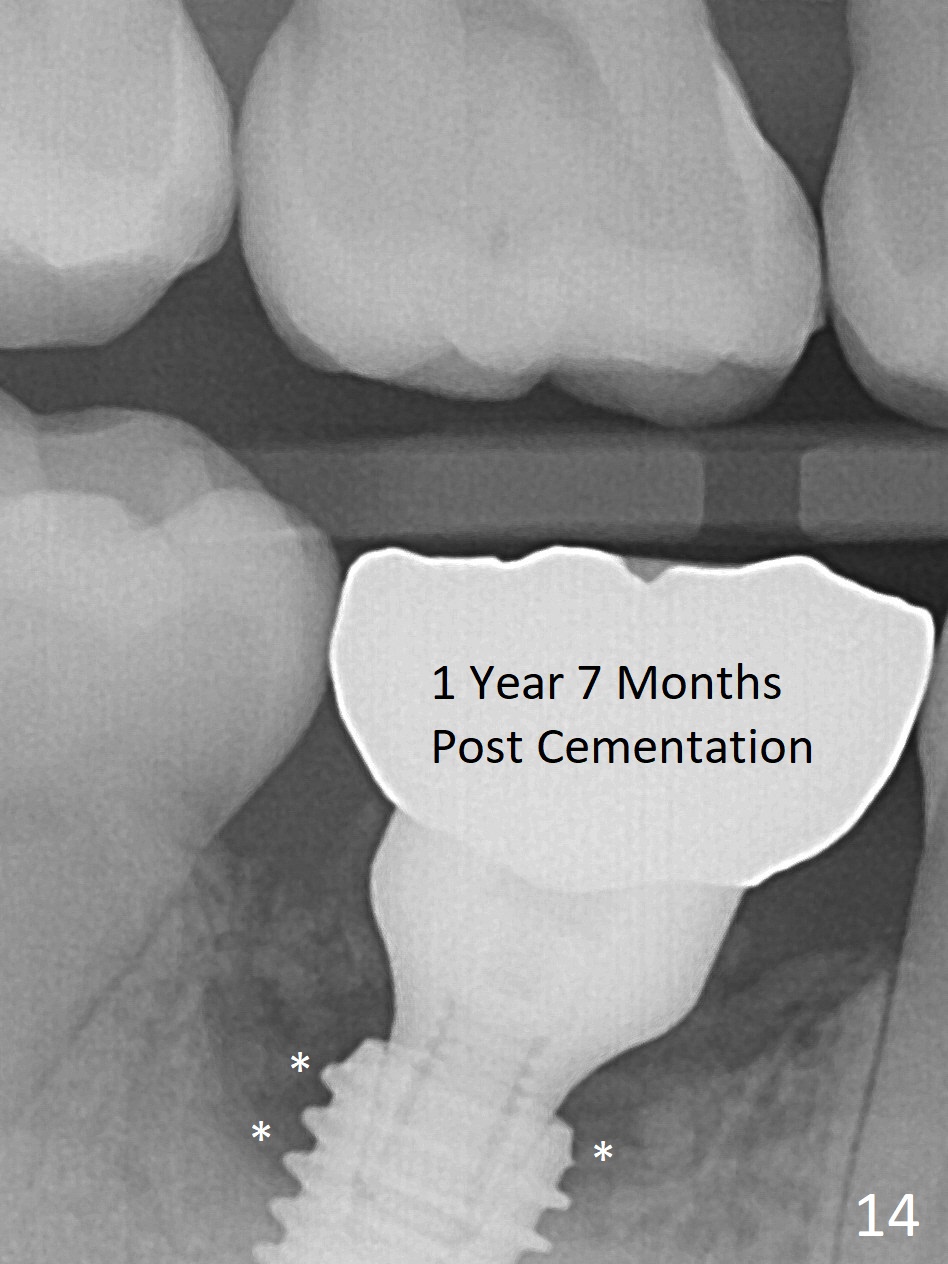
Fortunately no paresthesia is reported postop. Why is the Inferior Alveolar Canal not violated? Fig.7 is a coronal section of CBCT taken for a 40-year-old man at the lower 1st molar (at the septum). At the region, the Canal (brown circle) is close to the lingual plate (L). Because of severe bone loss of the lingual plate of this case (Fig.8 *), osteotomy is intentionally created buccal (green). The deep osteotomy may not contact the Canal, while the hemorrhage may stem from the medullary space (M in Fig.4,7). Bone morphology at the coronal end of the implant apparently changes 4 months postop, suggesting osteointegration (Fig.9). Impression is taken. Bone density around the implant at the crest seems to increase (Fig.10), while there is no soft tissue deficiency 10 months post cementation (Fig.11). The bone appears to regenerate toward the abutment, particularly distally, 14.5 months post cementation (Fig.12). Periimplantitis develops (bleeding on water pik and erythematous and tender buccal gingiva) 1 year 7 months post cementation (Fig.13,14). The 1st three threads are exposed (*). Bone graft with PRF and 6-month membrane or Cytoplast will be needed. Pain disappears 3 days of oral antibiotic. The gingiva looks healthy 1 month later when he returns for bone graft (Fig.15). But the lingual gingival cuff is not so healthy when the crown/abutment is removed (Fig.16 <). Bone graft is not done. For those patients with suboptimal oral hygiene, implants should be placed as low as possible, better with guide for precision.
Return to
Lower
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table),
IBS
Xin Wei, DDS, PhD, MS 1st edition 06/26/2017, last revision 07/13/2019