
 |
 |
 |
 |
 |
 |
 |
 |
Implant Placement with Occlusion in Mind
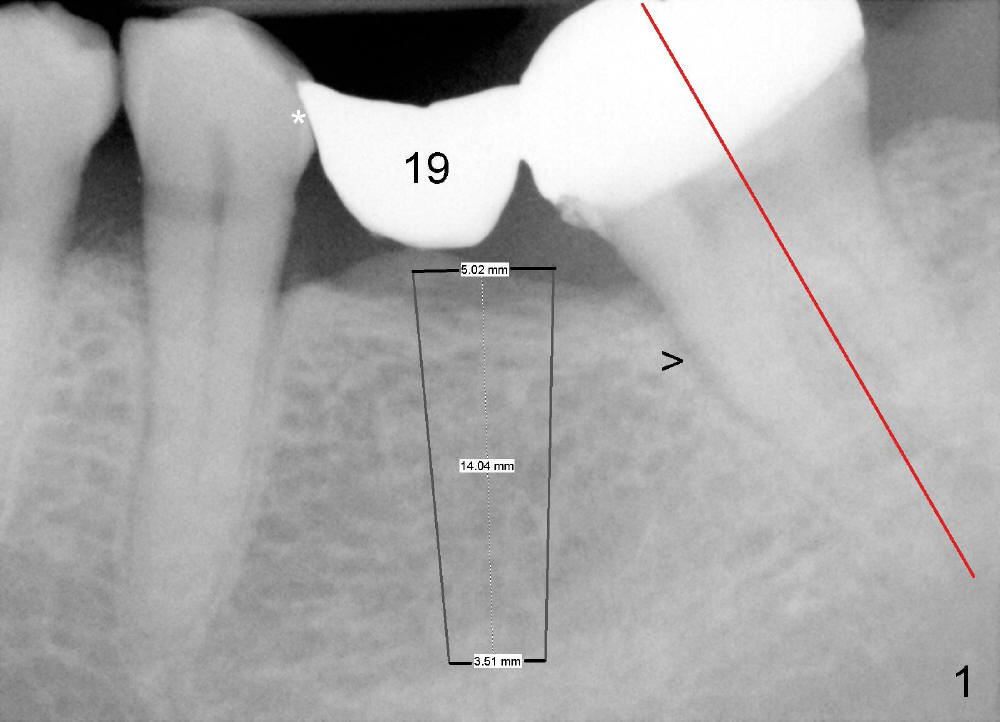
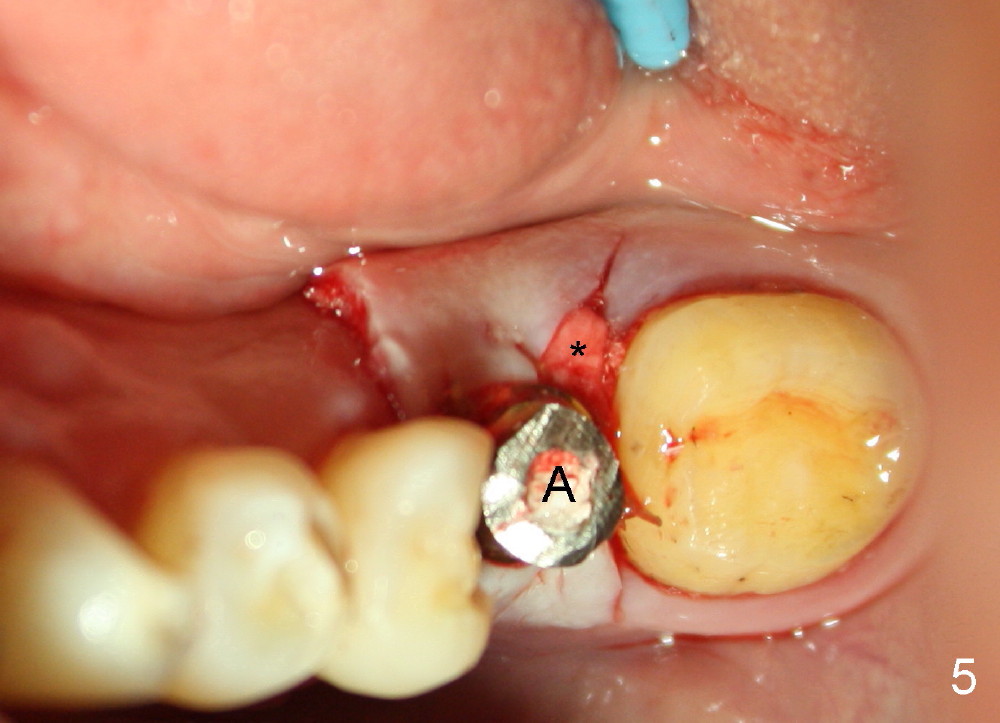
A 65-year-old man has a failing fixed prosthesis replacing the tooth #19 (Fig.1). The distal abutment tilts mesially (red line) with evidence of occlusal trauma (>). The implant at the site of #19 is intentionally placed distally (black outline) and will be used as an anchorage once osteointegrated to upright #18. Ultimately the mesiodistal width of #19 crown will be ideal.
