.jpg)






 |
 |
.jpg) |
 |
 |
|
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
||||
Depth First M
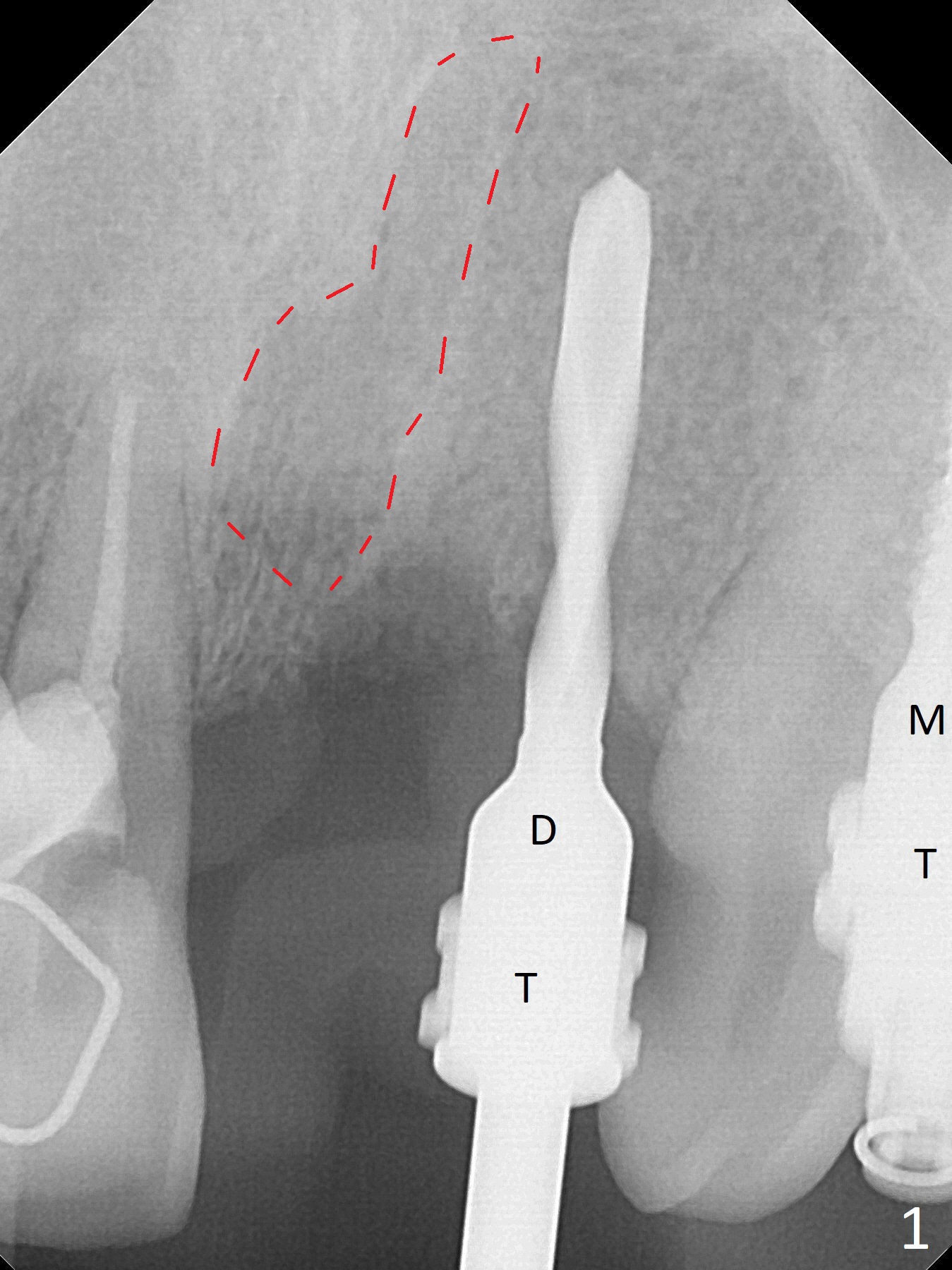
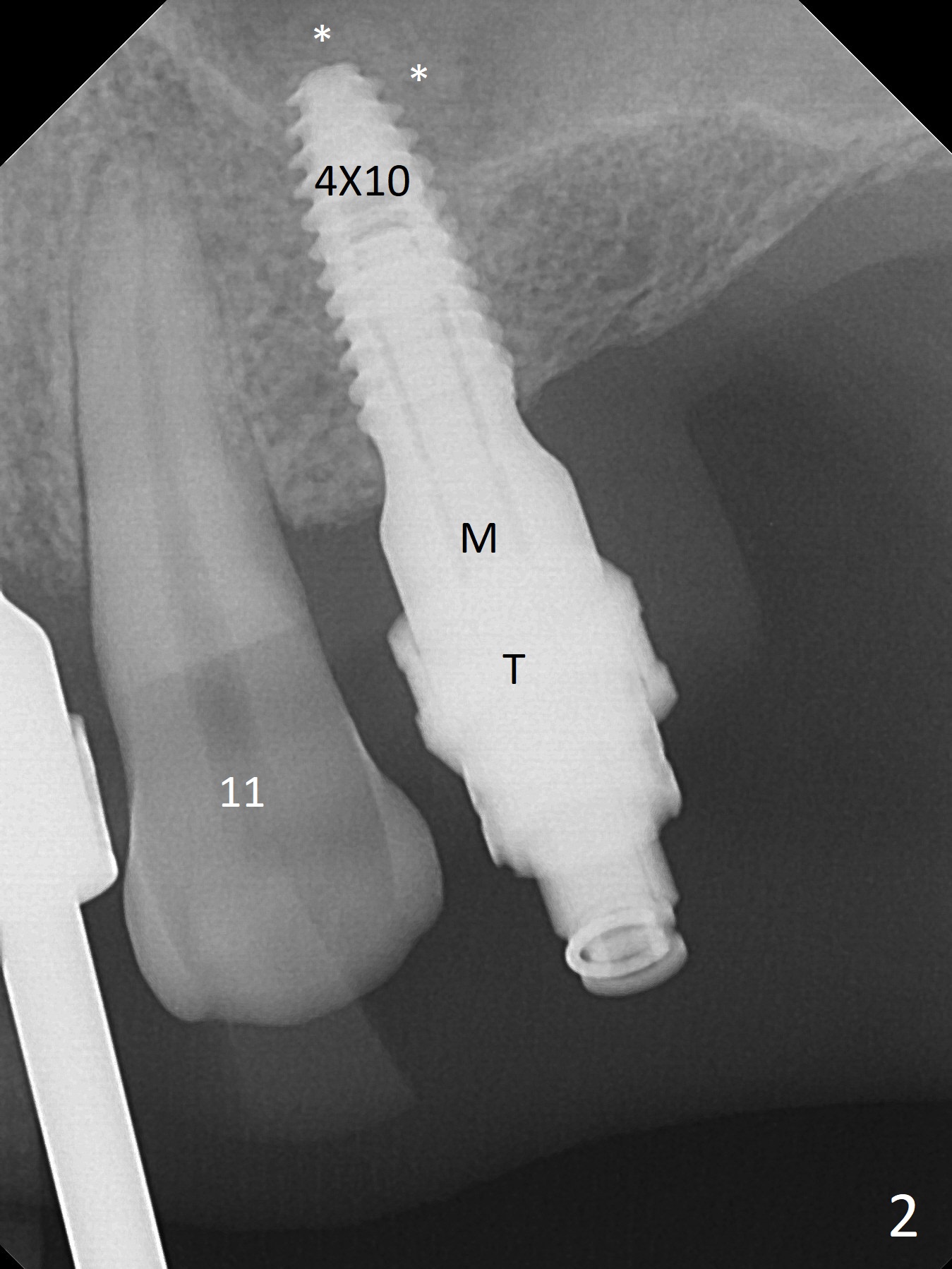
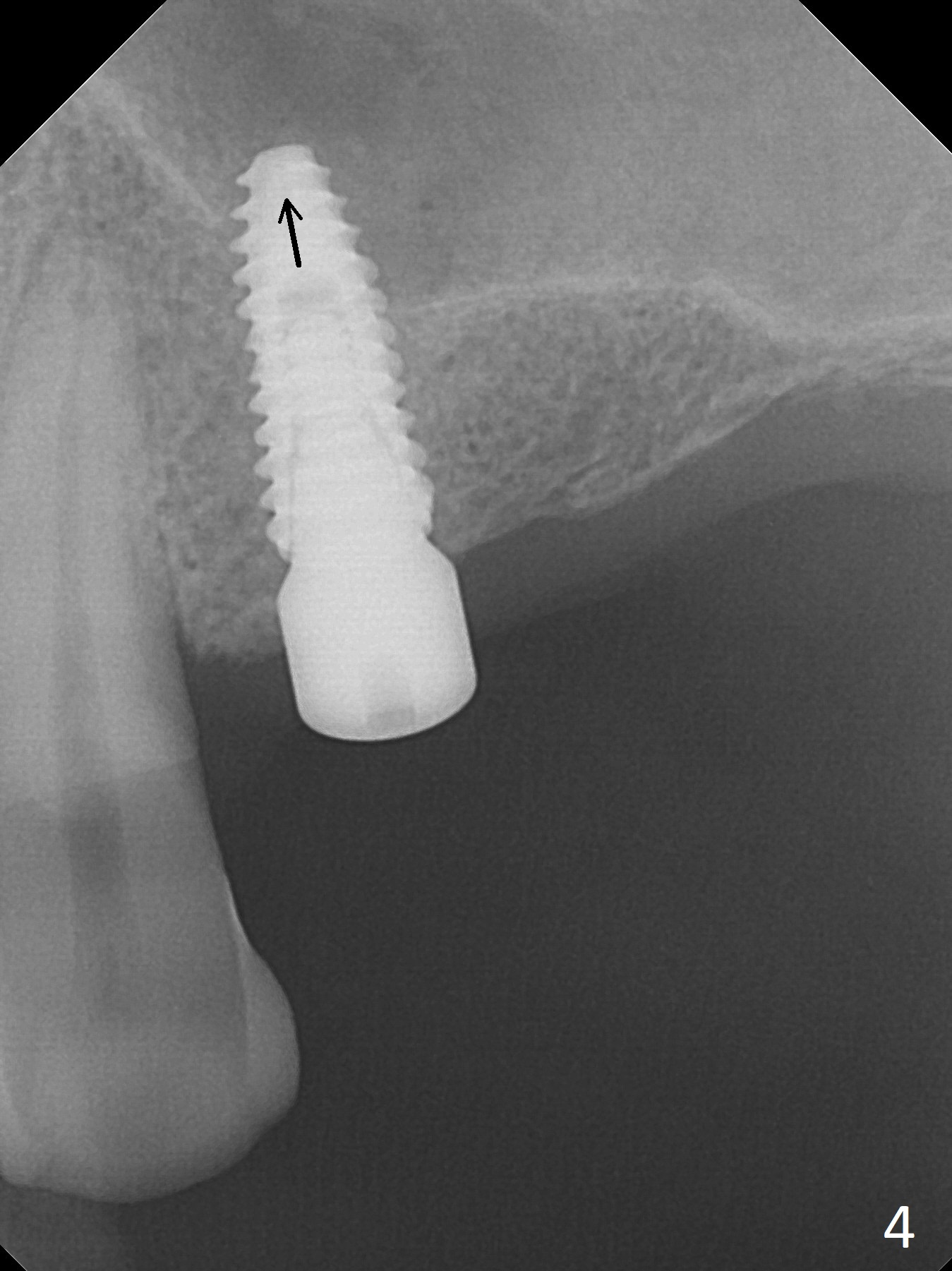
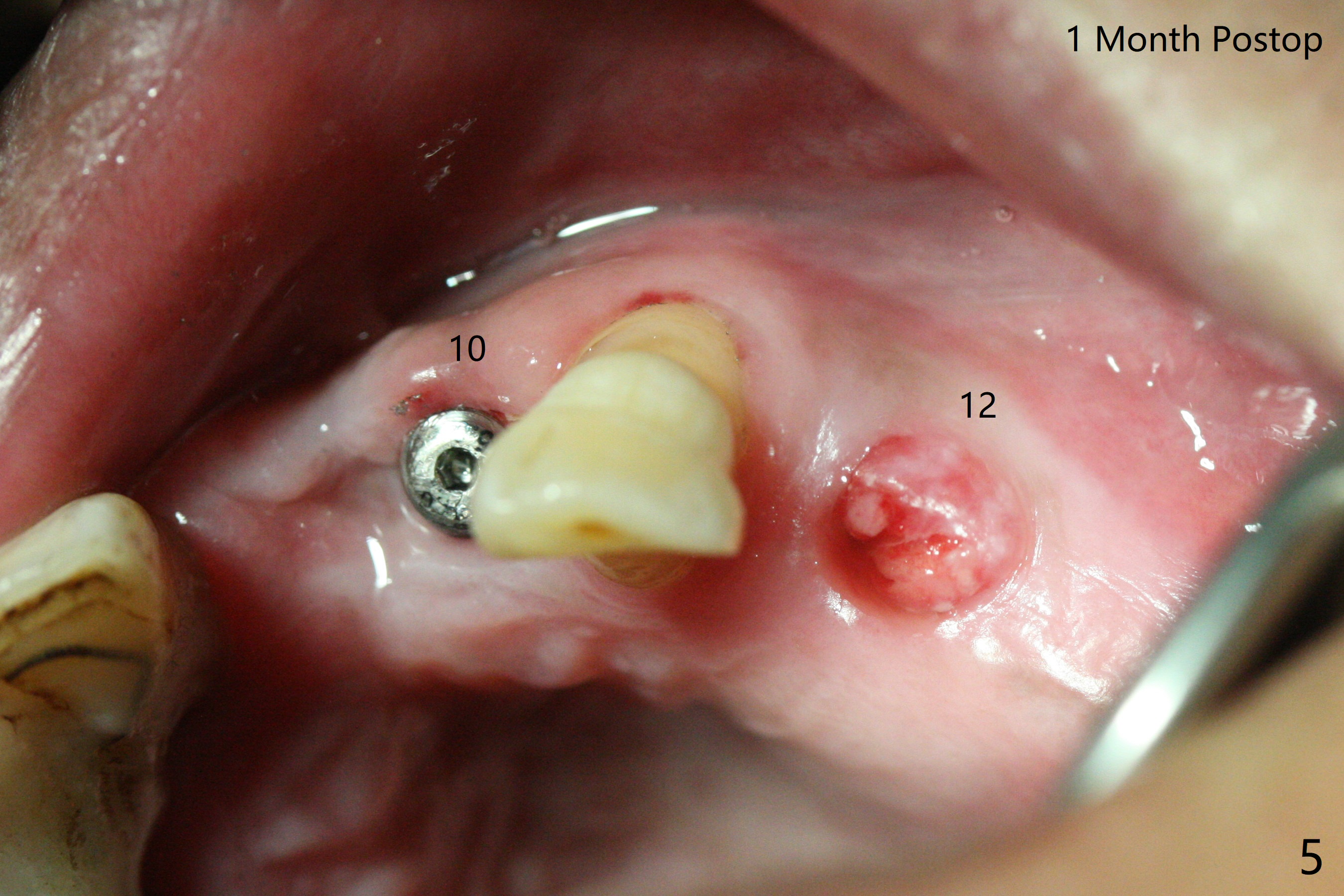
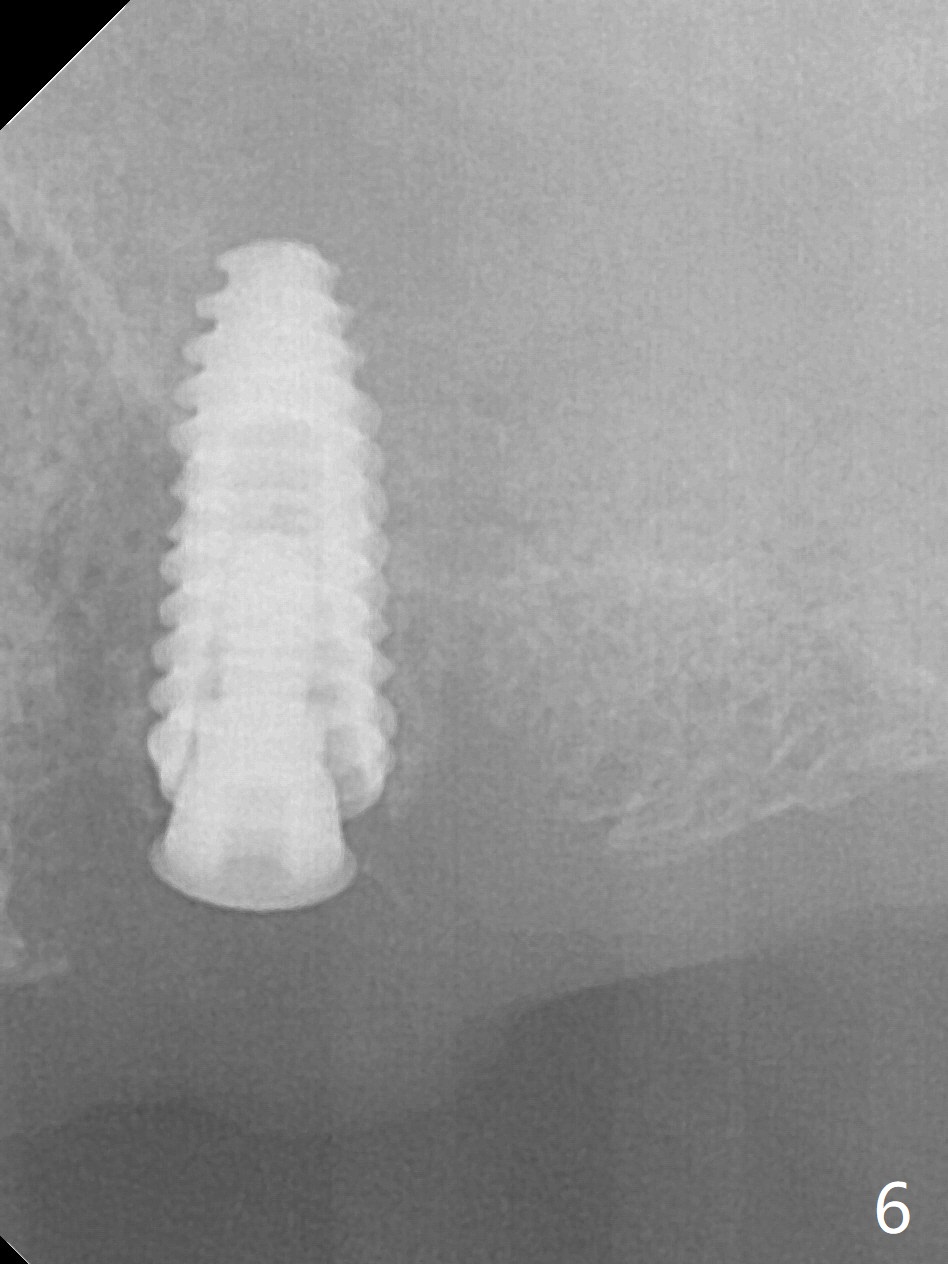
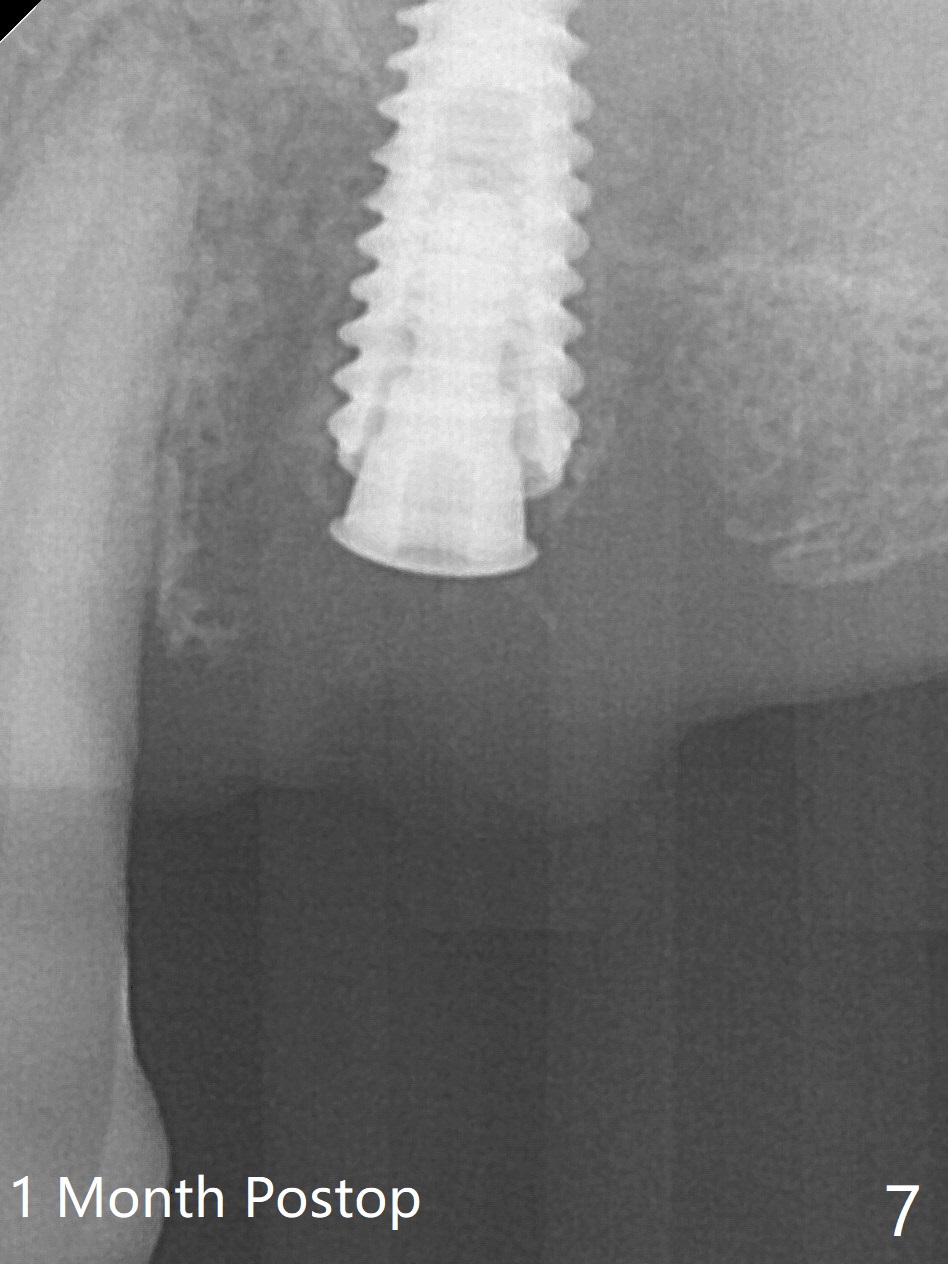
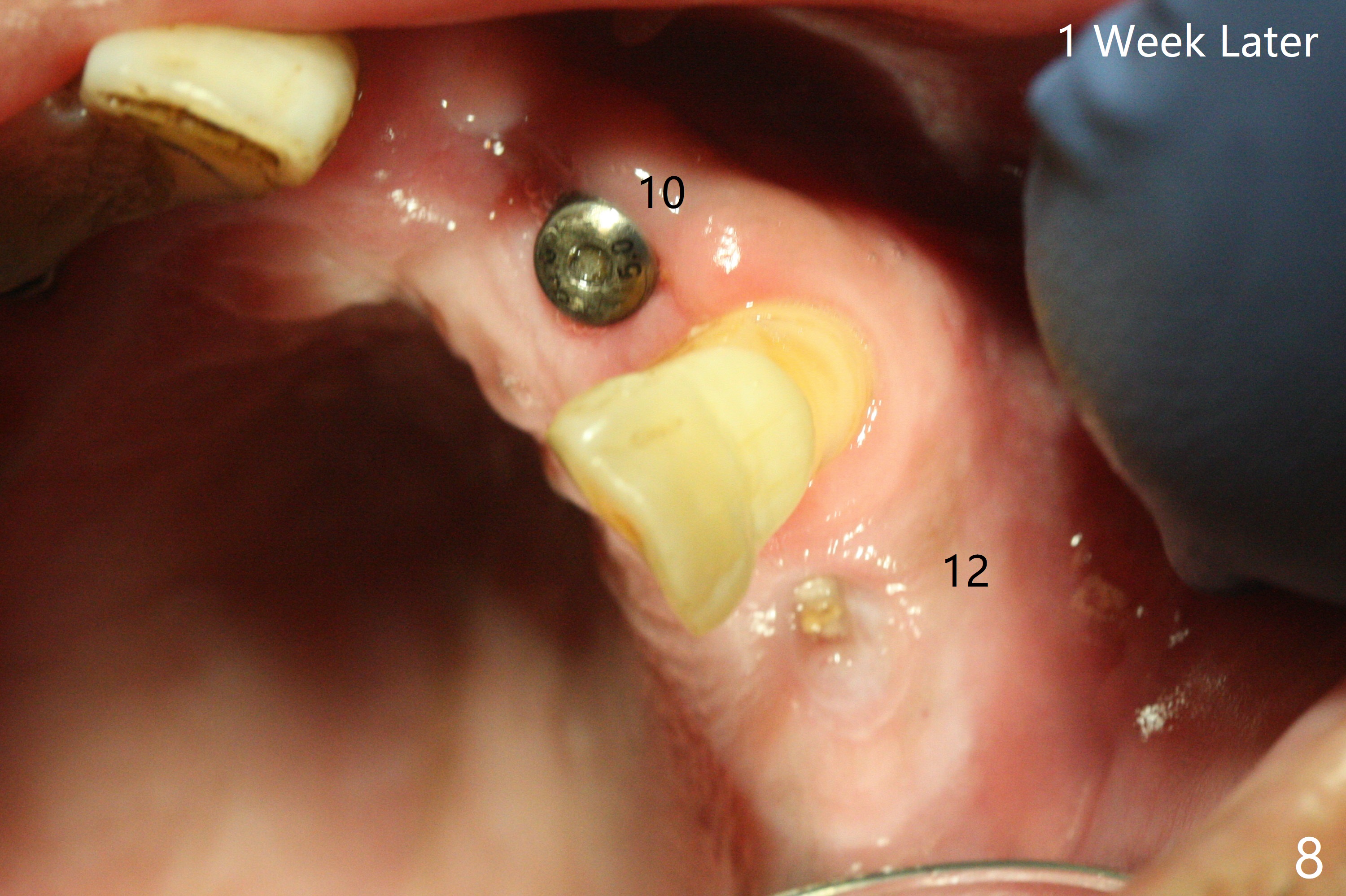
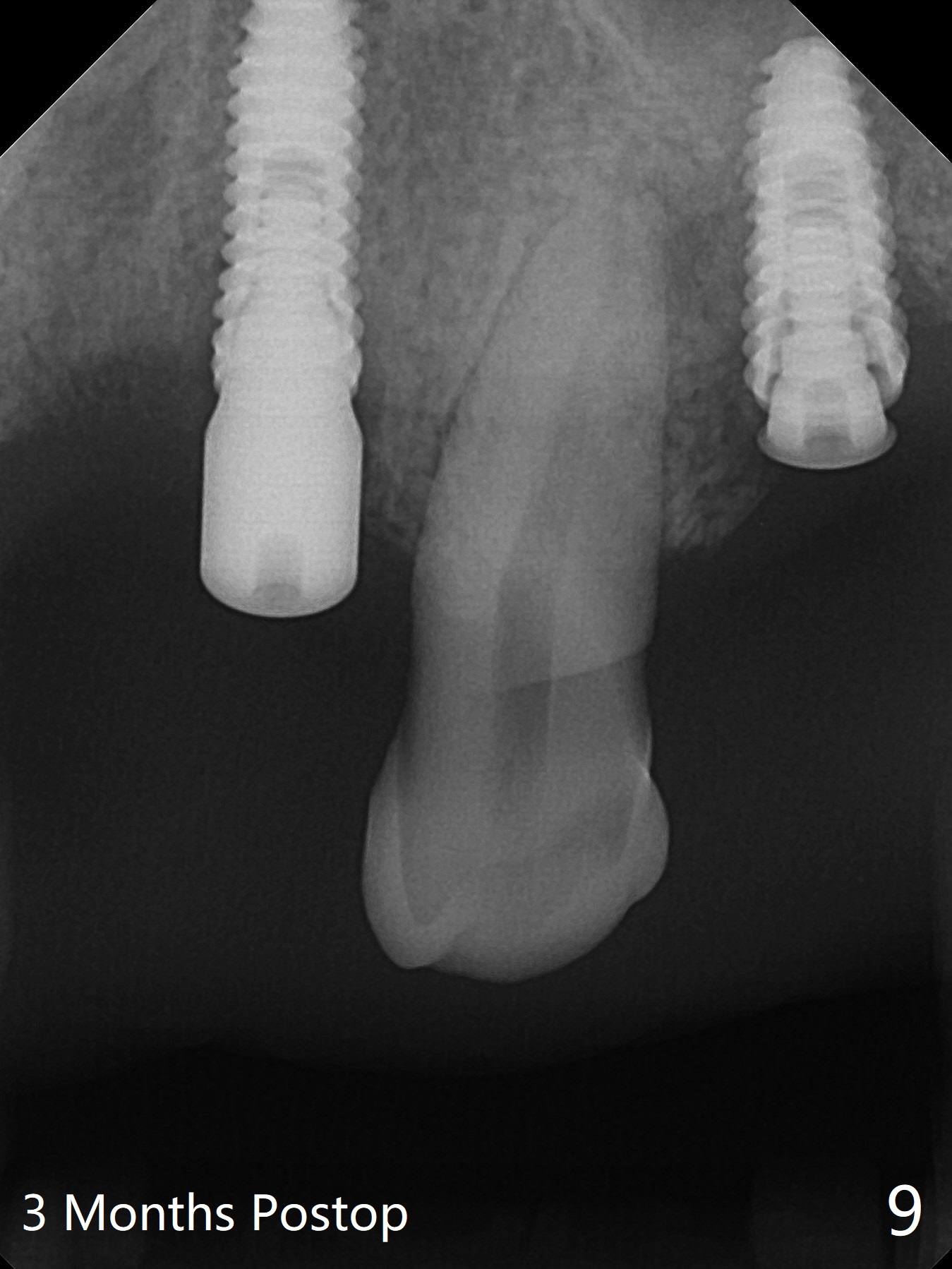
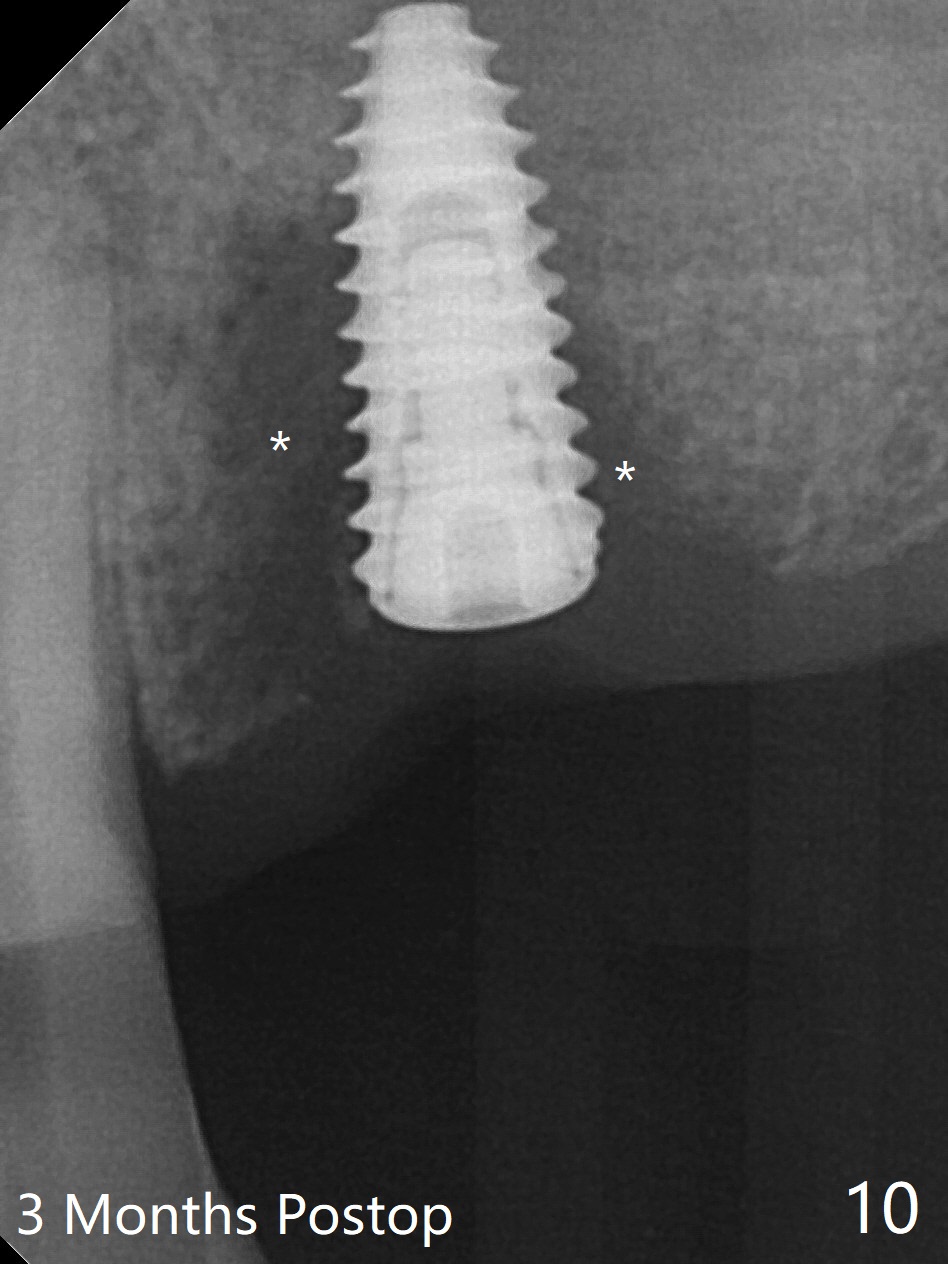
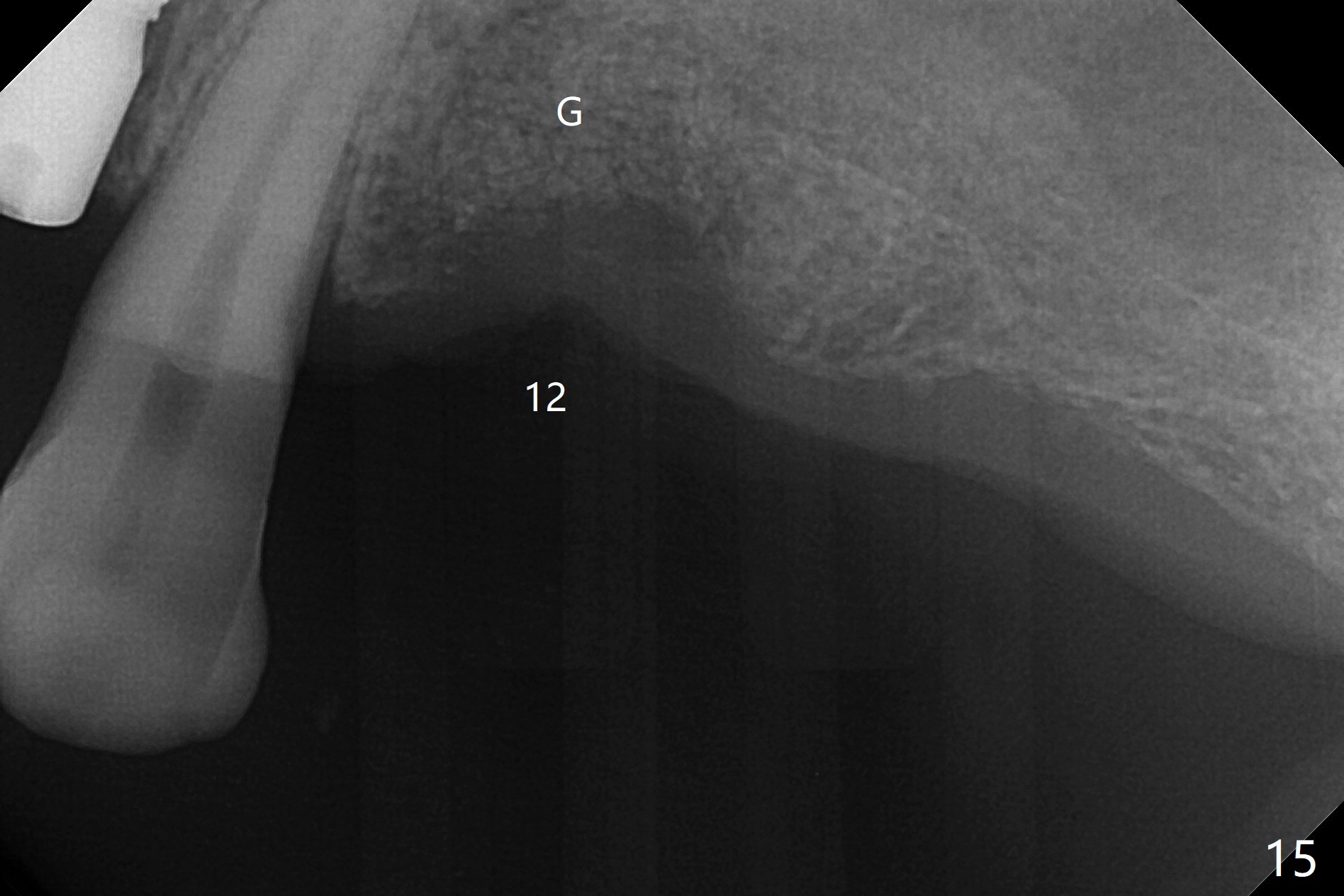
