
%20trim,%20more%20graft.jpg)
.jpg)





 |
 |
 |
 |
|
 |
 |
%20trim,%20more%20graft.jpg) |
.jpg) |
 |
 |
 |
 |
||
 |
 |
|||
Use of Partial as Surgical Stent
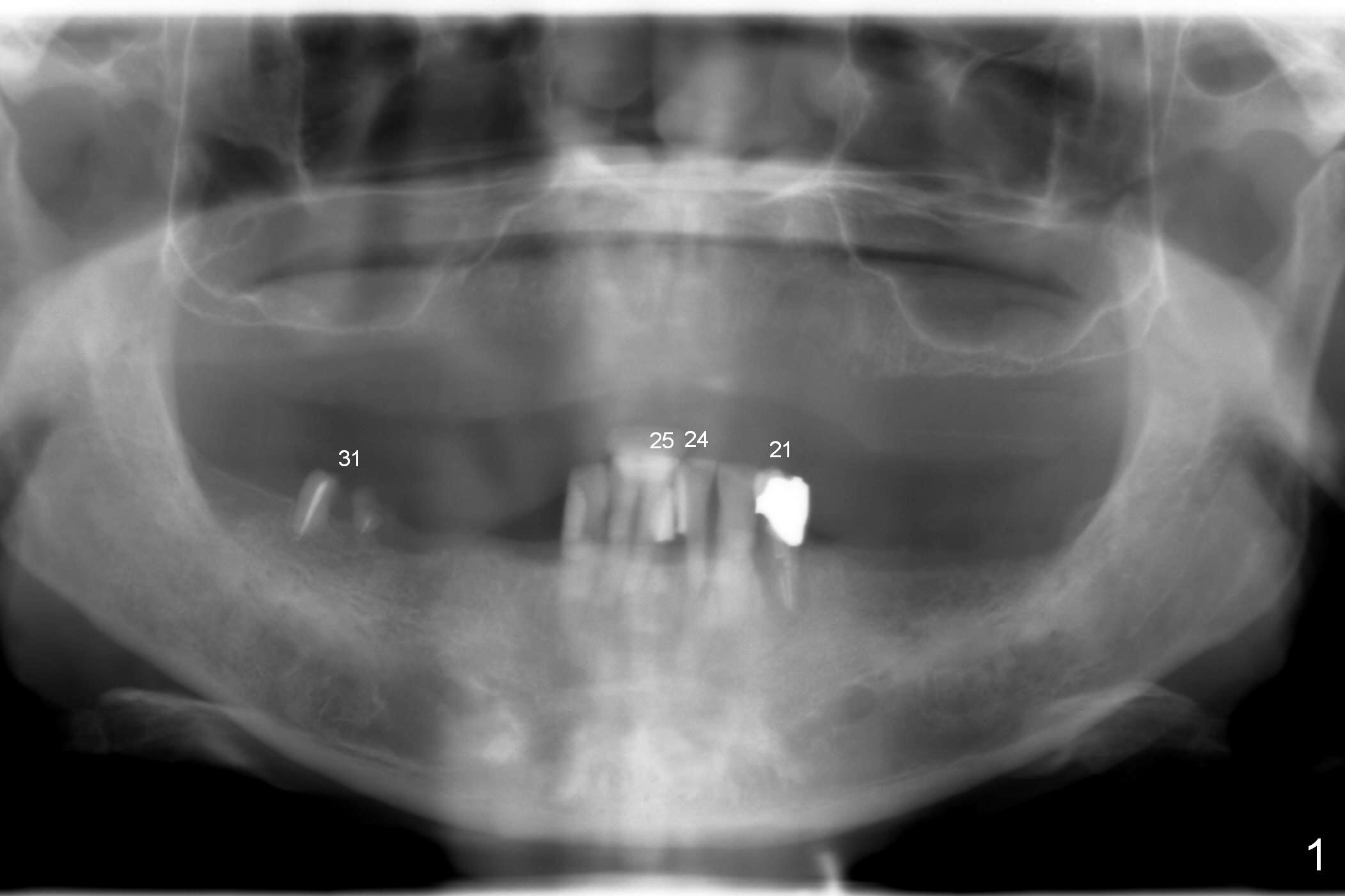
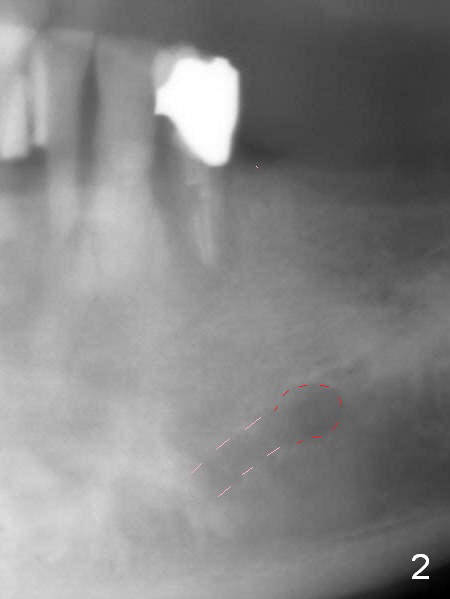
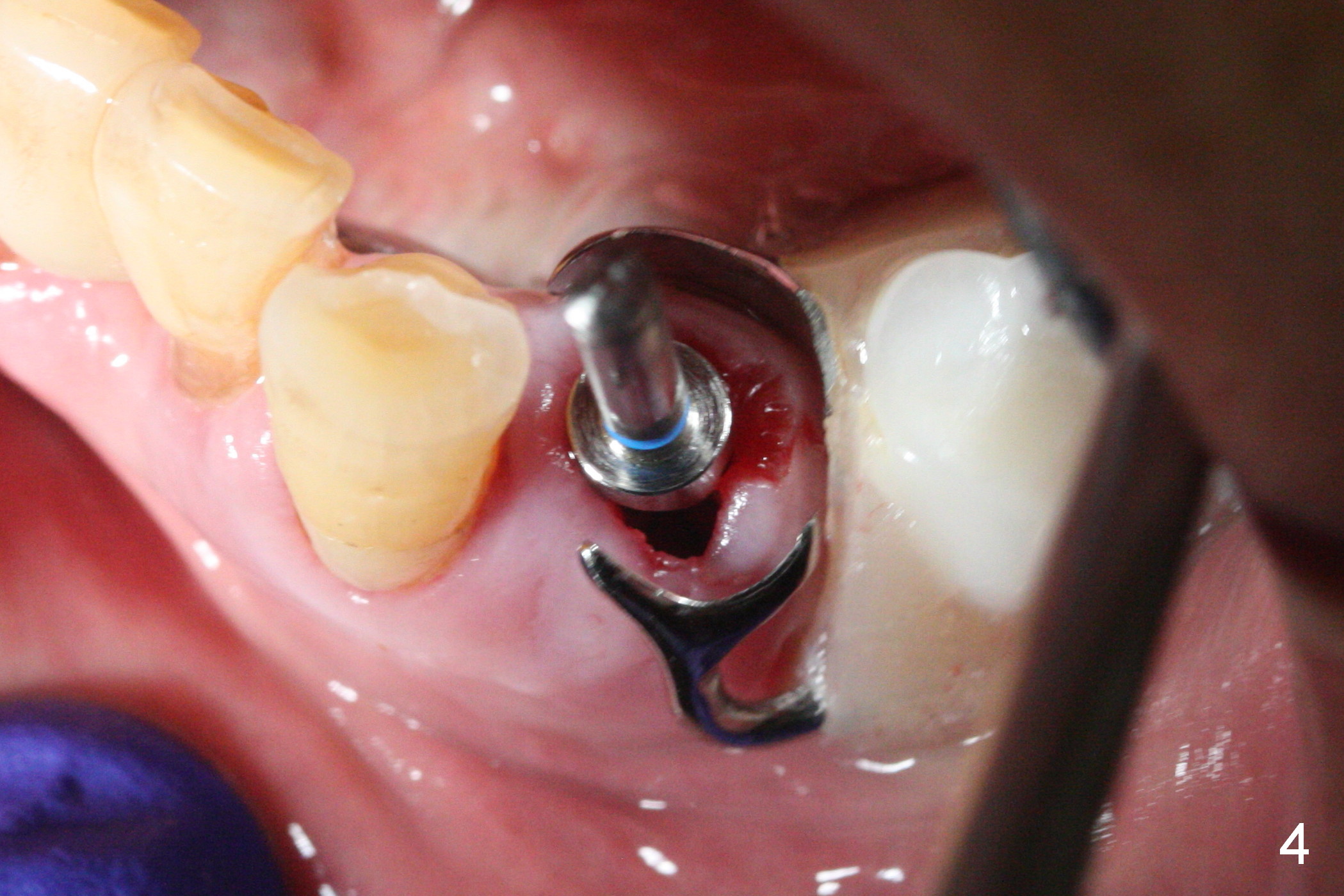
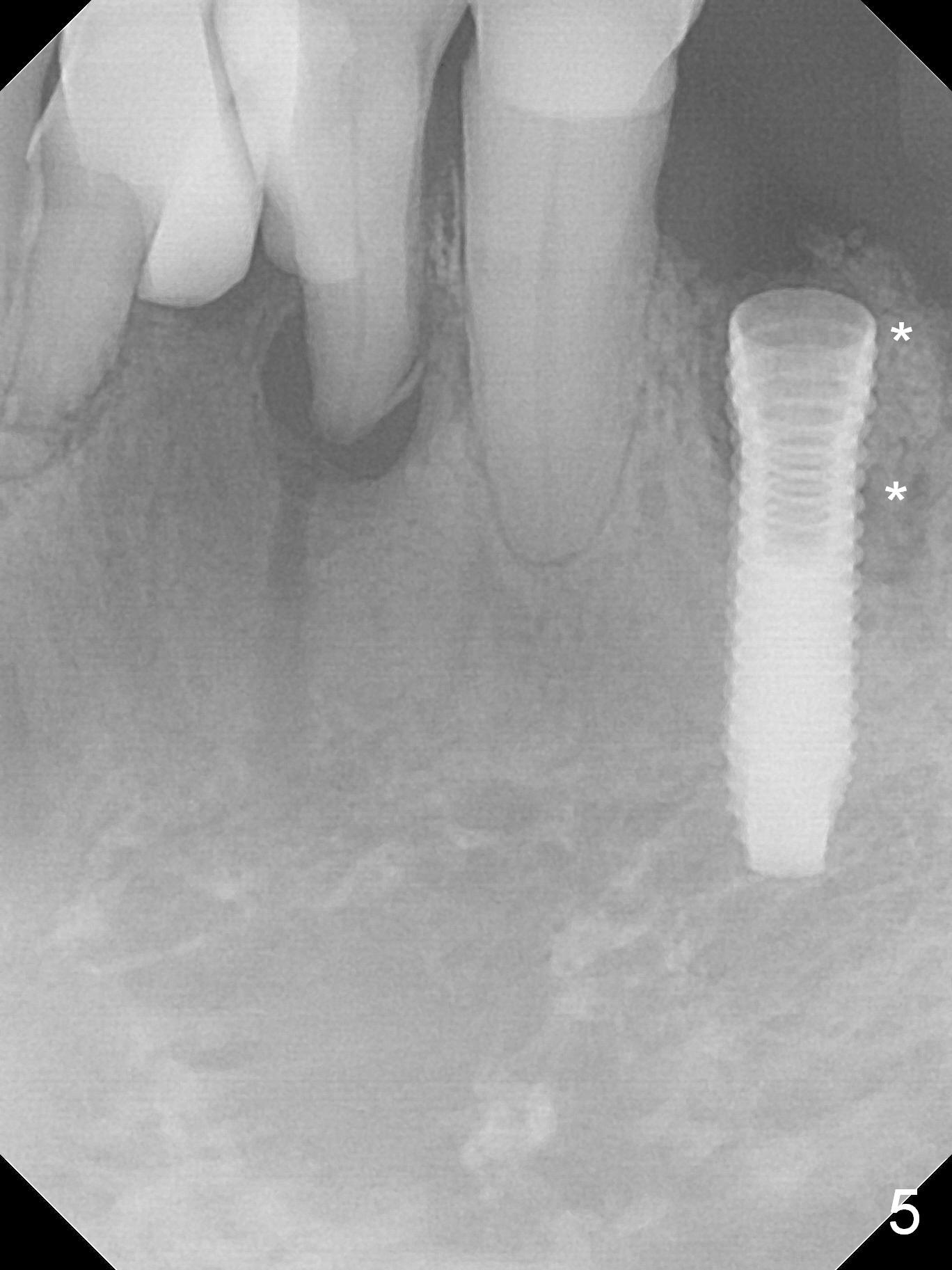