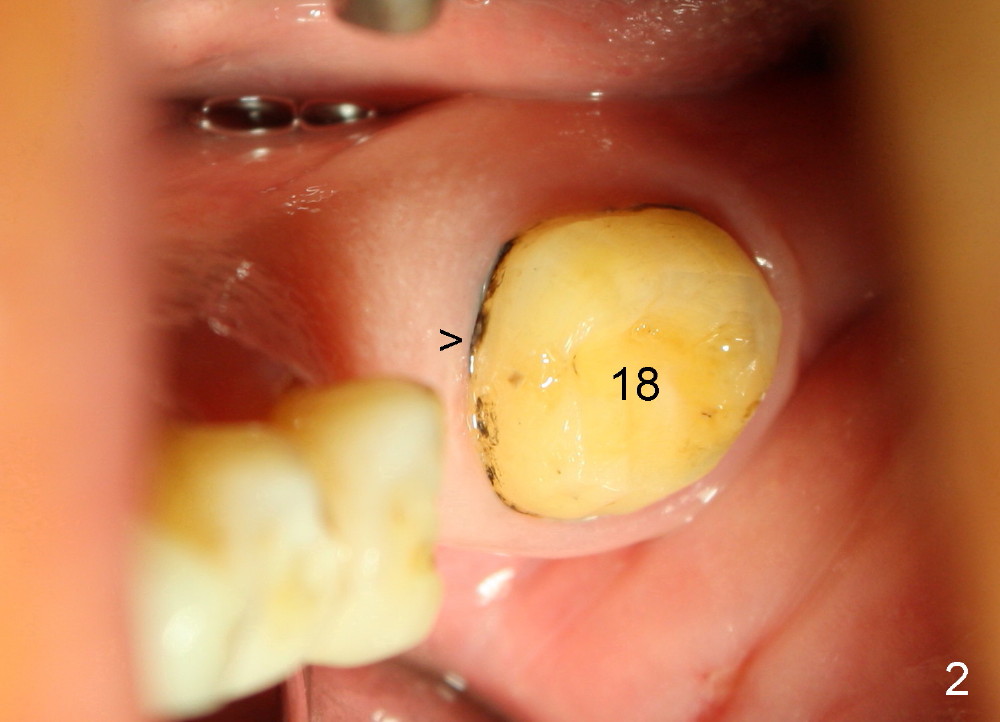
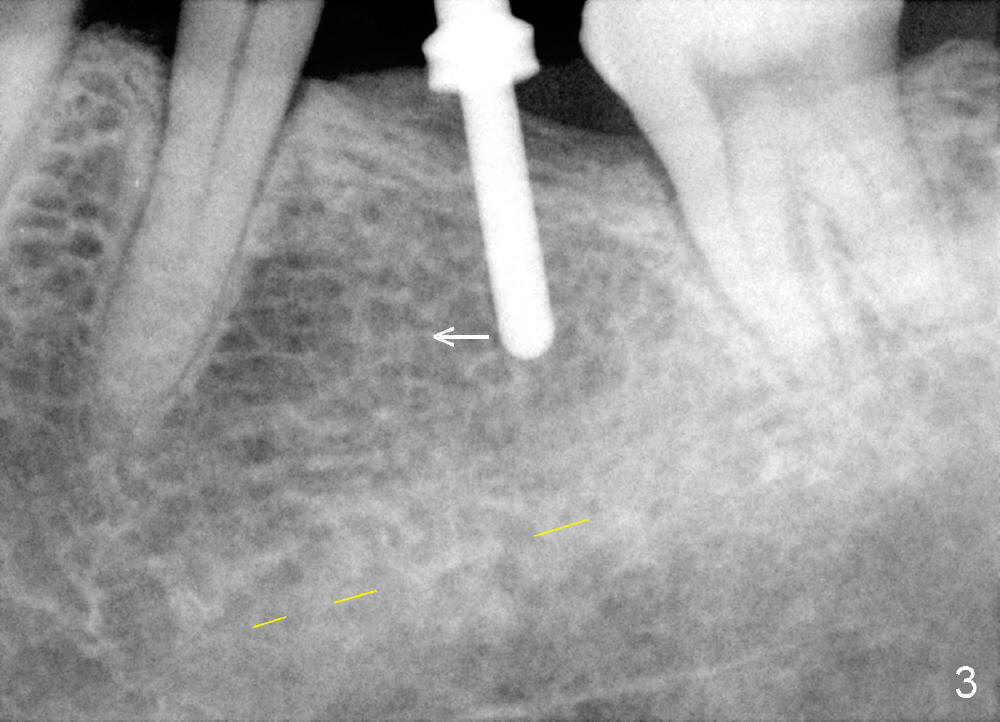
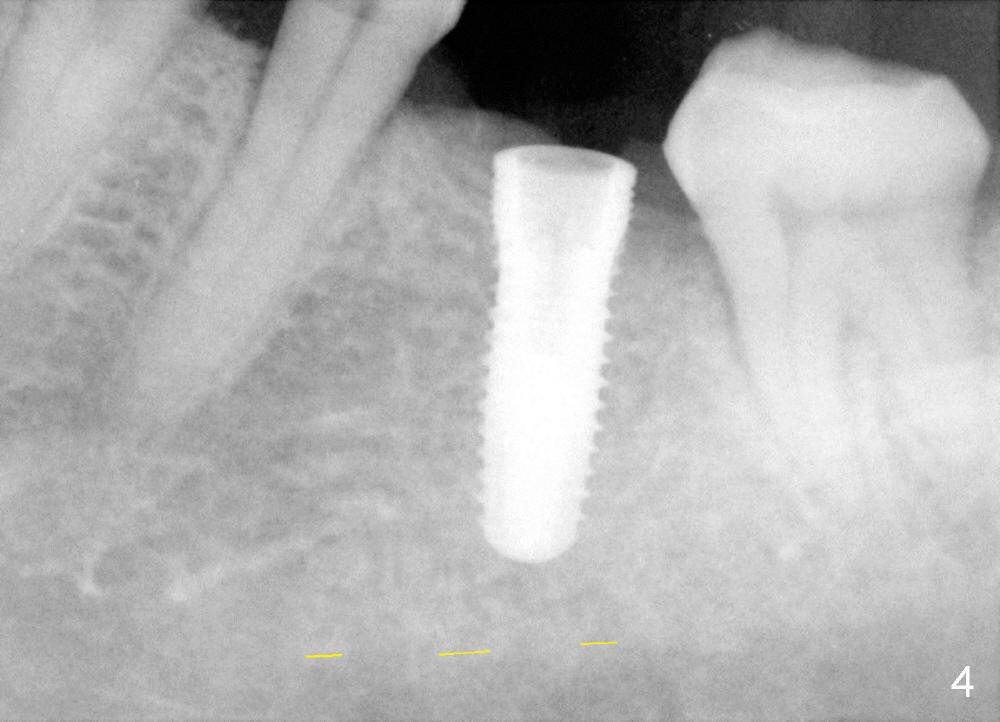
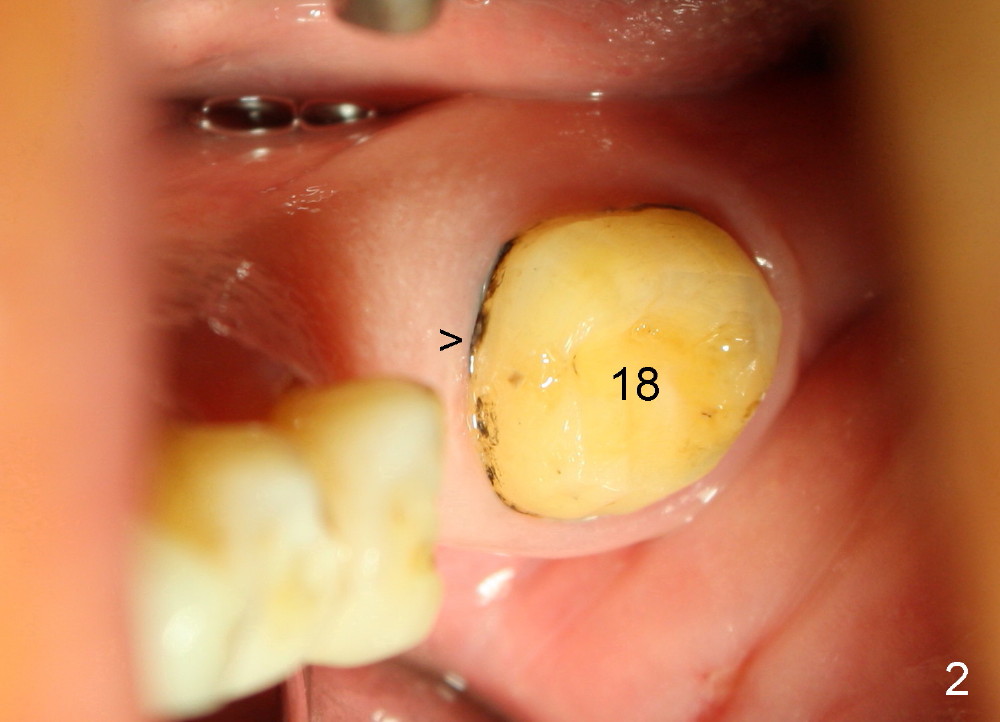
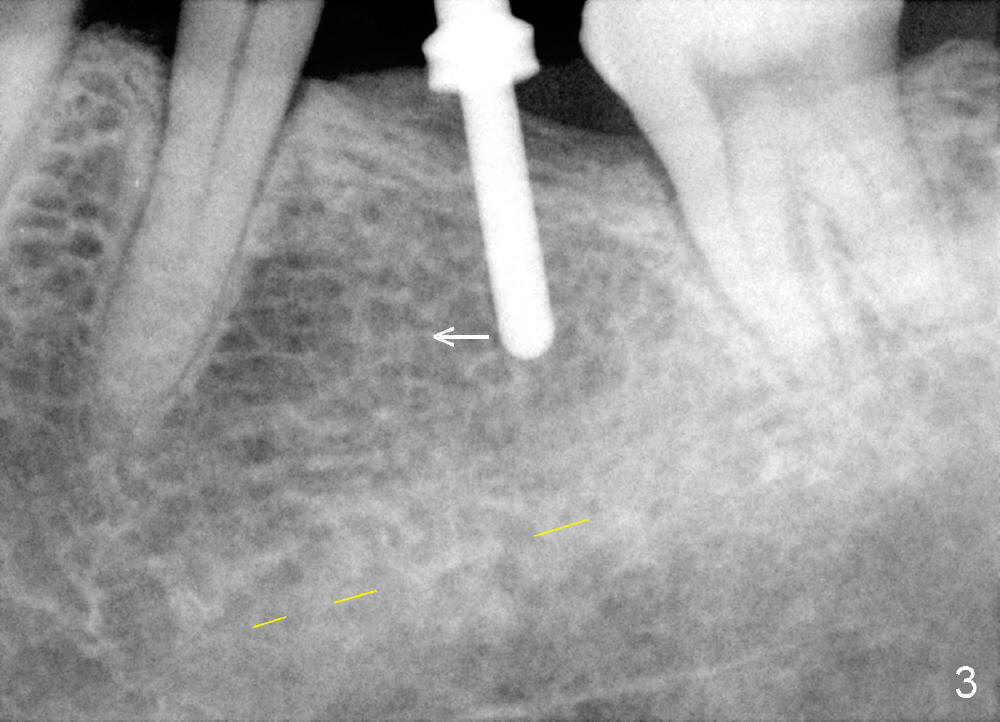
