




 |
 |
 |
 |
||
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
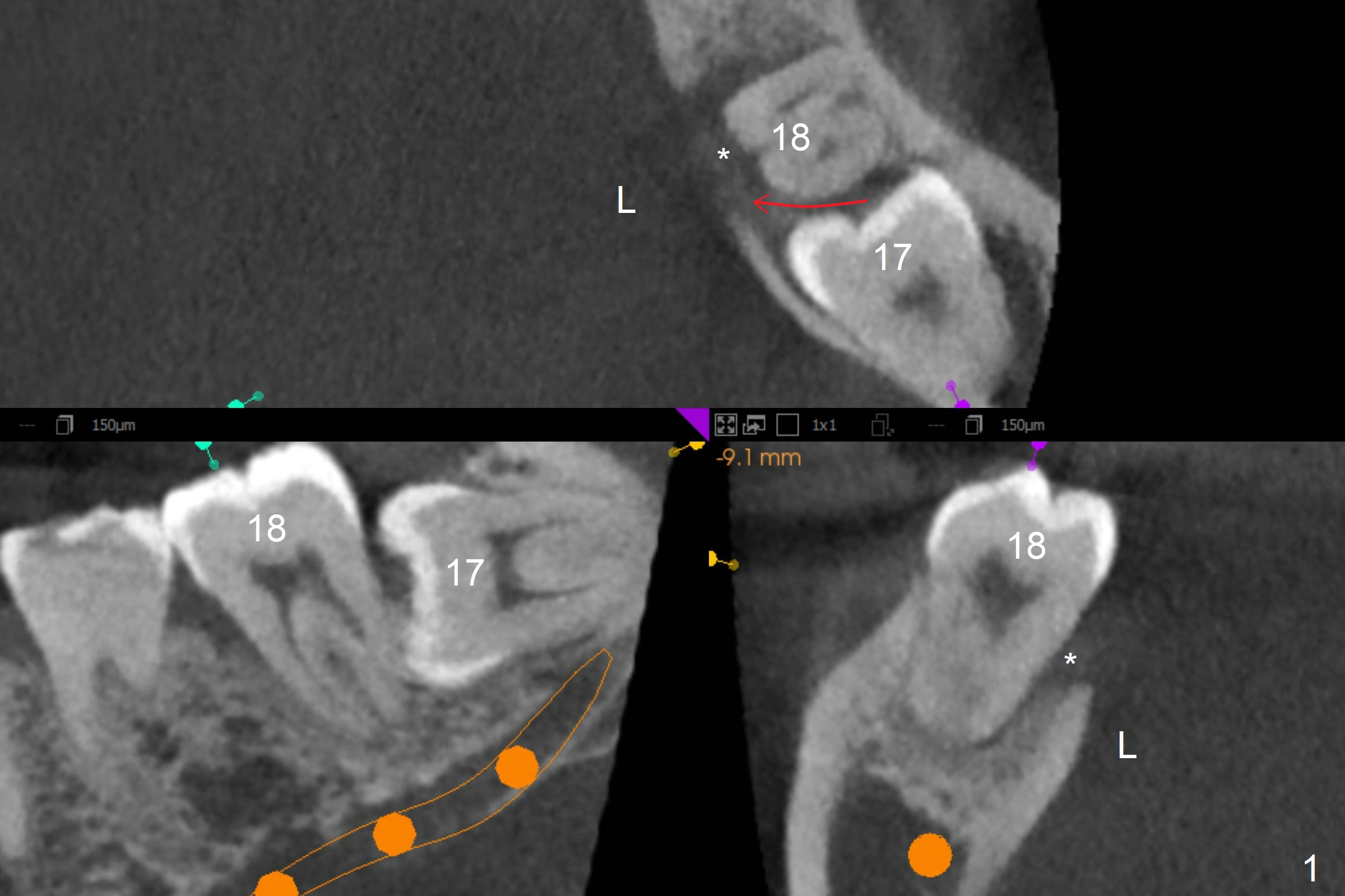
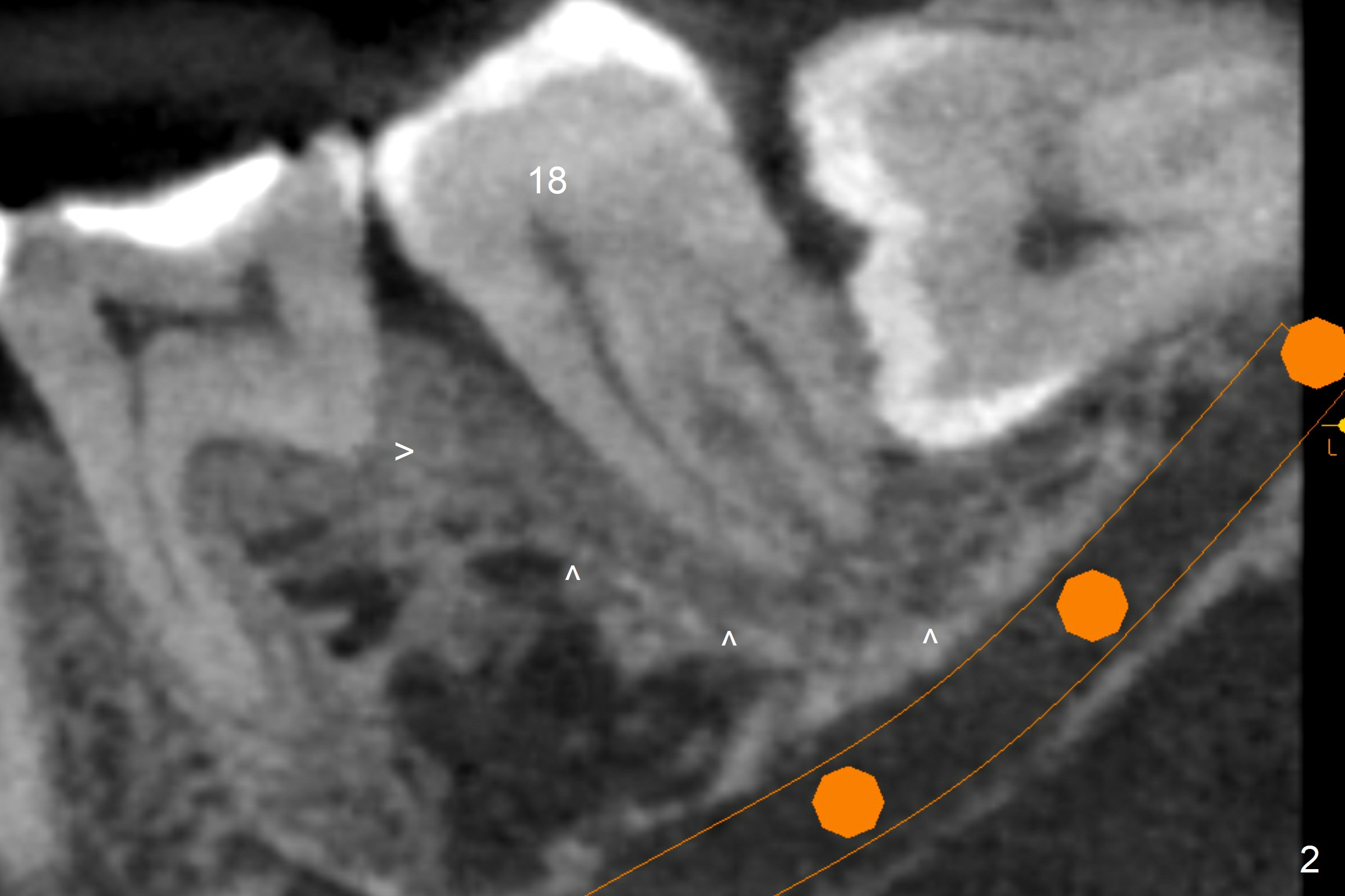
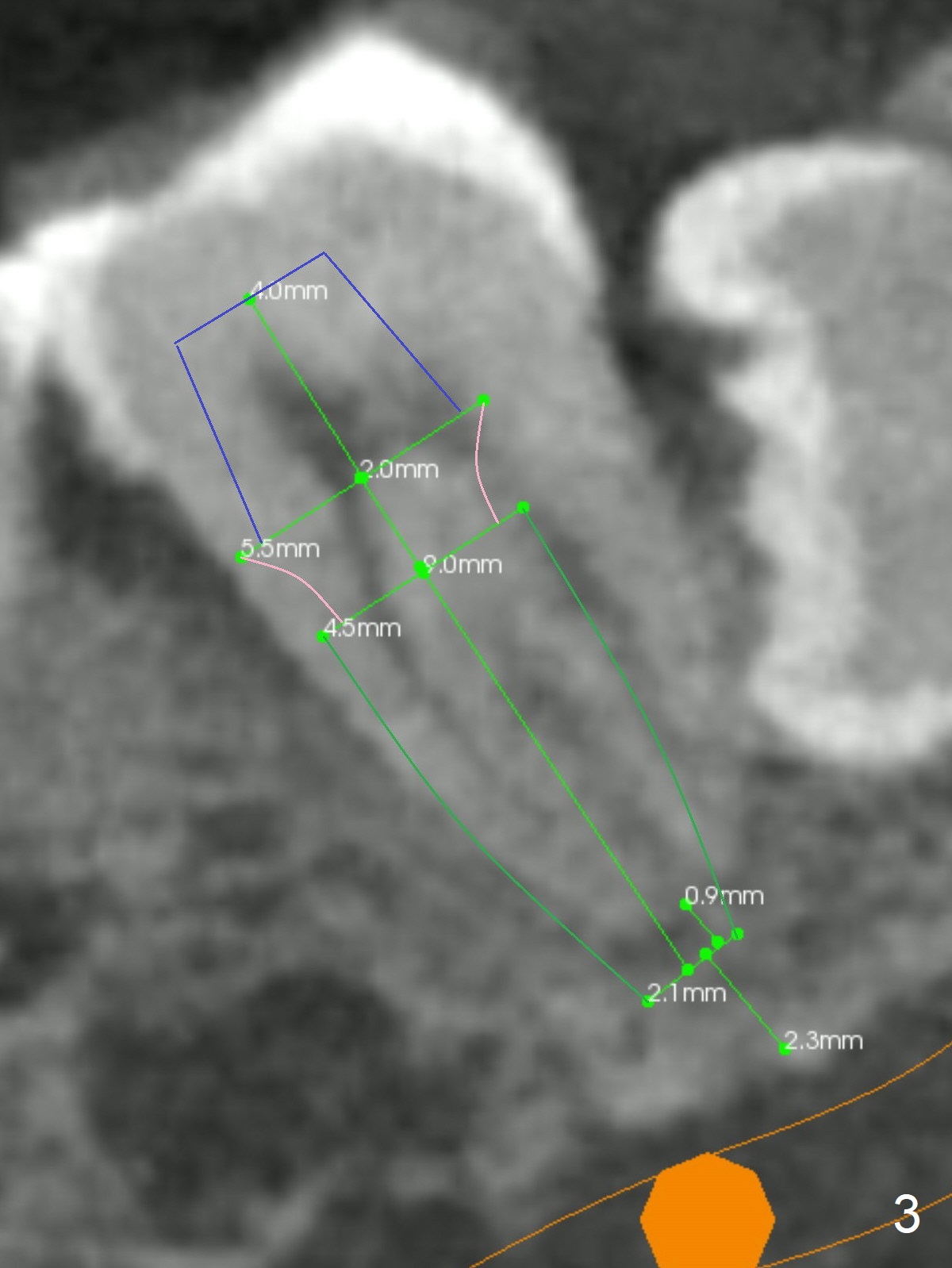