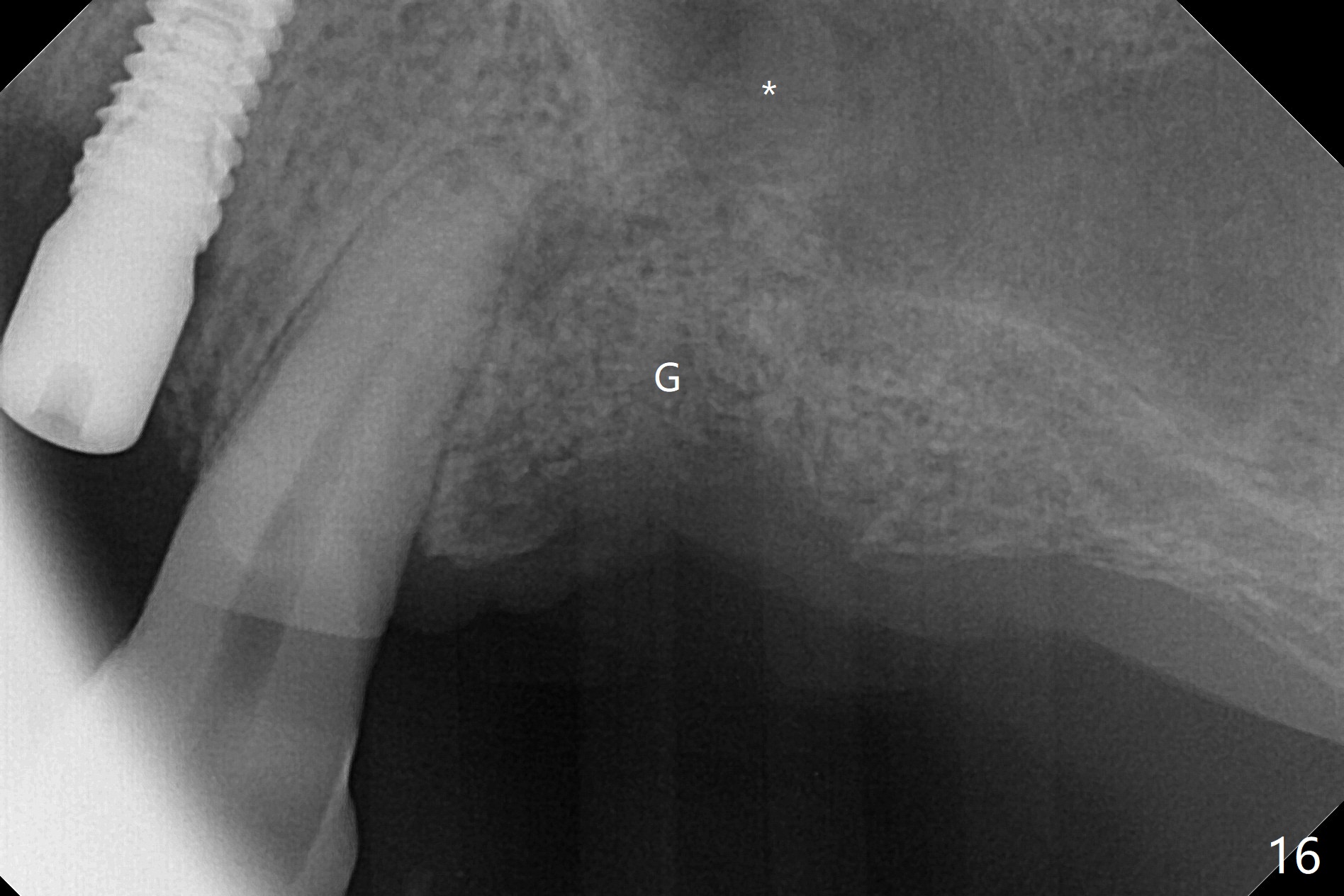
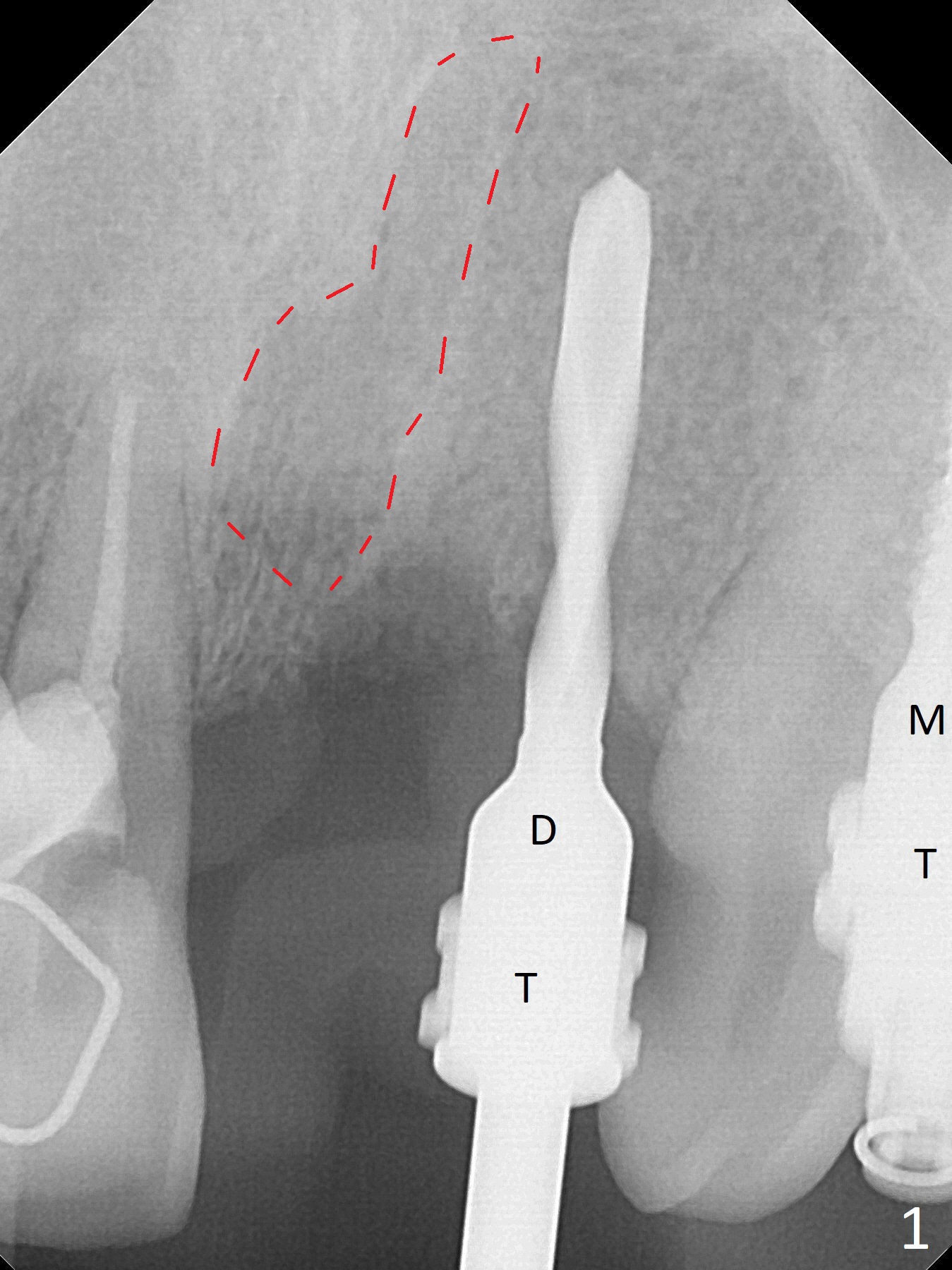
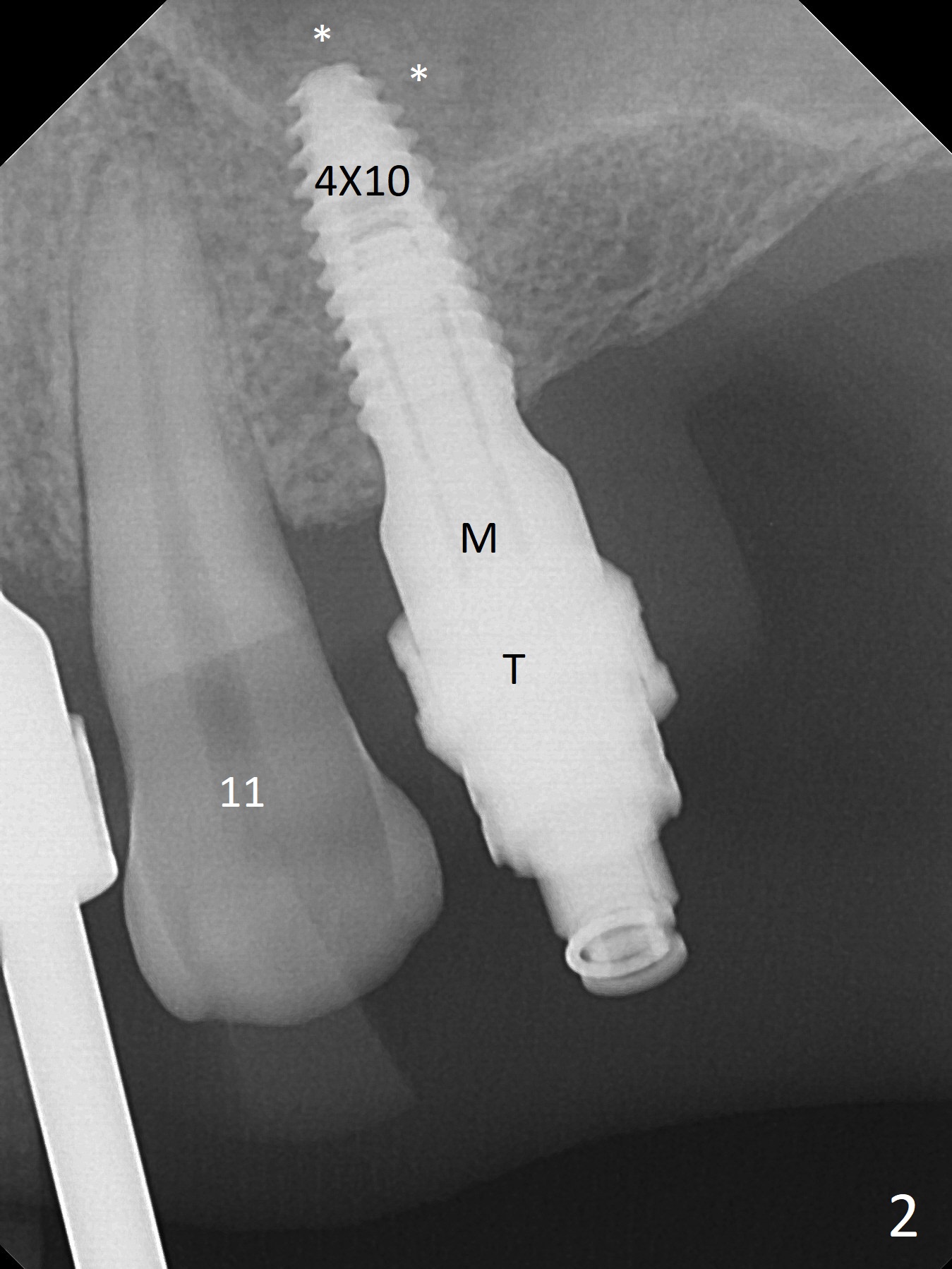
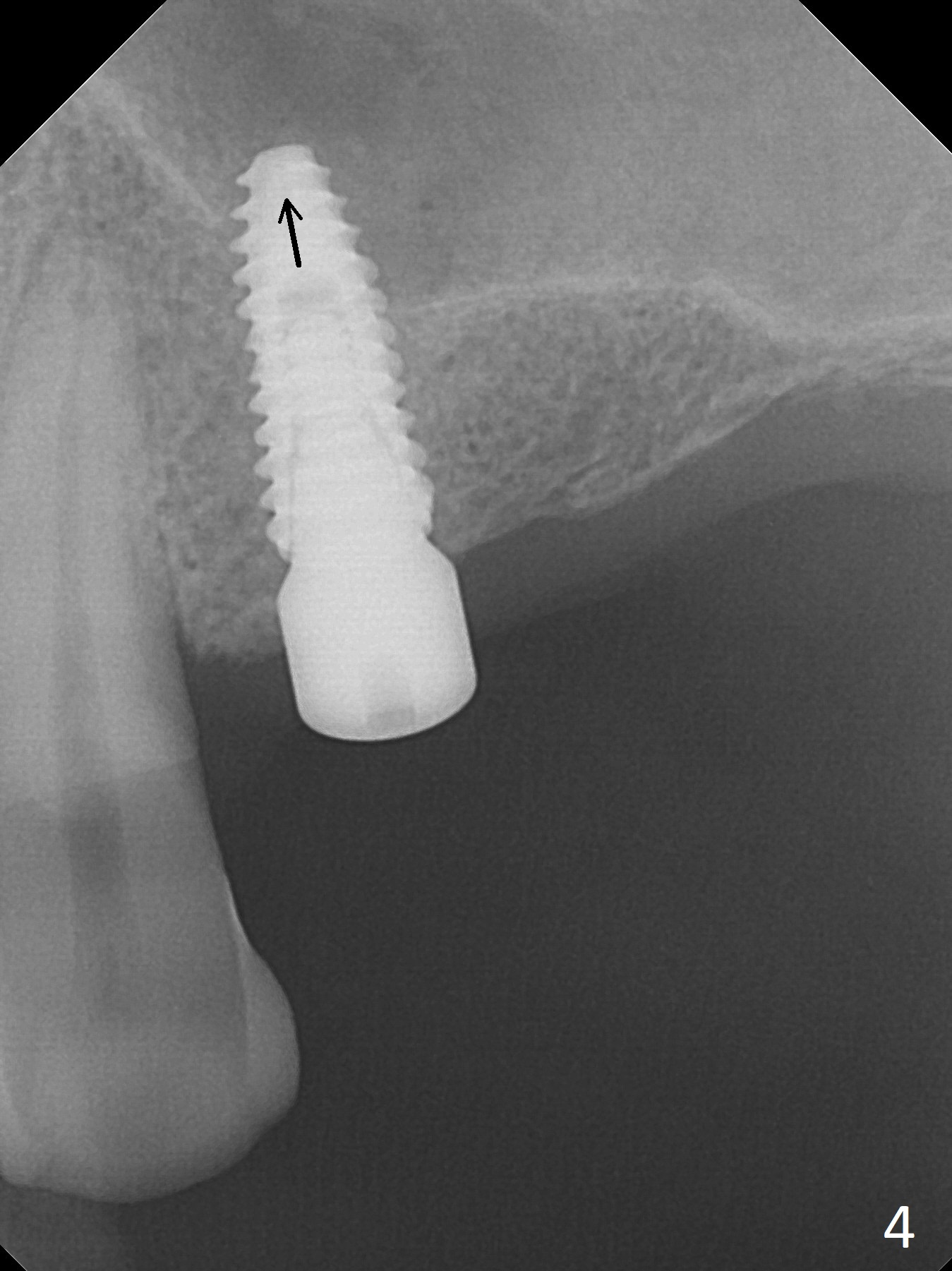
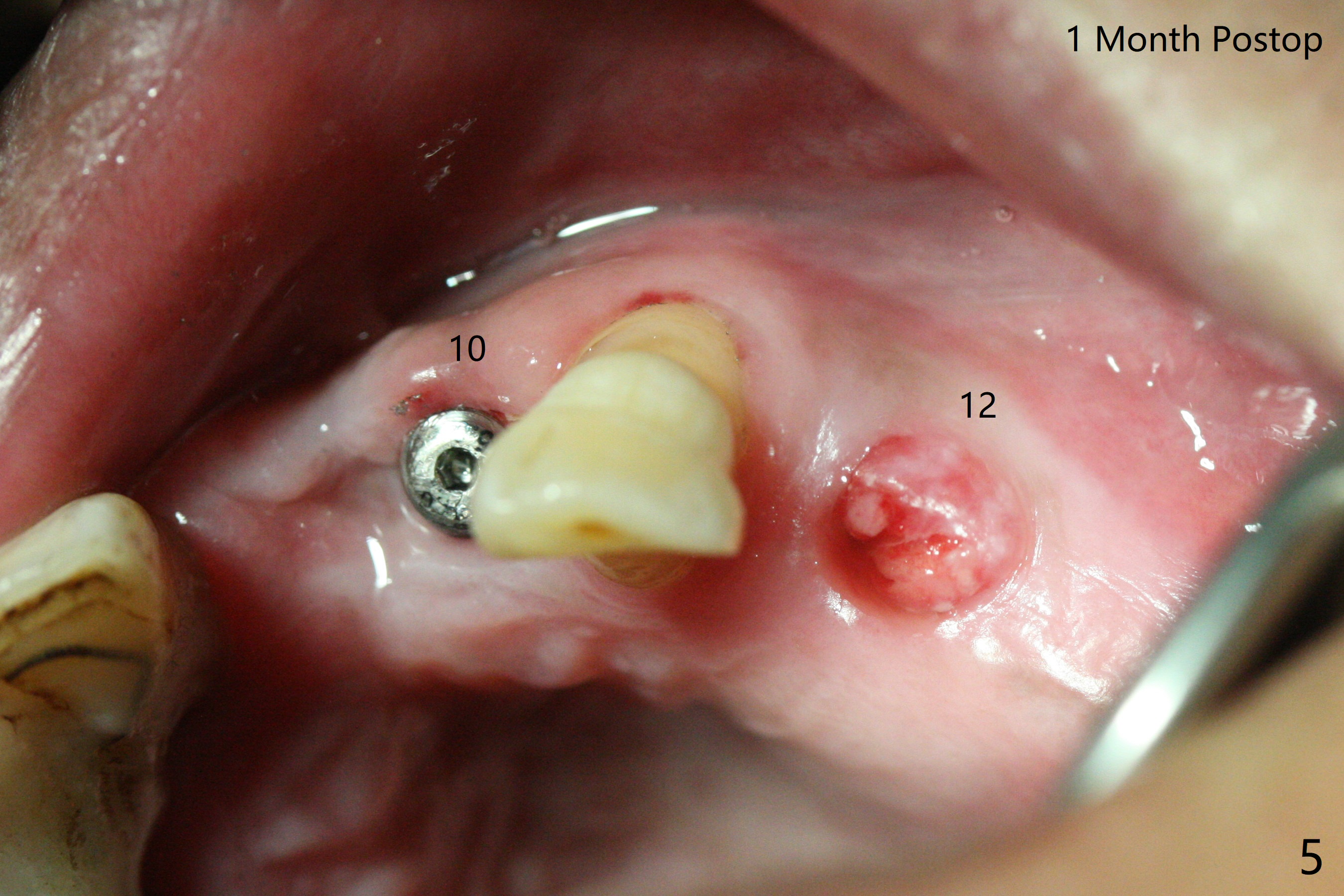
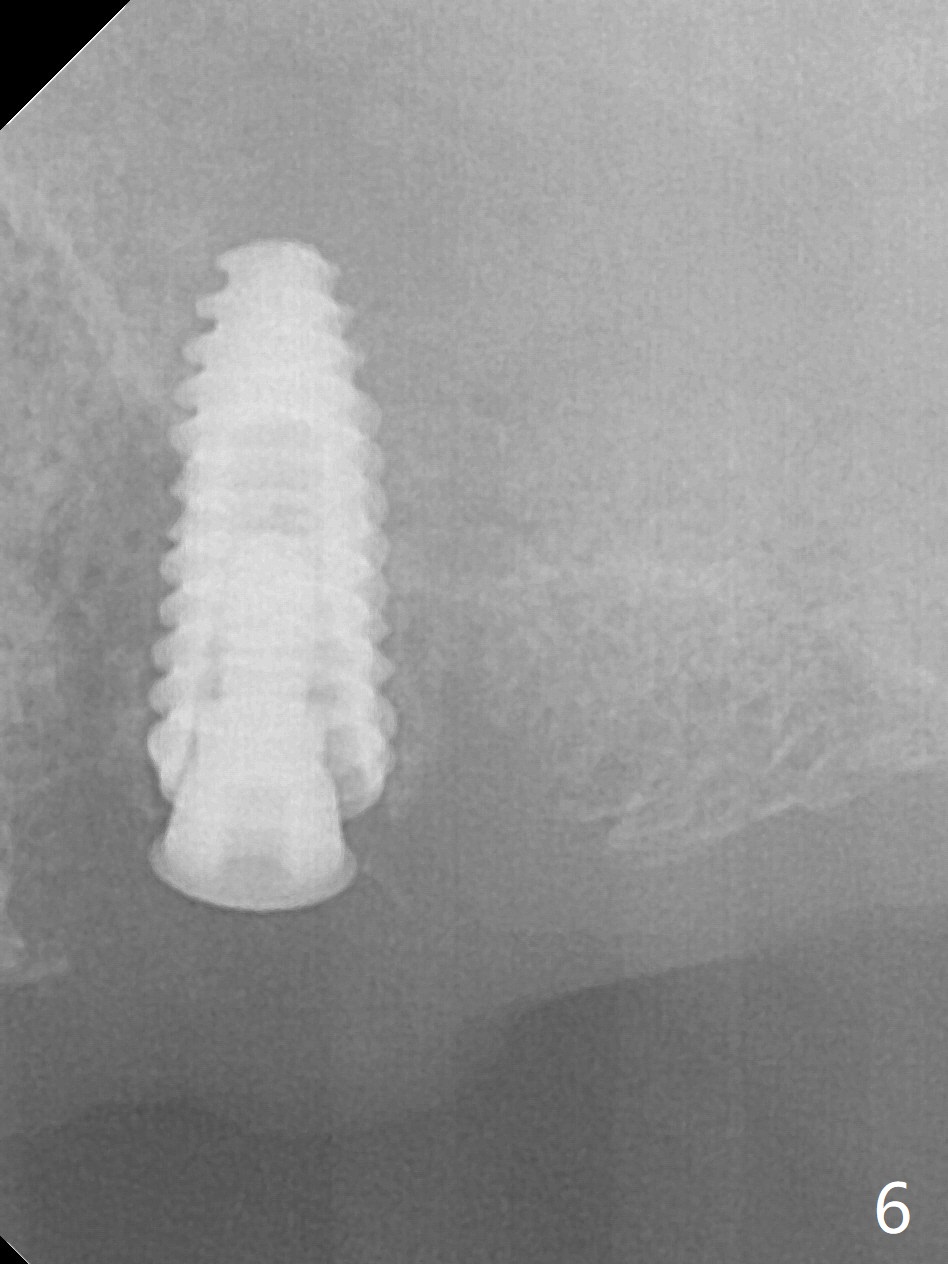
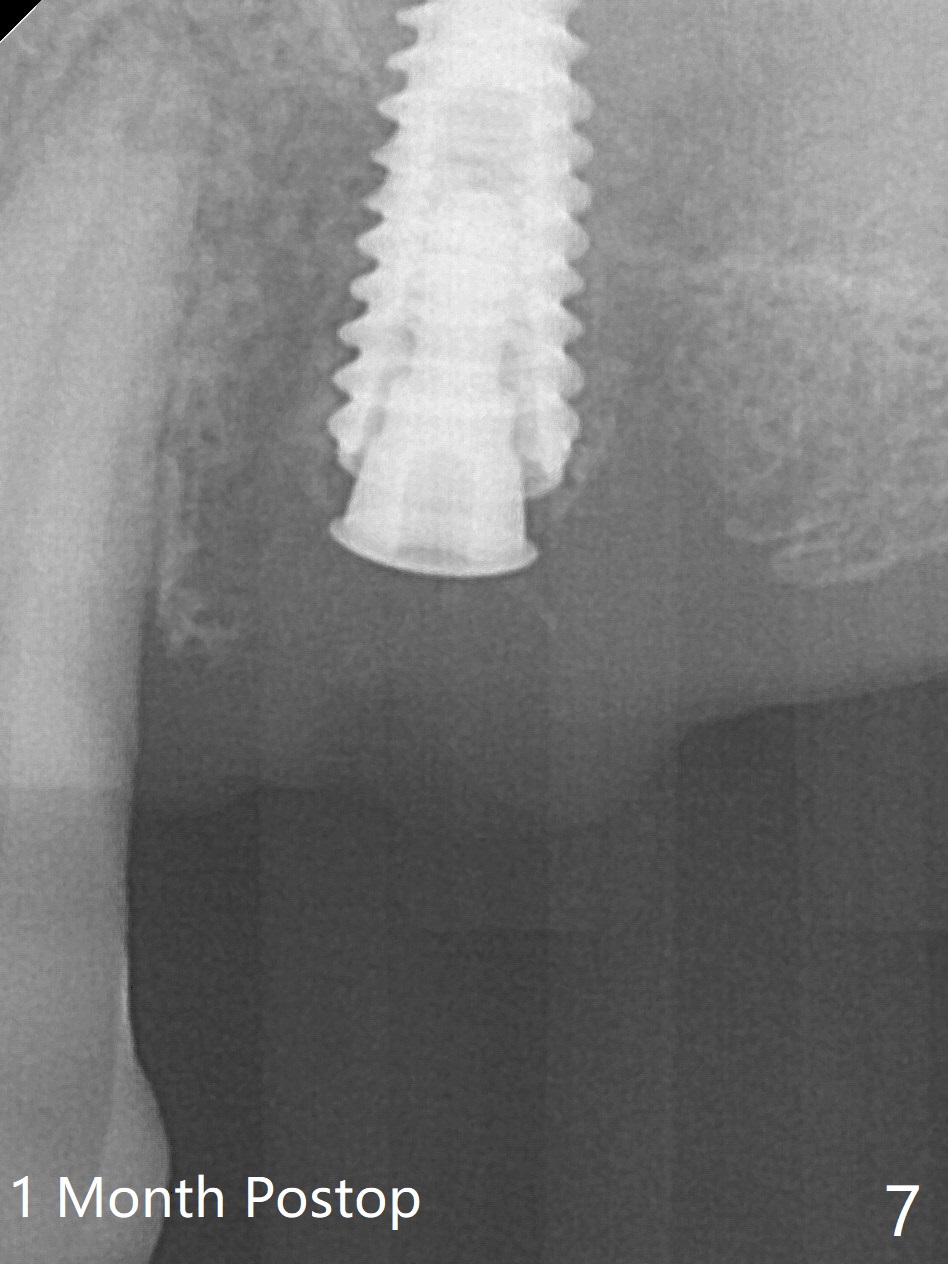
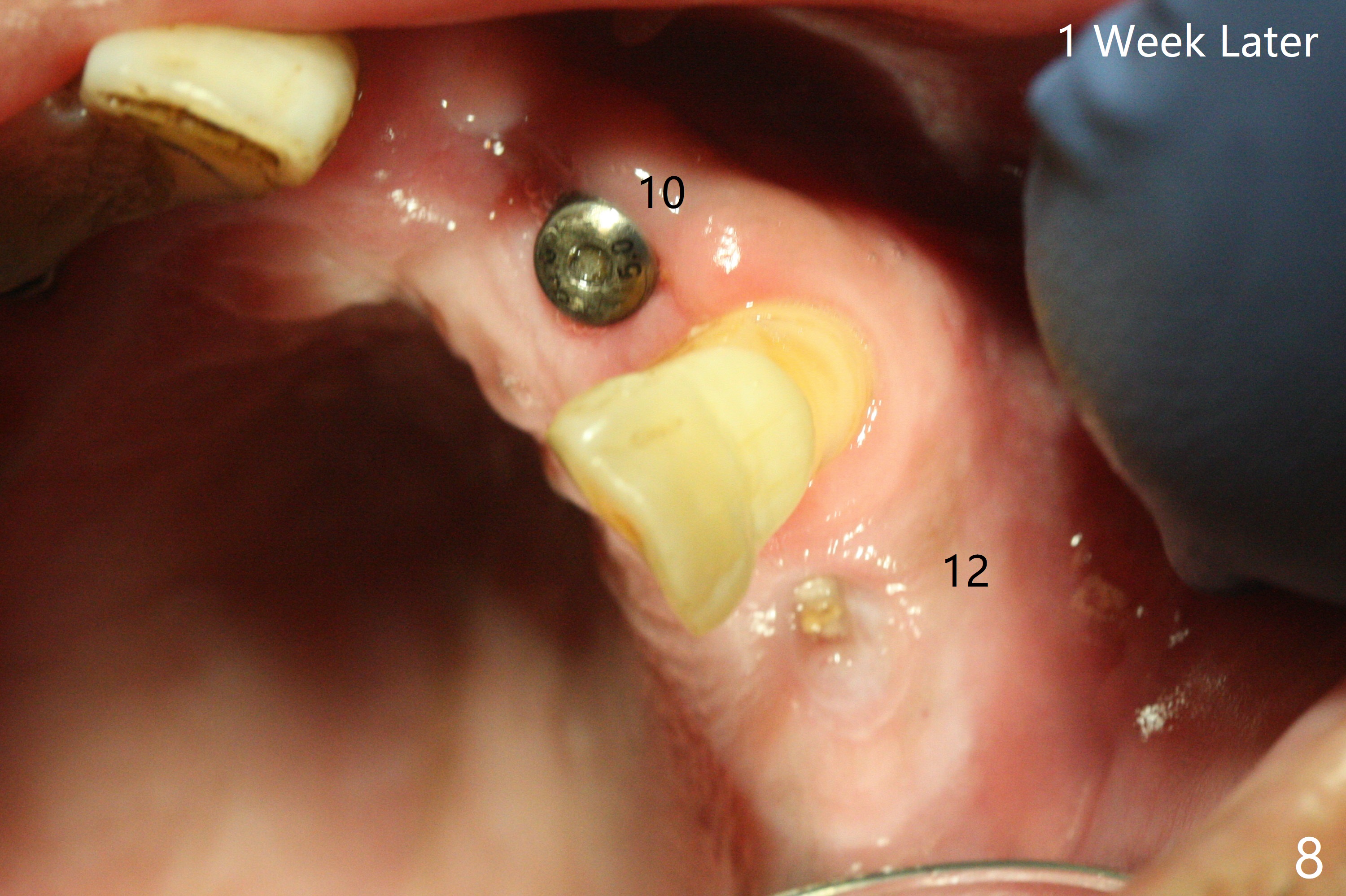
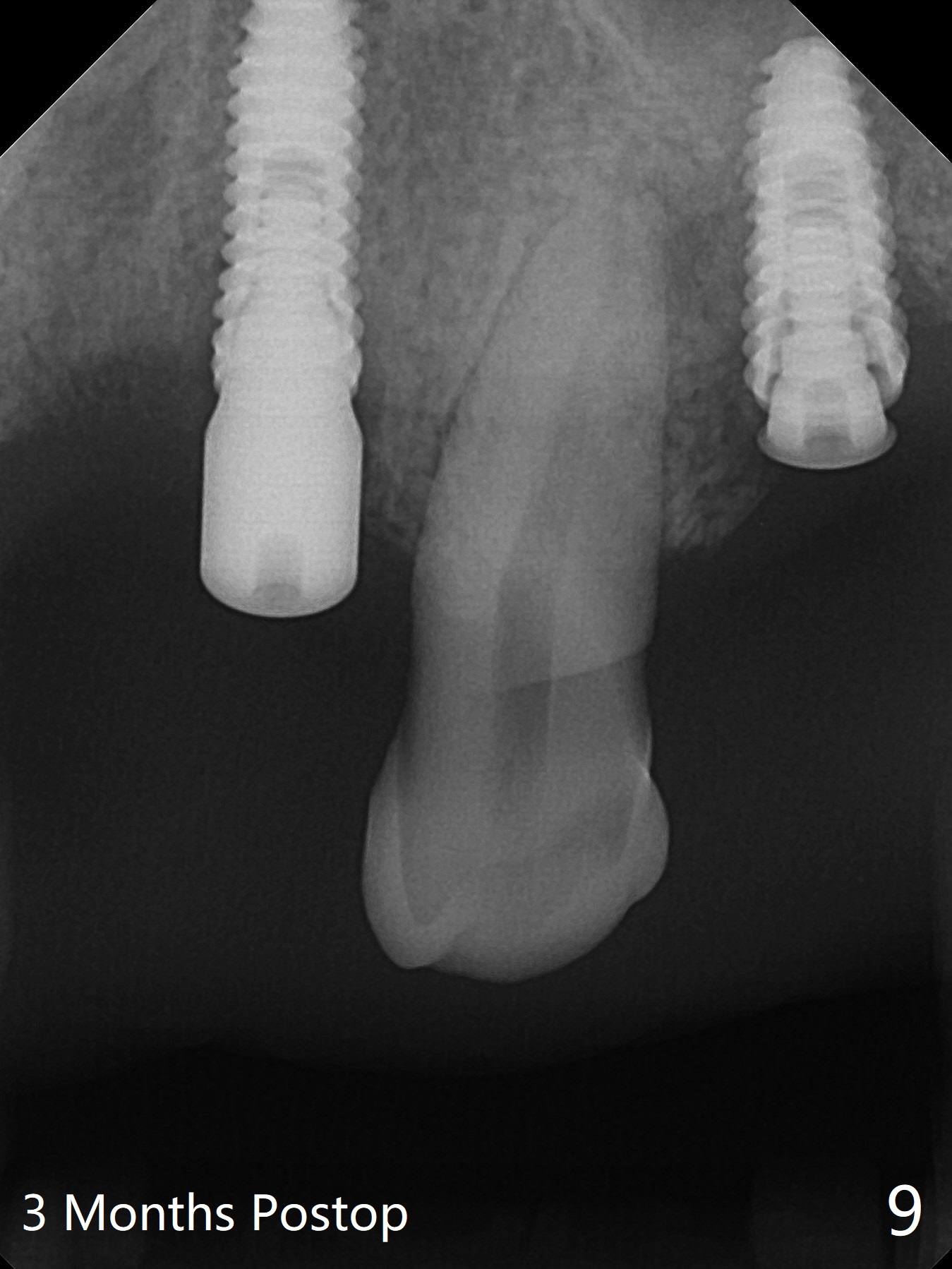
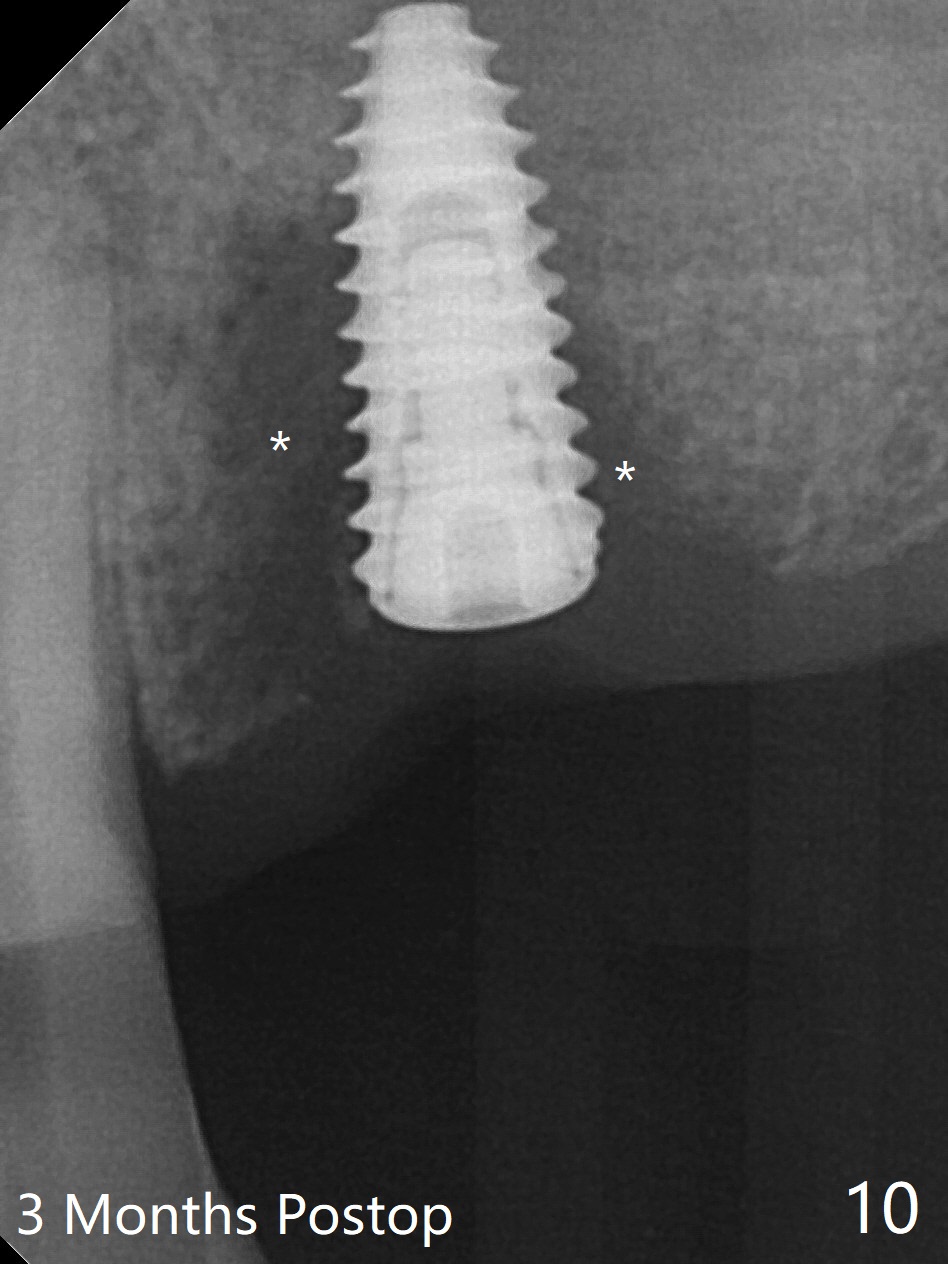
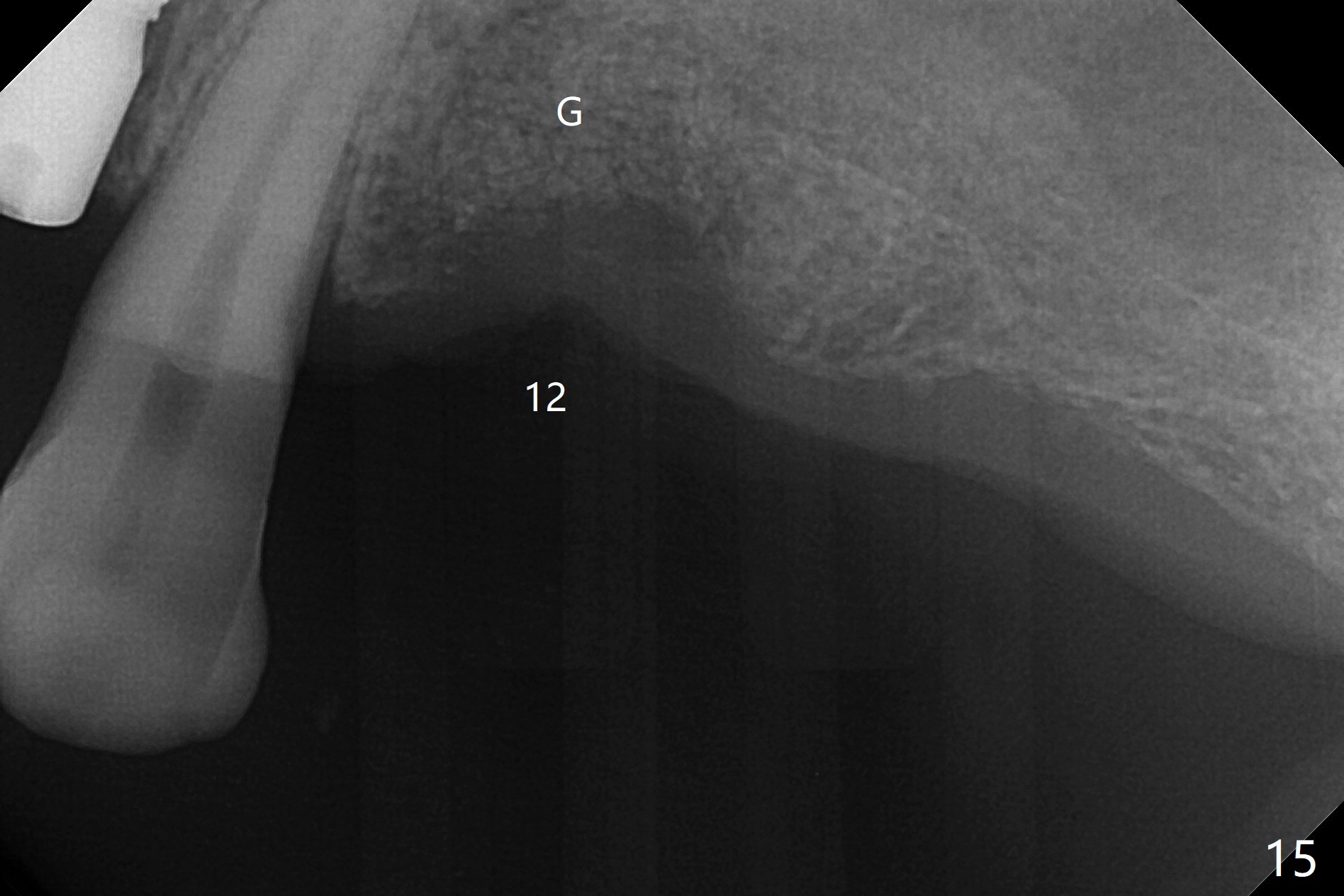
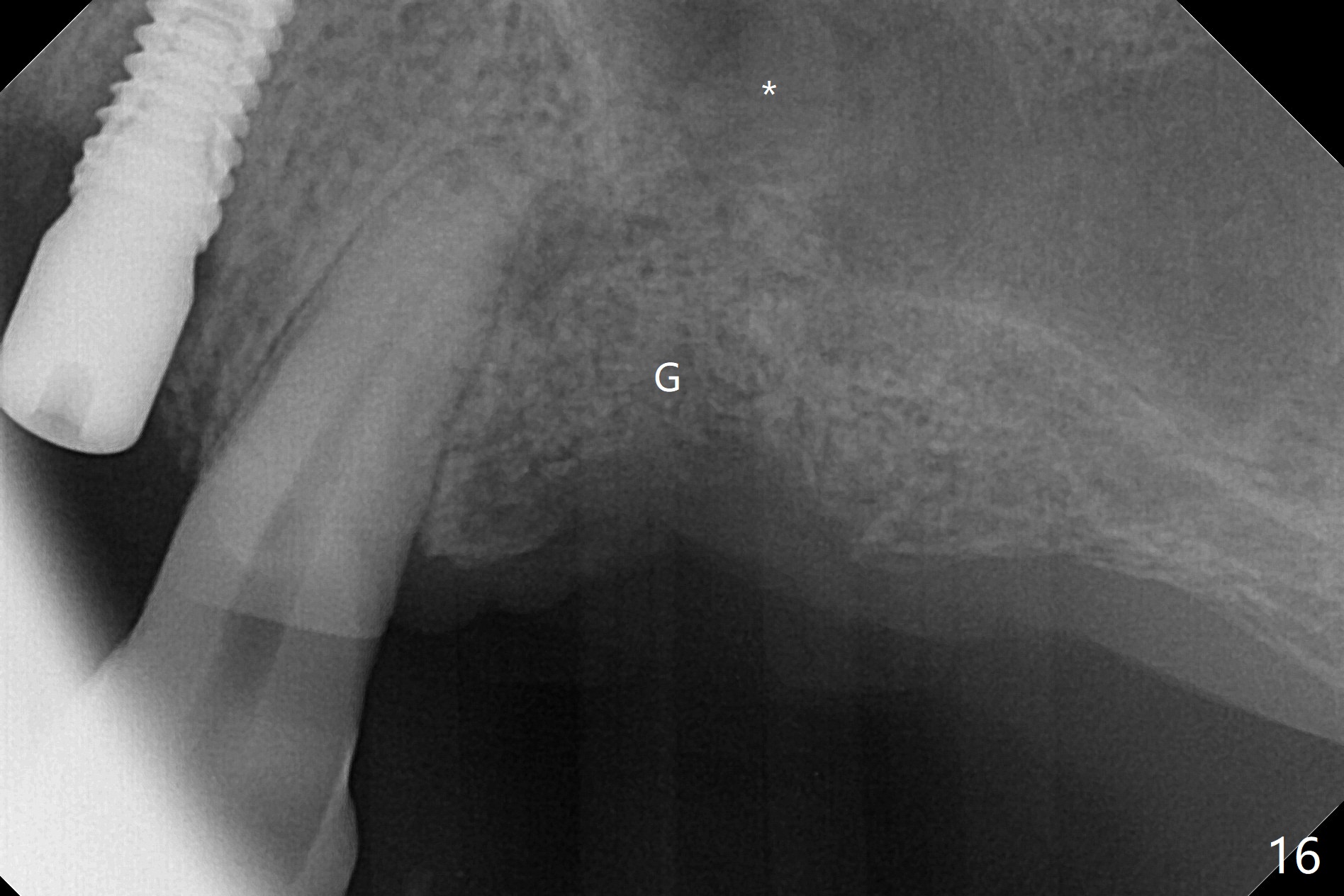