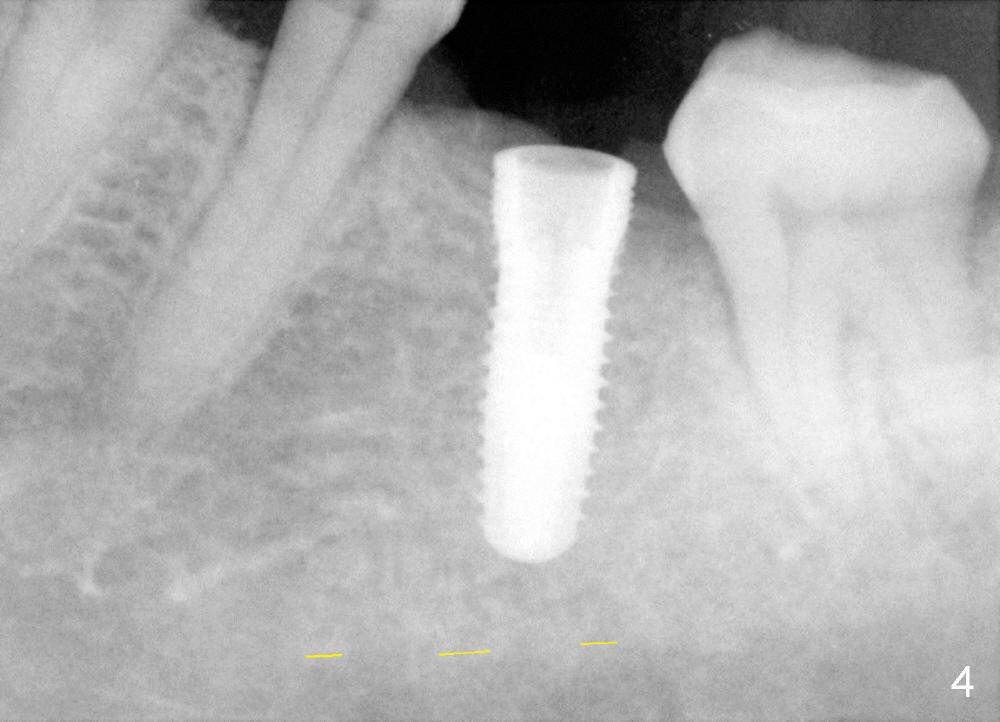
Fig.2 shows calculus in the mesial sulcus of #18 preop. After calculus removal, a 10 mm paralleling pin is inserted (Fig.3); it appears