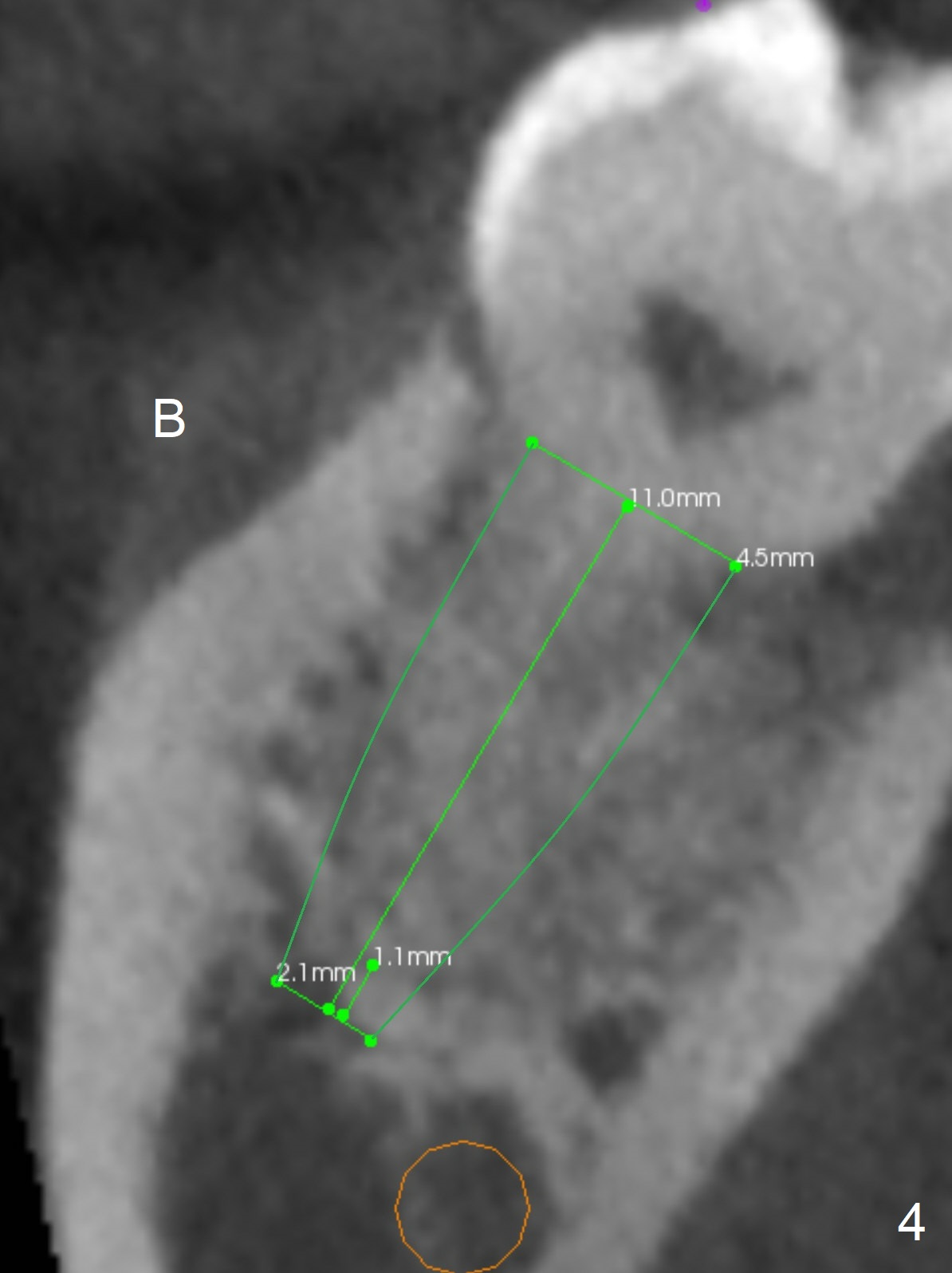
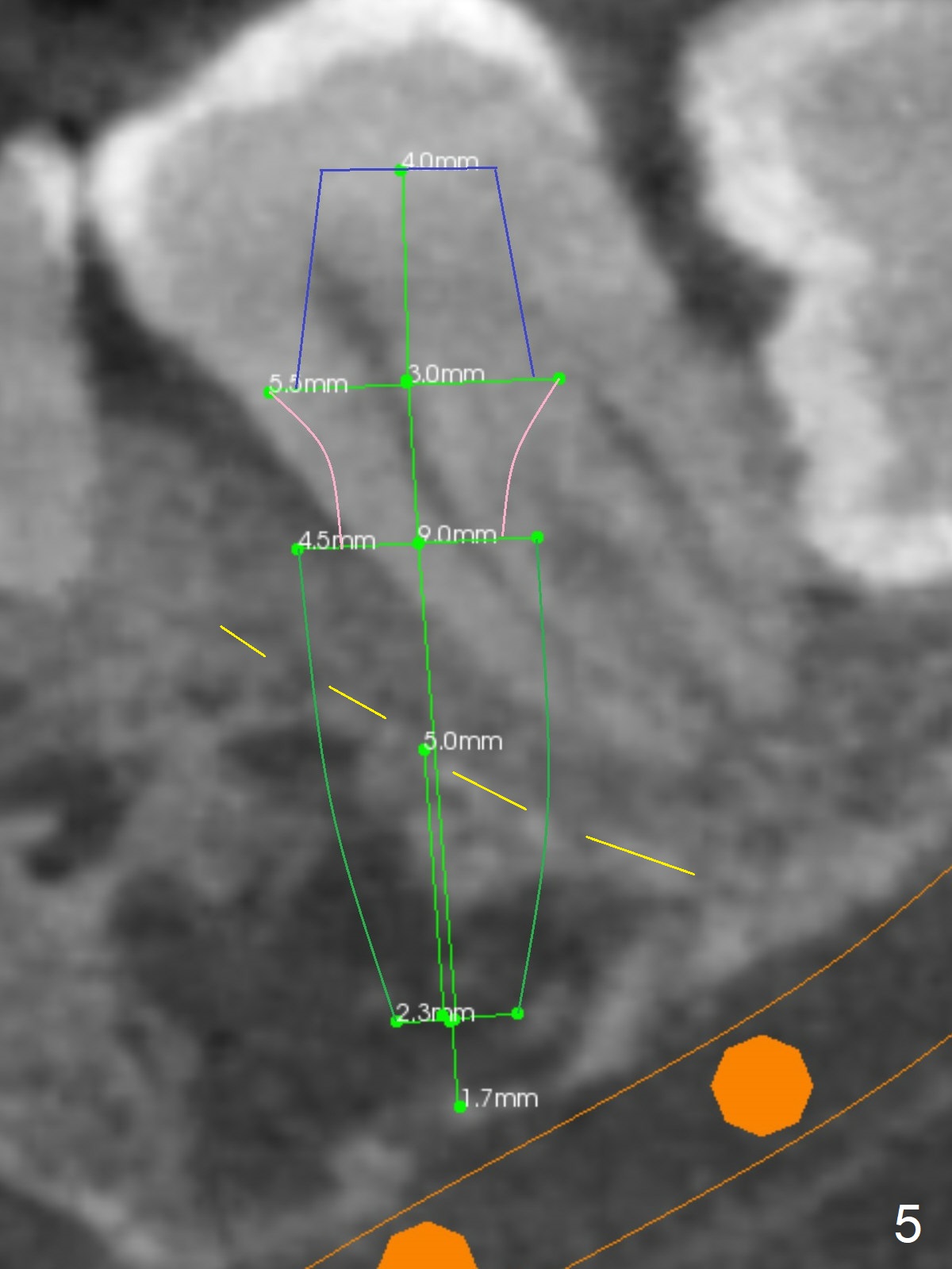
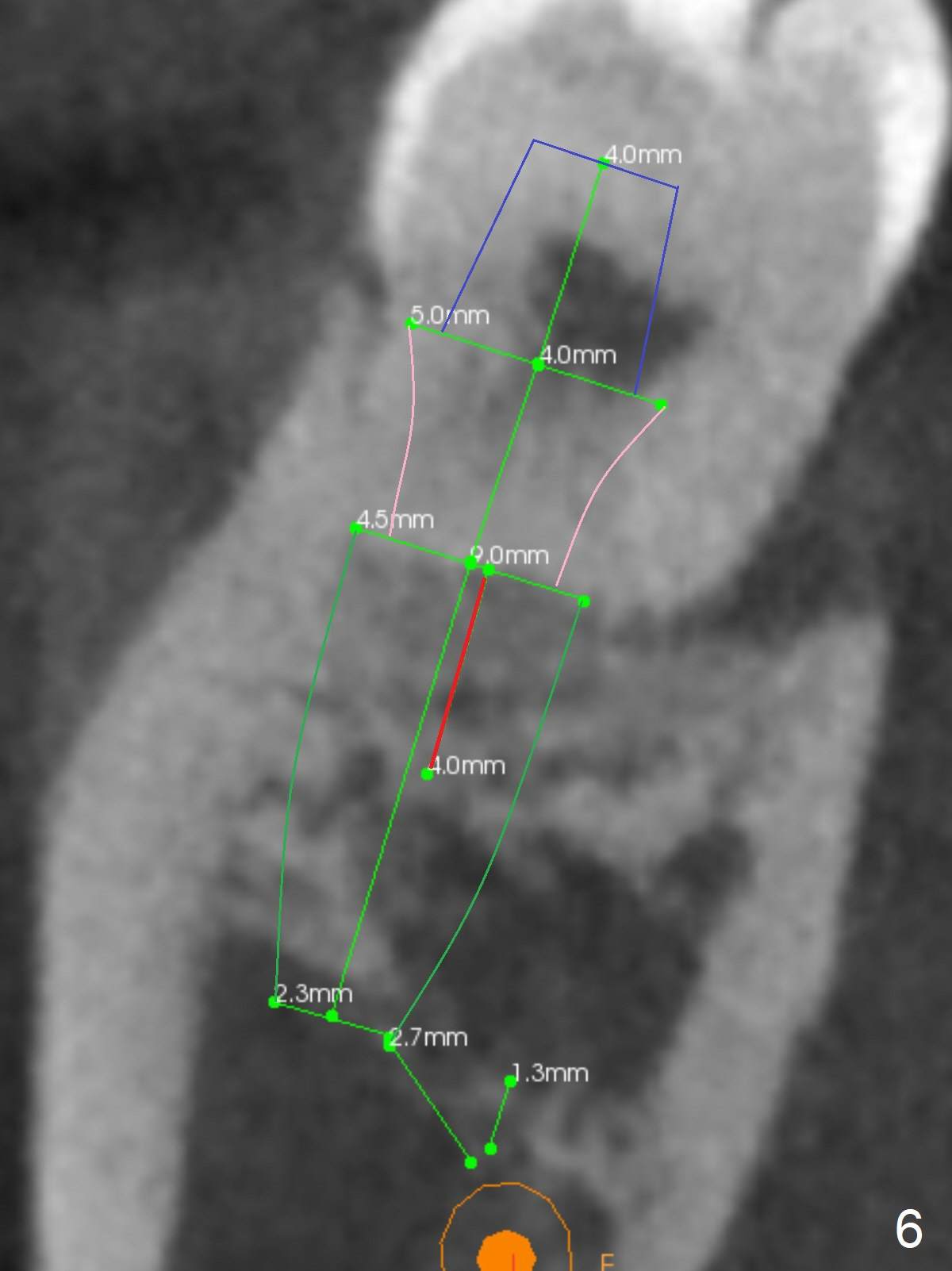
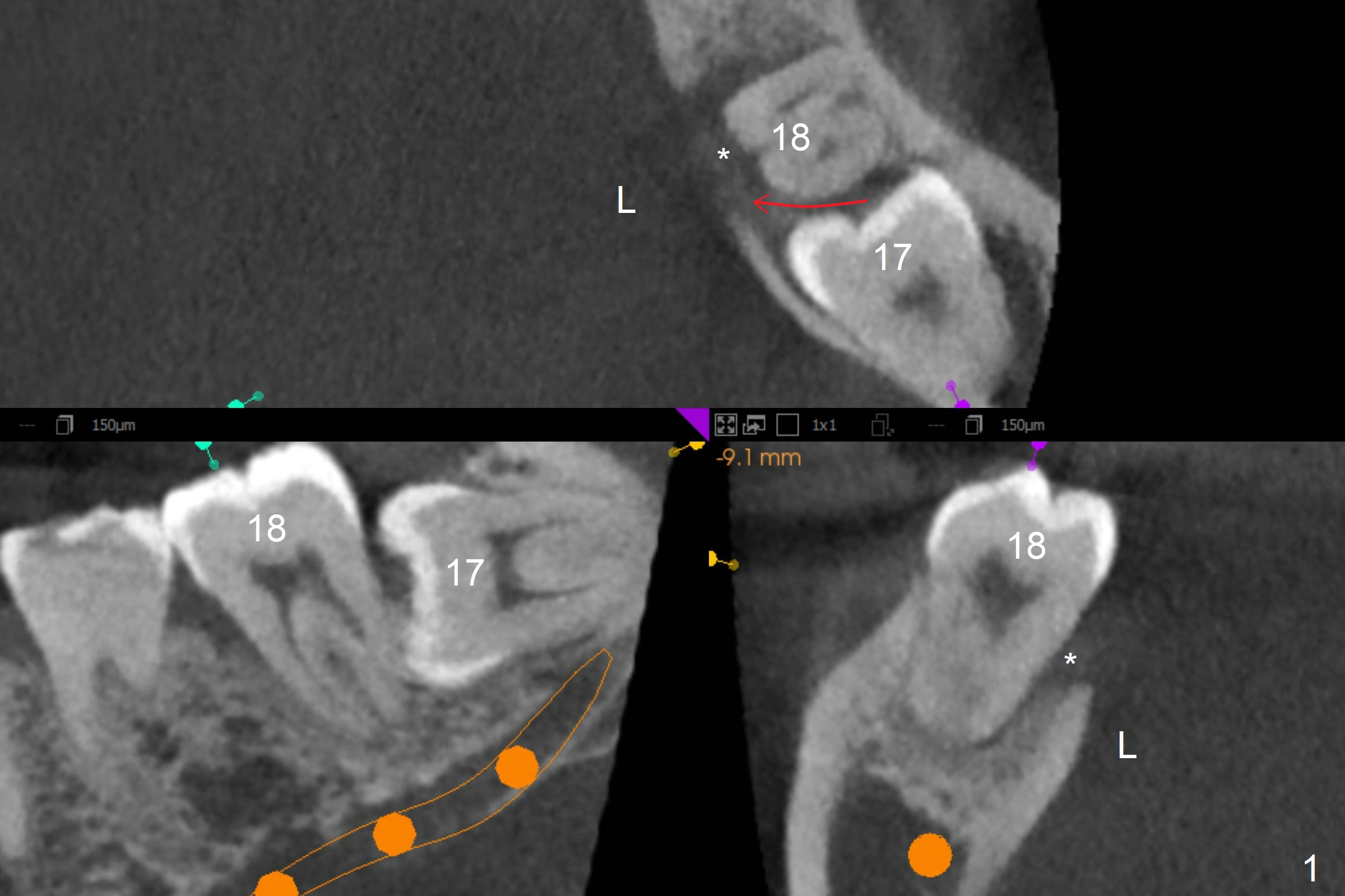
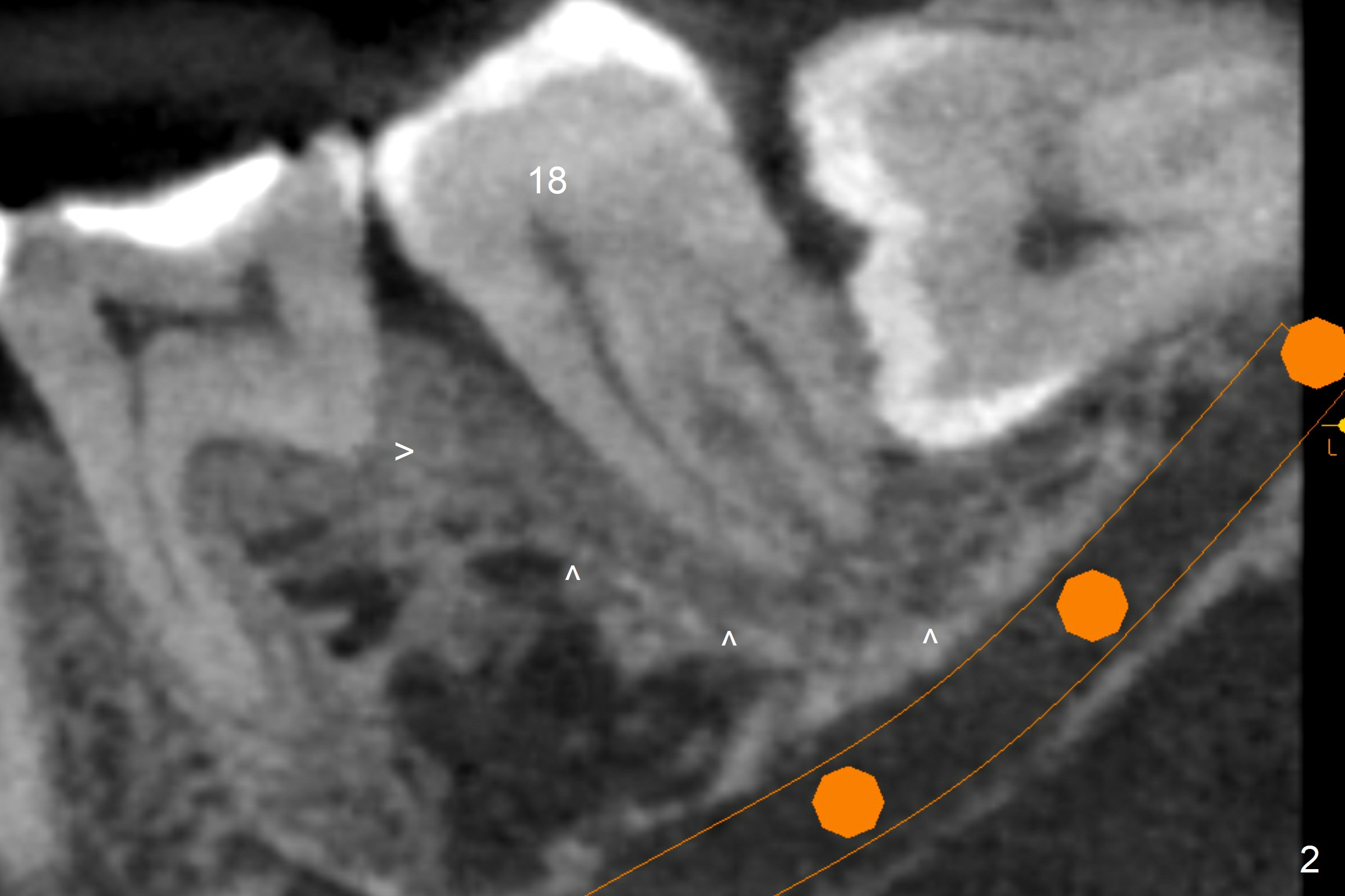