After a 4x10 mm implant is placed with fixture mounting (Fig.2 M) following sinus lift (*) at #12, osteotomy is initiated at #10 (Fig.1 (T: tube of surgical guide)). It appears that the drill (D) has good trajectory (between the Incisive Canal (red dashed line) and the canine root). The final position of the implant at #10 is acceptable (Fig.3). The implant at #12 is placed deeper (Fig.4 (arrow), as compared to Fig.2) because of clinically buccal superficial placement. The most critical challenge is anterior deep bite associated with posterior collapse. Periodontal dressing is applied. When the latter dislodges, there is minimal clearance for a provisional. Periodontal dressing is re-applied. The patient (smoker, partial edentulism with occlusal interference) returns for provisional nearly 1 month postop with chief complaint "something is lost in the back". In fact the healing abutment at #12 is lost with buccal granulation tissue (Fig.5). When a new abutment is seated, there is discomfort. When a healing screw is placed, it cannot be seated completely with two separate trials (Fig.6,7). Should we leave it as it is or open up for complete seating? It appears that the implant is loose. After preparation for clearance at #10, the abutment is retightened. It appears to turn with the underlying implant with discomfort. A 4x5 mm healing abutment is placed to reduce micro-movement. One week later, the infection at #12 dissolves with oral Amoxicillin (Fig.8). Due to limited occlusal clearance