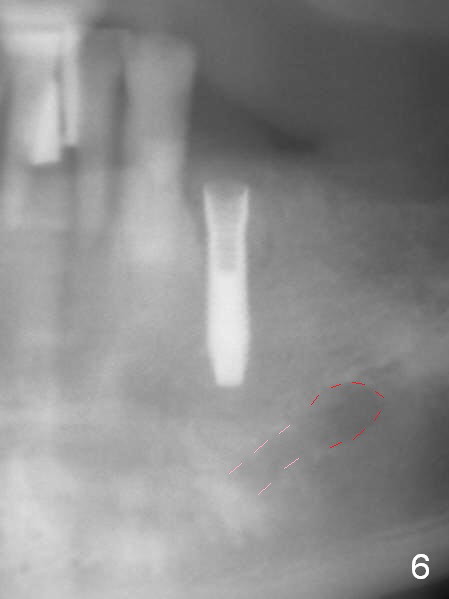
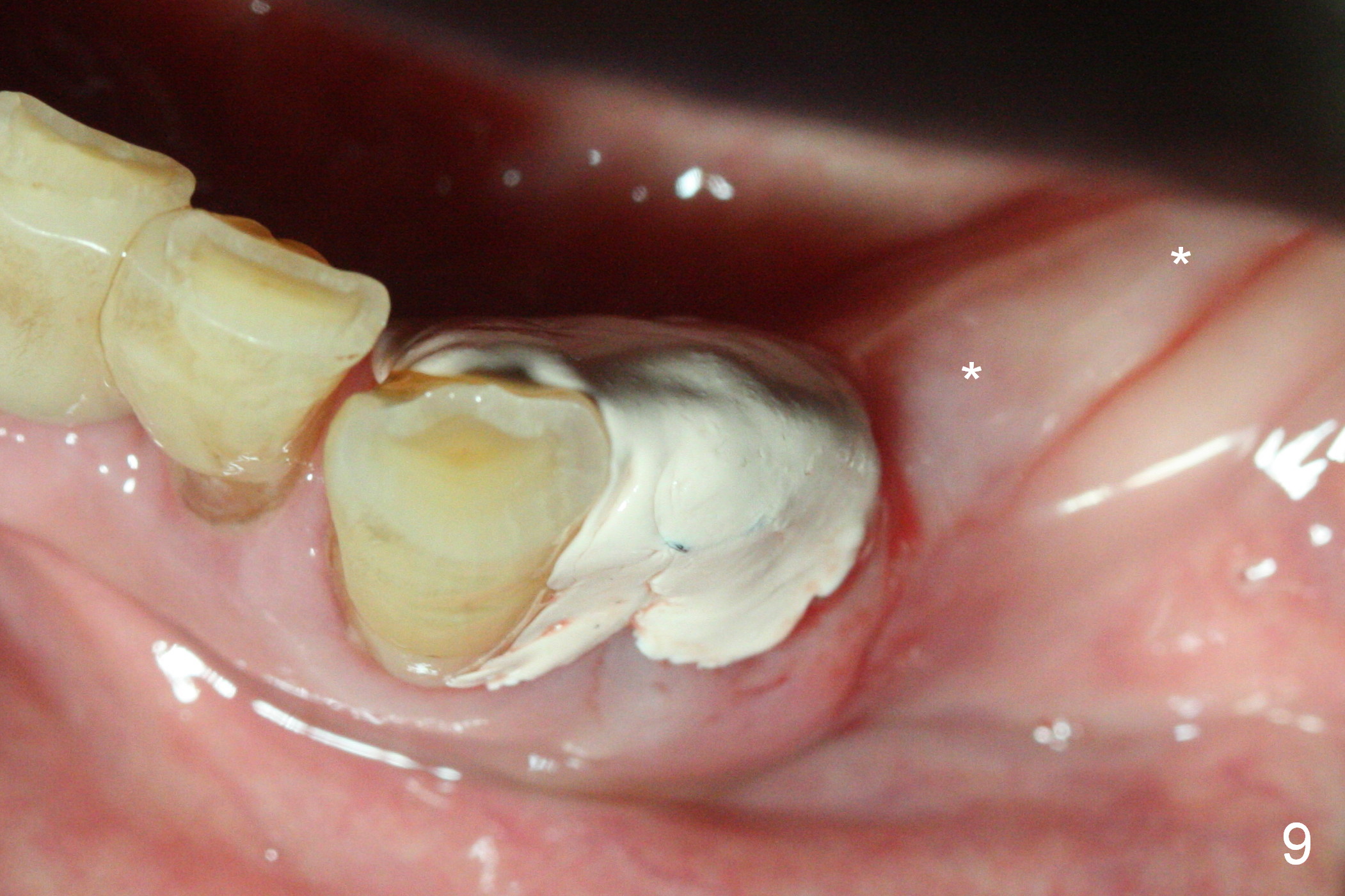
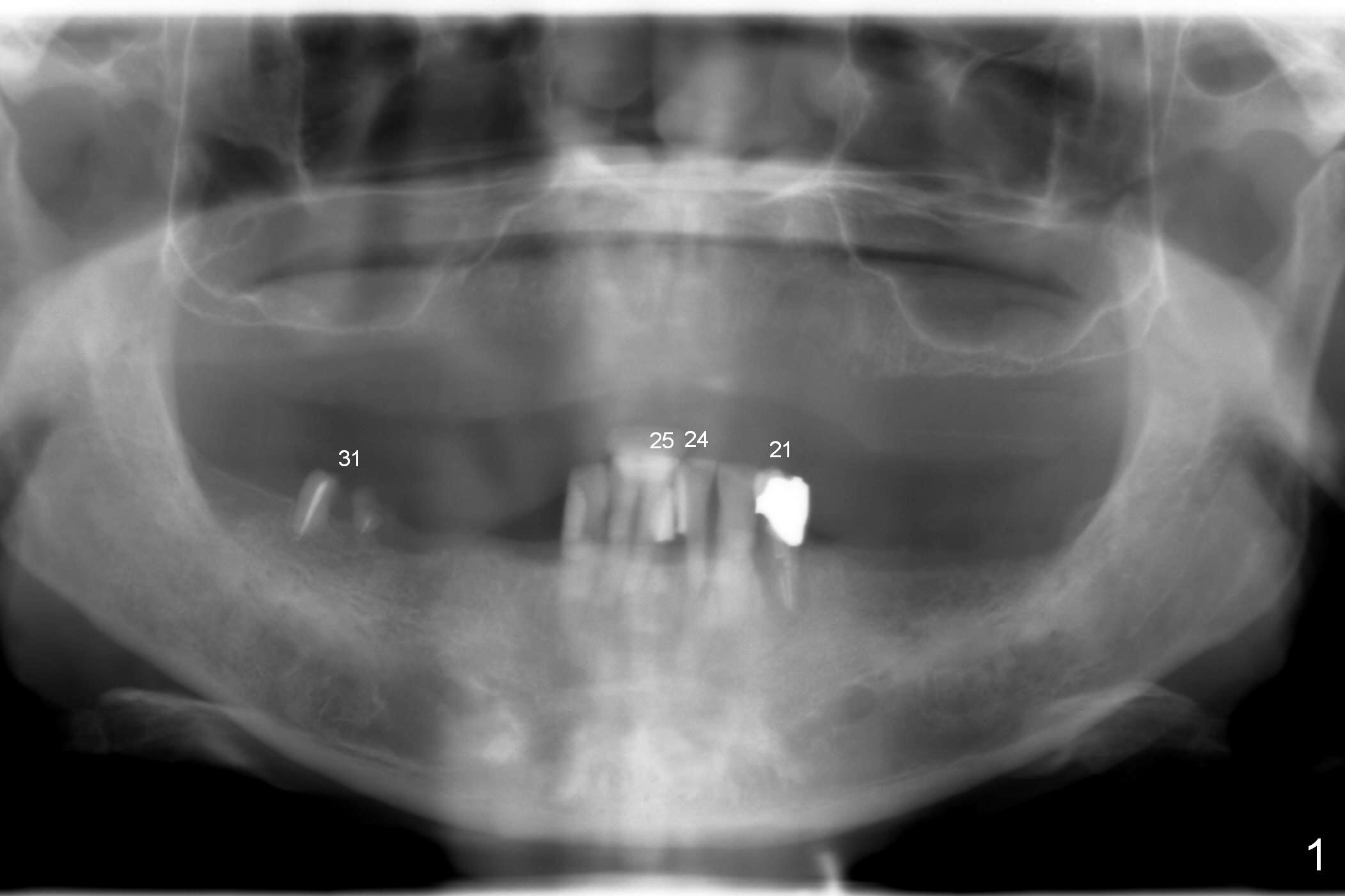
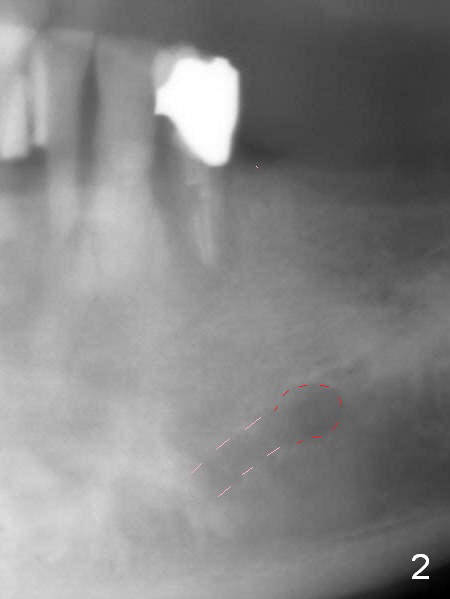
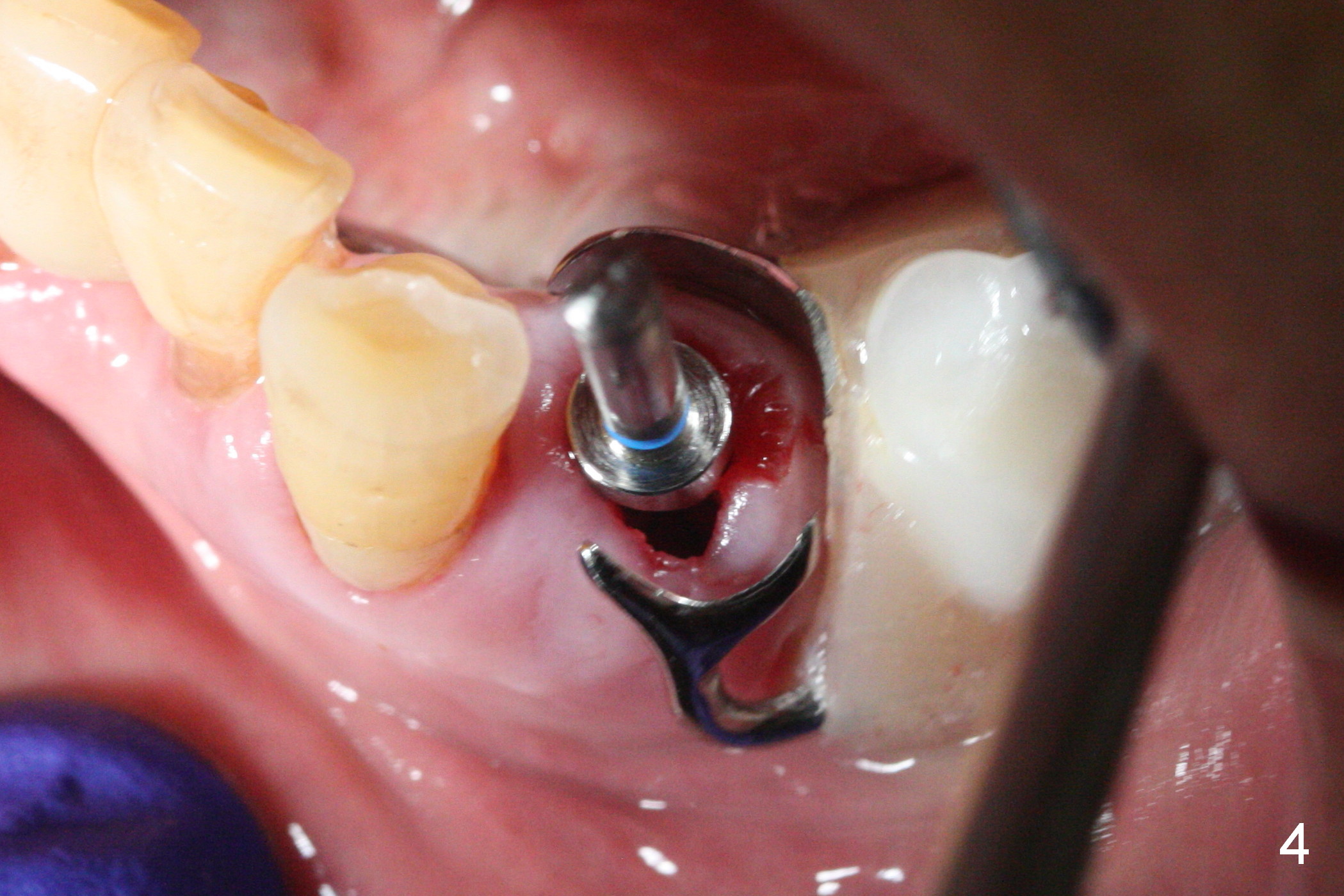
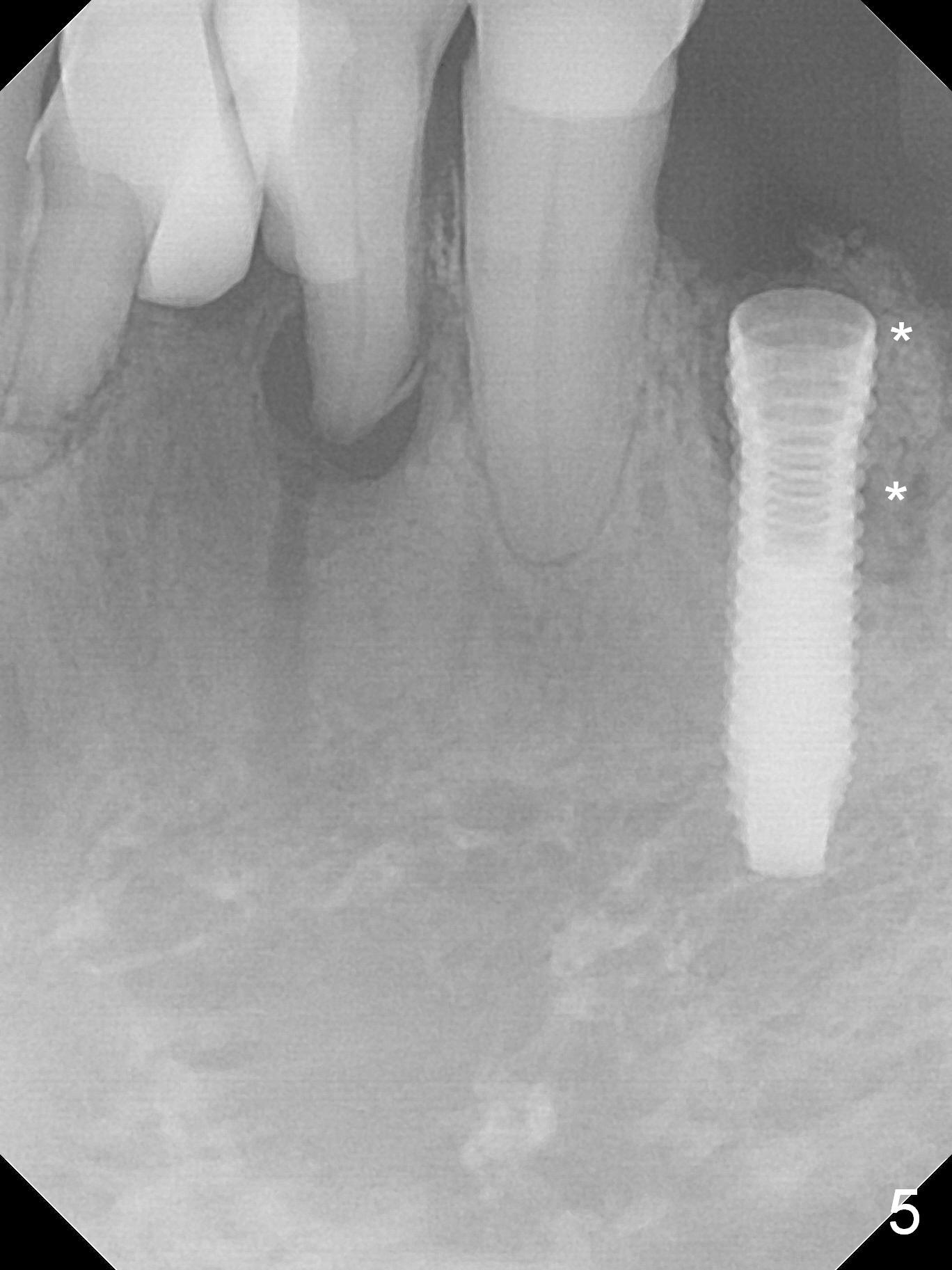
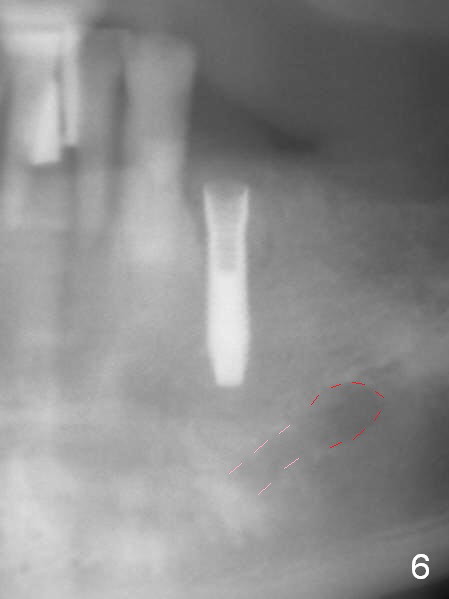
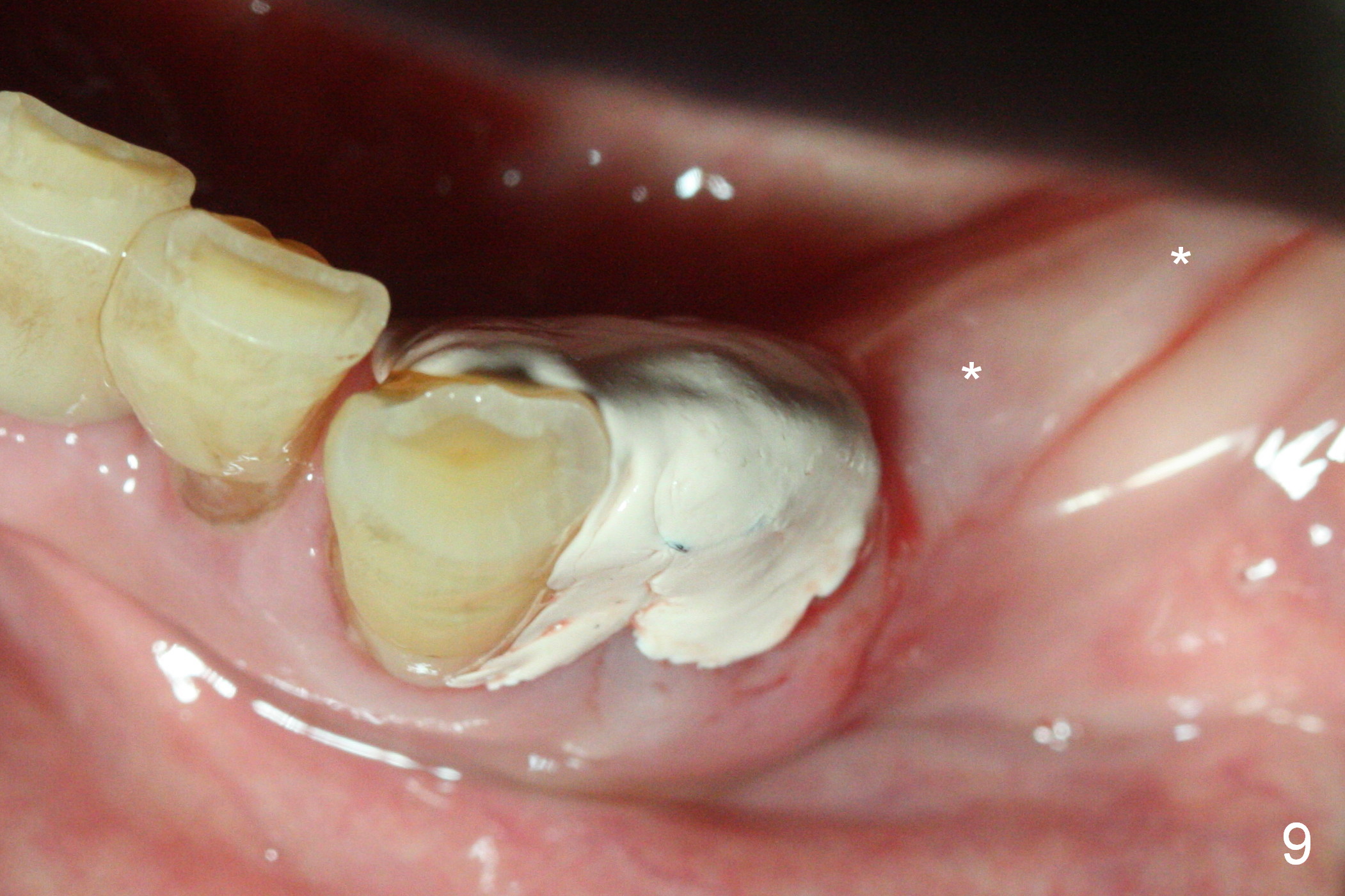