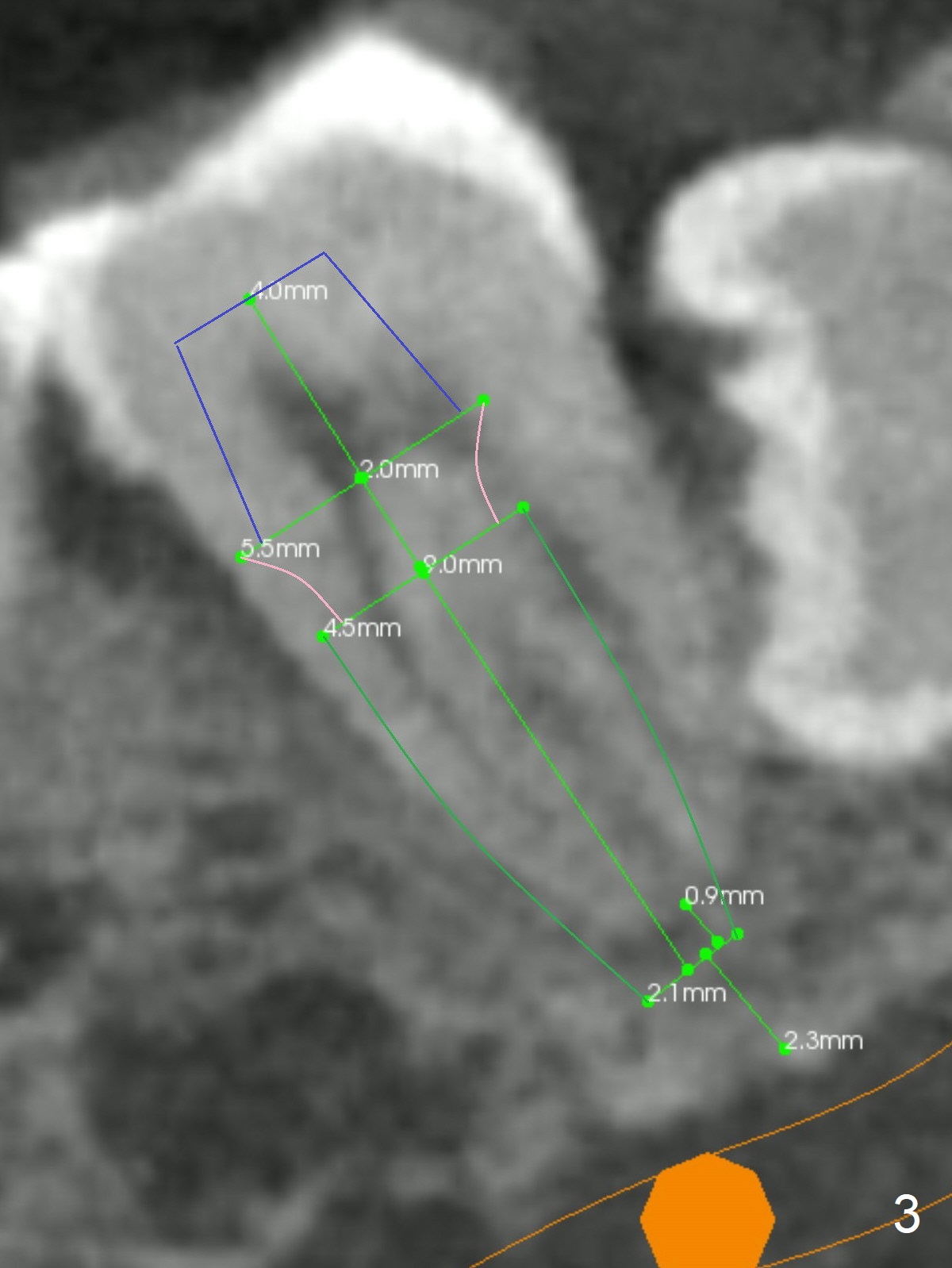
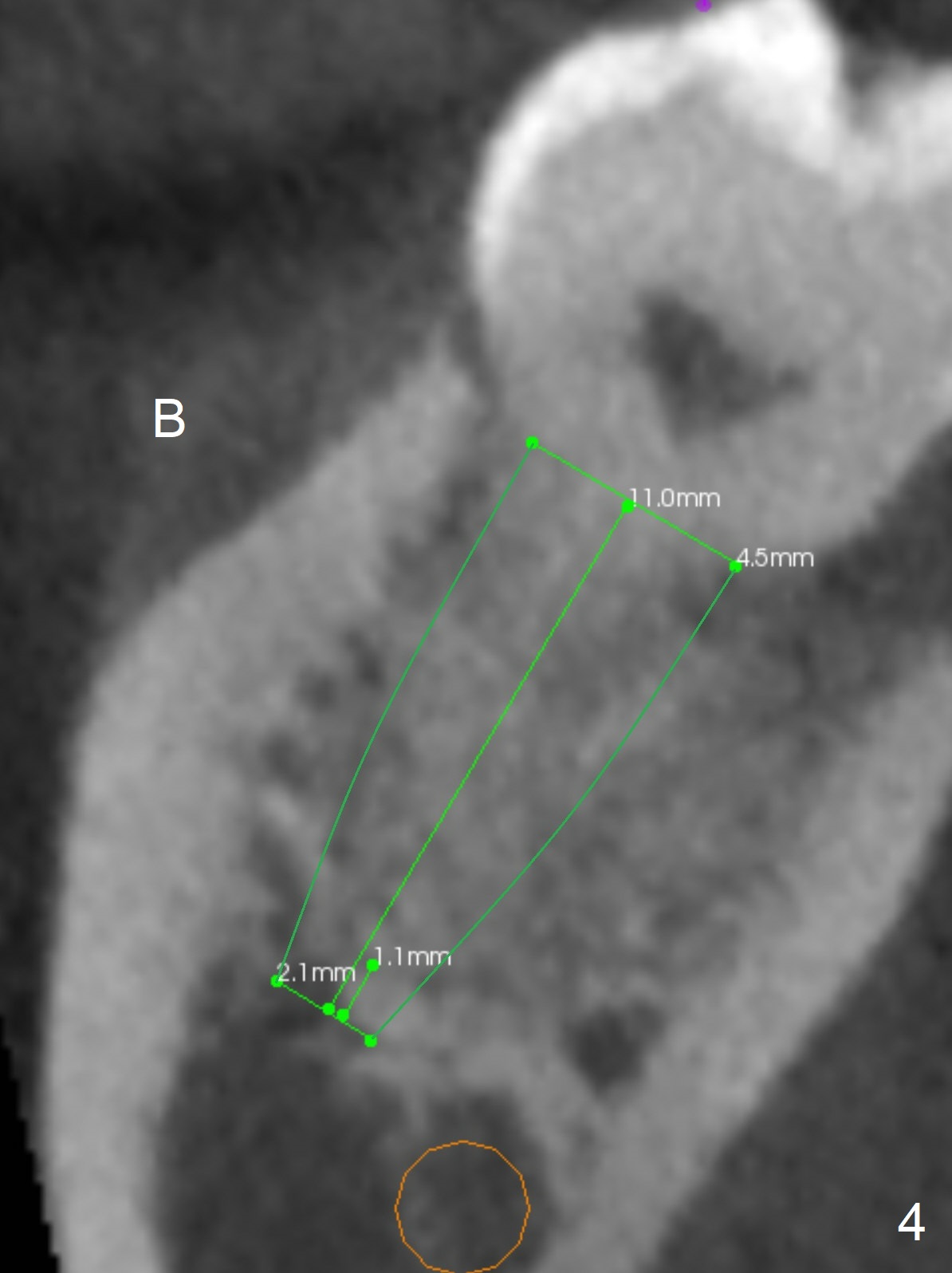
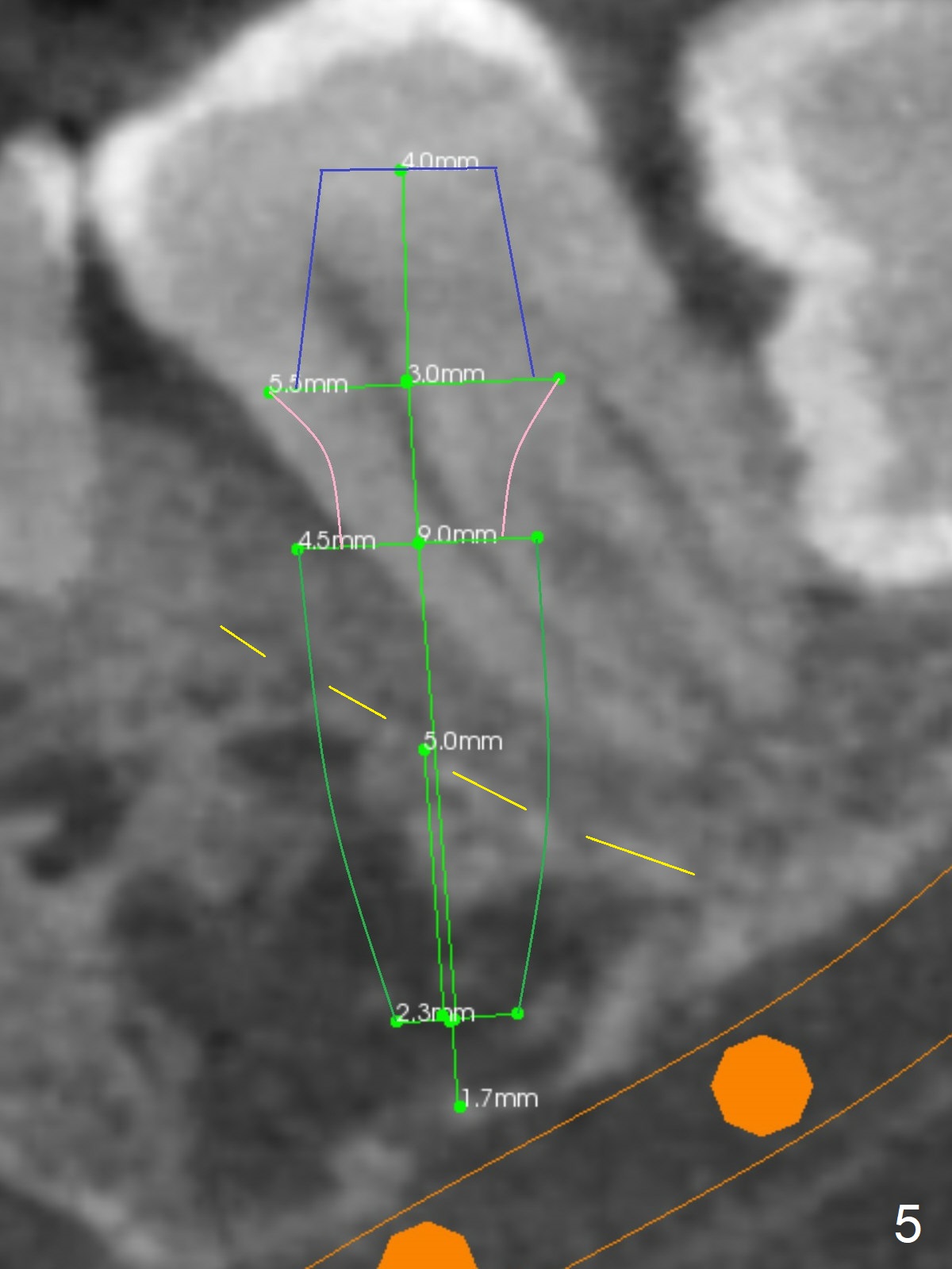
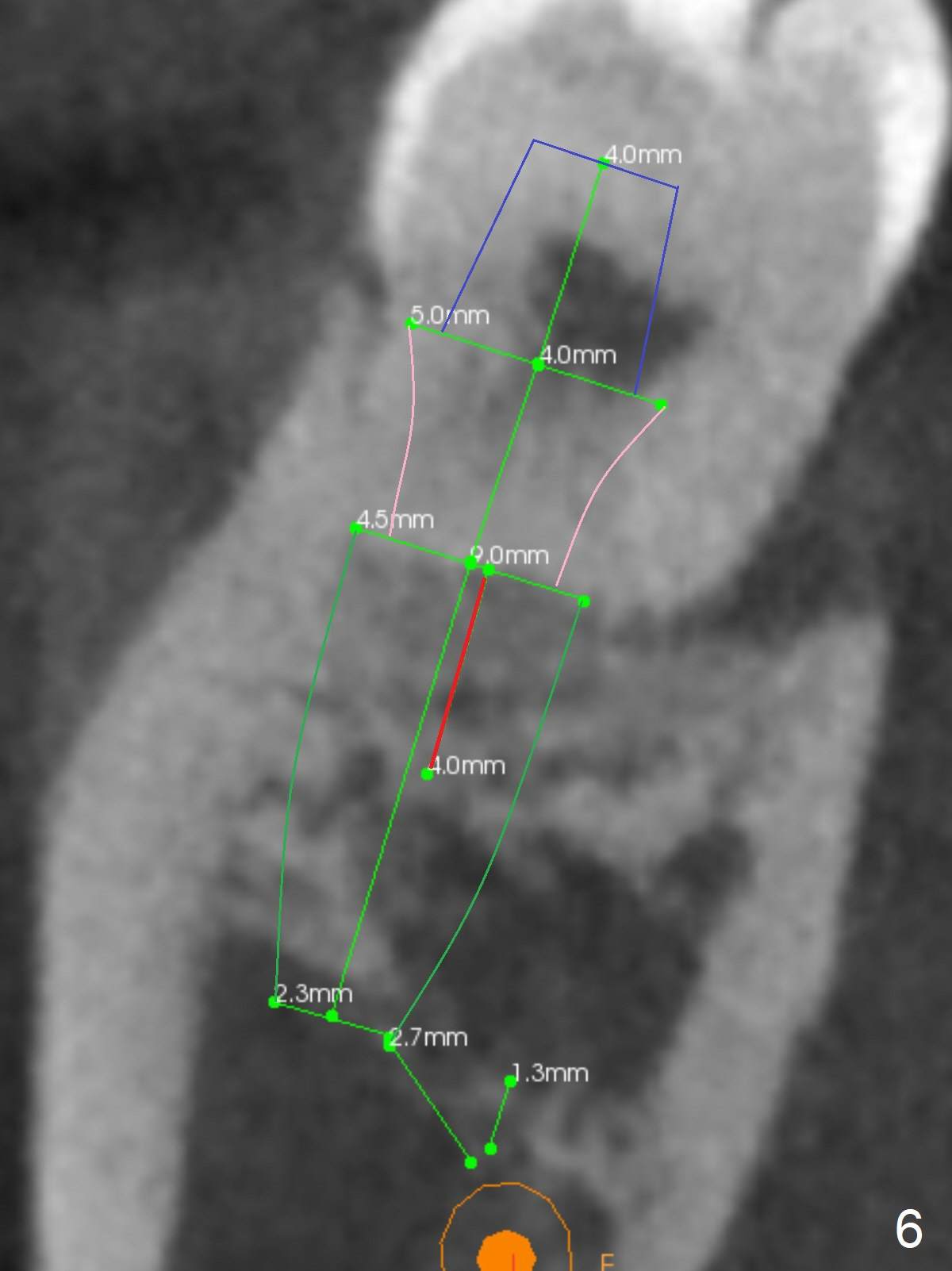
A 40-year-old man removes food debris from the lower left area, probably between #17 and 18, using Water Pik. Initially it looks as if the bone loss lingual (Fig.1 (CBCT with 3 sections) L) to #18 is derived from #17 (red curved arrow). Closer look shows generalized thickened periodontal ligament space at #18 (Fig.2 arrowheads). The patient requests extraction of the tooth #17; the tooth #18 seems non-salvageable. When an immediate implant is placed in the middle of the socket (Fig.3,4 (coronal section)), there is limited amount of the native bone to stabilize the implant (~1 mm). In contrast, there is approximately 5 mm of the native bone for primary stability if the implant is placed in the mesial slope of the fused socket (Fig.5 yellow dashed line). The implant should be placed buccally (B) to reduce the chance of nerve injury (Fig.4,6).