and implant tenderness when the abutment abutment is retightened, the cemented abutment is changed to a healing abutment. The implant at #10 seems to be osteointegrated, while the healing screw at #12 remains incomplete seating 3 months postop (Fig.9). The loose healing screw cannot be retightened securely, as there is bone loss around the implant 3 months postop (Fig.10 *). When a 4.5 mm x 15 degree 4 mm cuff angled abutment is placed, the mesiodistal trajectory improves (Fig.11), but there is no occlusal clearance (Fig.12). The latter would form when posterior support is established (Fig.13, either removable appliance (which the patient hates) or fixed one (finance)). Fig.14 shows the unhealed site of #12. Incision confirms the bone loss around the implant, which is removed. Although the sinus floor is absent, there is no membrane perforation. After debridement, allograft mixed with small amount of Osteogen is placed (Fig.15,16 G) and covered with Osteogen plug and 6-month membrane.
The bone density of the site is low 4 months post bone graft (Fig.17,18). Use the existing guide, but incision will be made. The osteotomy will be underprep. Take 5x5 cm CT for bone width and height after use of 2.2x7.3 drill with 1 or 2 O-rings. Prepare sinus lift, including water pump and bone graft, especially distal. Place healing screw and suture. Prepare PRFx2.
Return to Upper Incisor Full Mouth Immediate Implant, Trajectory
Xin Wei, DDS, PhD, MS 1st edition 06/14/2019, last revision 02/13/2020