A 72-year-old man presents to clinic for implants because of pain associated with wearing the lower partial. The teeth #21, 24, 25 and 31 seem to be non-salvageable and are going to be replaced by implants so that the lower RPD can be reused (Fig.1). The edentulous ridge is atrophic (Fig.9 *). The upper complete denture appears to be functional. Since the tooth #21 is symptomatic (Fig.2) and the patient has chronic TMJ dislocation, the affected tooth is extracted first (Without antibiotic socket treatment) for immediate implant (Fig.3 (1.5 mm drill (placed more lingually)). The lower RPD is used as a surgical guide (Fig.4 (3 mm drill in place)). When a 3.8x16 mm implant is placed with bone graft (Fig.5 *), the underlying neurovascular bundle is undetected. A small field of panoramic X-ray is retaken; it seems that there is enough clearance from the Mental Foramen (Fig.2,6,7 (red dashed line)) and the Incisive Canal (pink dashed line). The implant is then placed 2 mm more apically (Fig.7) to reduce the chance of periimplantitis since the buccal plate is lost. A 5.5x5(5) mm abutment is placed (Fig.5) with more graft. The access of the abutment is left open so that a part of periodontal dressing is inserted for additional retention (Fig.8,9). The RPD is placed back for adaptation of the dressing. The patient is advised not to wear the RPD postop to reduce micromovement.
The patient returns 2 days postop because of hemorrhage (Fig.10,11 * after removal of loose periodontal dressing). Periodontal dressing is repacked (Fig.12). The hemorrhage may be due to incomplete removal of granulation tissue or invasion of the Incisive vessel intraoperatively, although there is no pain or paresthesia postop. Soft food is recommended without the upper complete denture. A provisional is fabricated (Fig.14 P) nearly 3 months postop (after changing the 5.5x5(5) mm abutment to 4.5x5(4) mm, Fig.13) when an implant is being place is #31.
Return to
Lower Premolar
Immediate Implant, IBS,
Improvement,
#23/25
Xin Wei, DDS, PhD, MS 1st edition 01/03/2017, last revision 07/04/2017