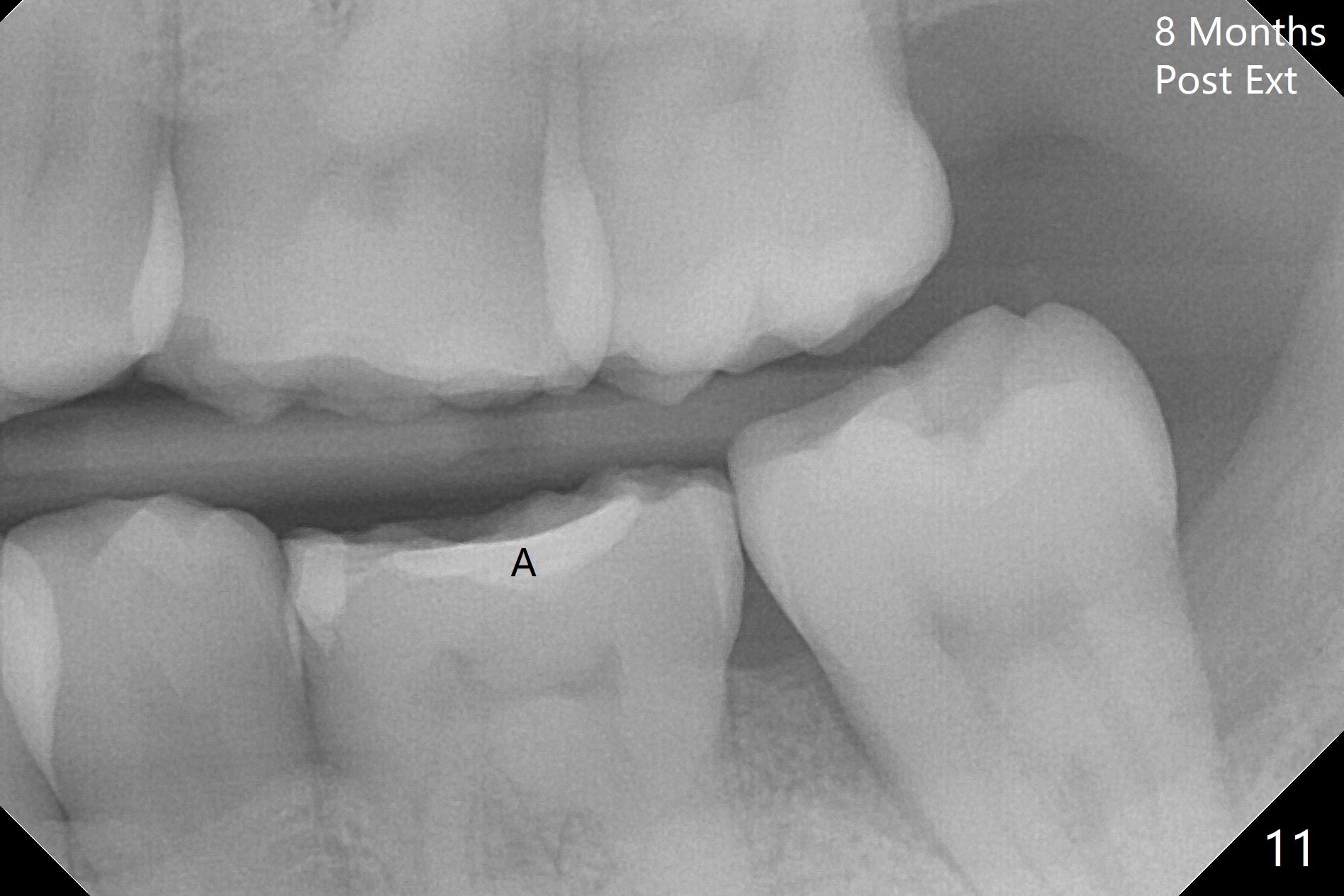
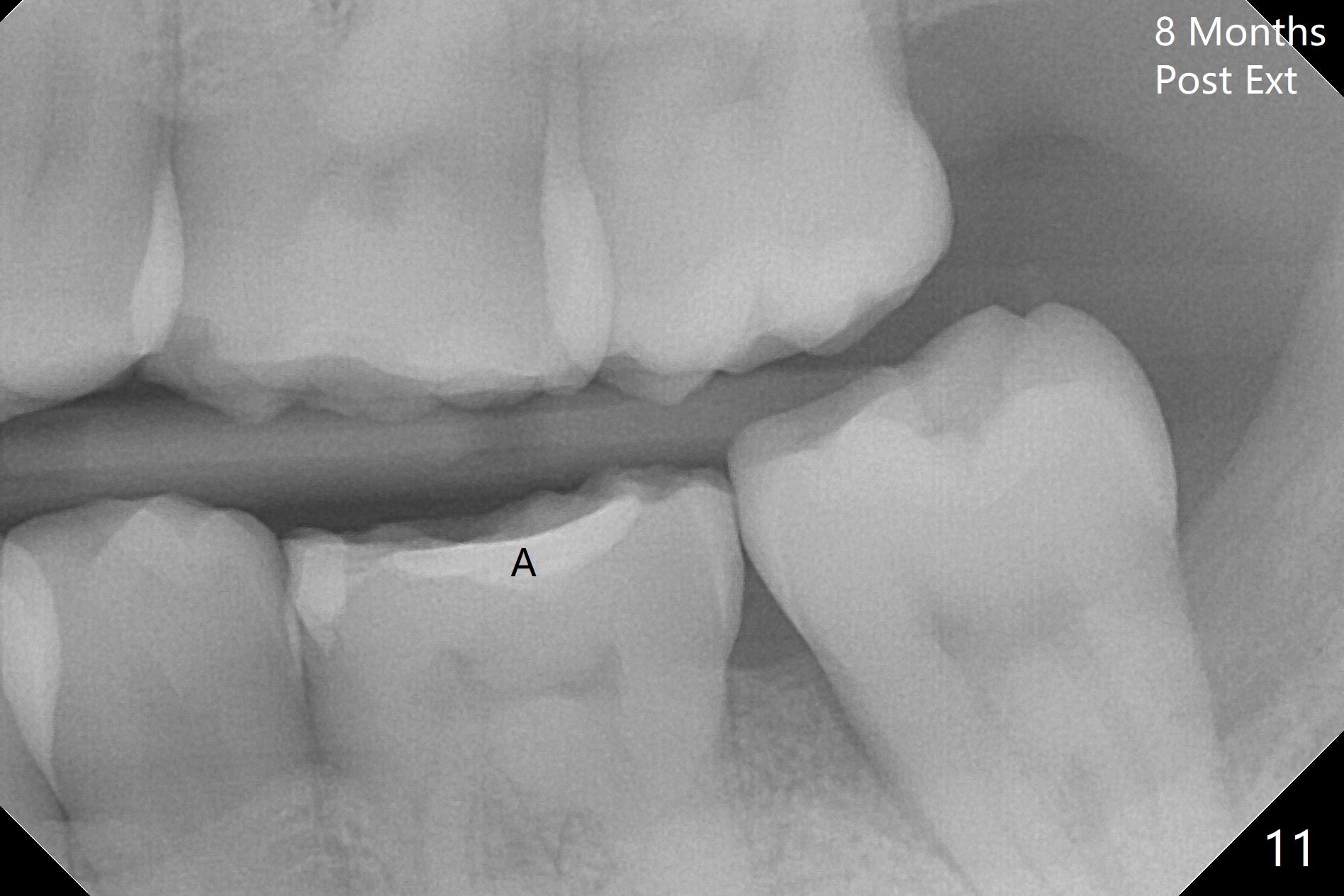
Photos are taken to show occlusal wear (bruxism) of the teeth #31 and 17 (Fig.7,8) prior to #17 extraction. Osteogen plug is placed in #17 socket after extraction and SRP at #18. The bone height at #18 distal seems to increase 2 years 4 months post extraction (Fig.9-12). The 1st molars have enamel hypoplasia with occlusal wear. In addition, occlusion is abnormal. There is no centric occlusion, partially contributing to periodontitis at #15 and 18. Crown is planned at #19 because of loss of occlusal amalgam (Fig.11 A, 12). Orthodontics may be required, although 2 insurances do not have orthodontic coverage for adults.
Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), IBS, Antibiotic Xin Wei, DDS, PhD, MS 1st edition 07/02/2017, last revision 12/01/2019