that the apical end should be moved mesially (arrow). Finally a 5x14 mm implant is placed as planned (Fig.4).
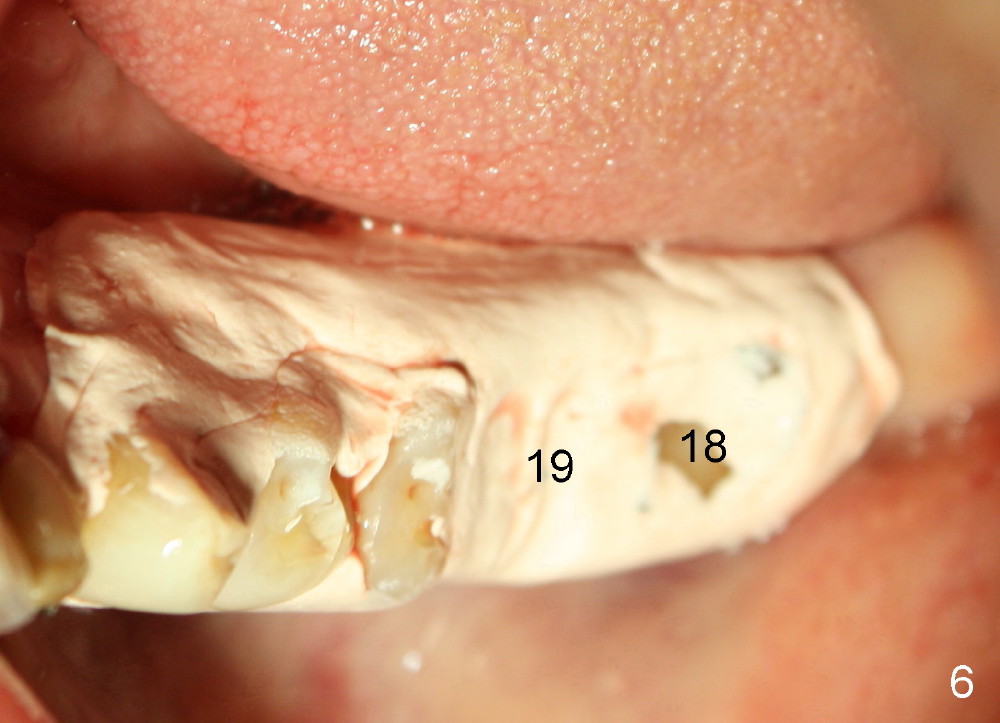
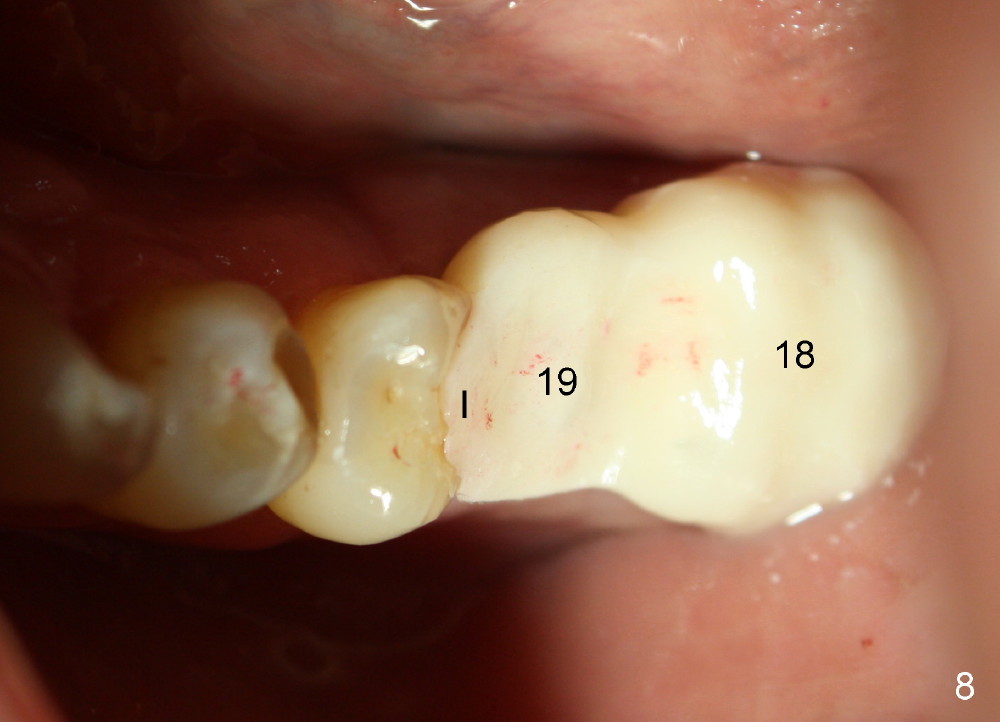
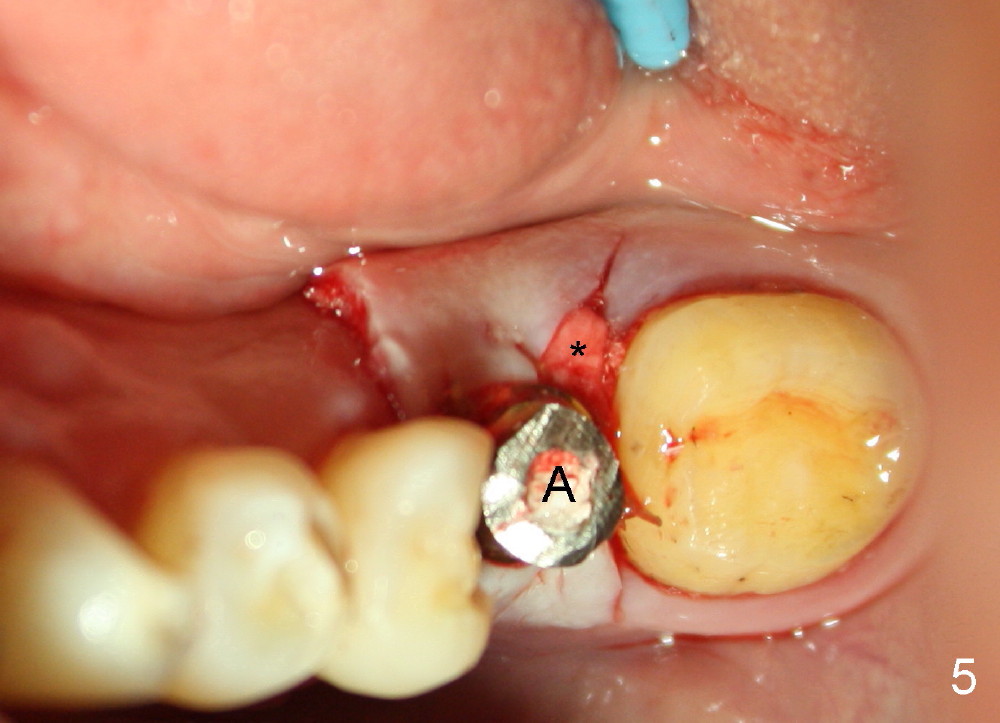
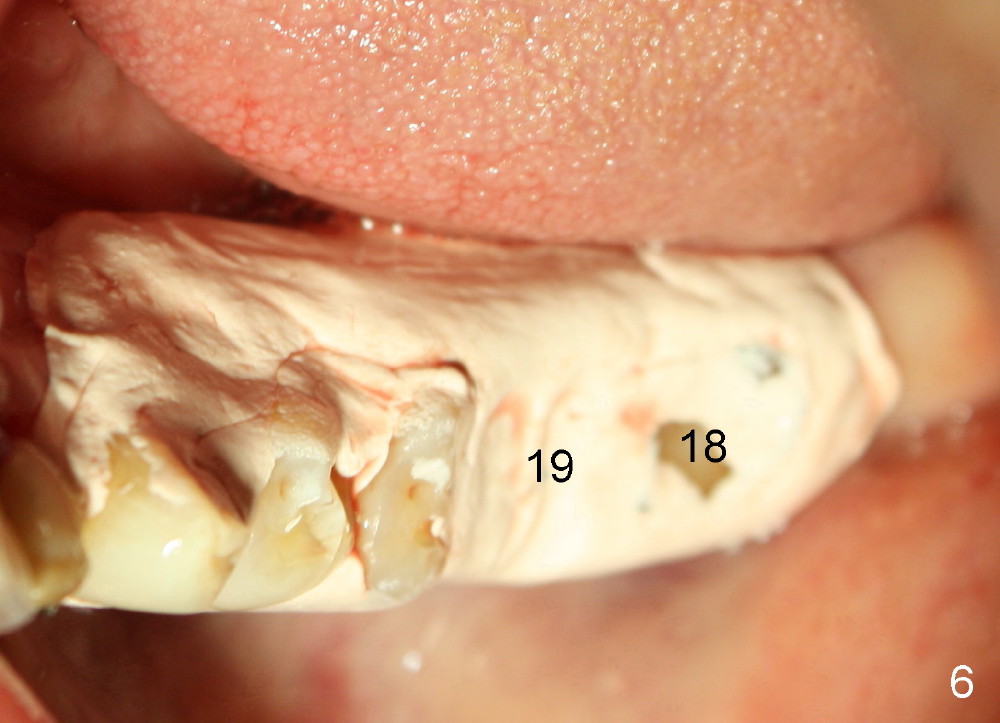
Buccolingually the implant and its straight abutment (5.8 mm, A in Fig.5) are within restorative limit. The most coronal threads of the implant are exposed lingually. Autogenous bone and Osteogen are placed over the threads, followed by collagen membrane (*). The wound is covered by perio dressing (Fig.6). When the wound heals 1-2 weeks postop, the implant will be used to load the provisional fixed prosthesis, which is also supported by #18 and 20 (distal inlay prep: Fig.1 *).
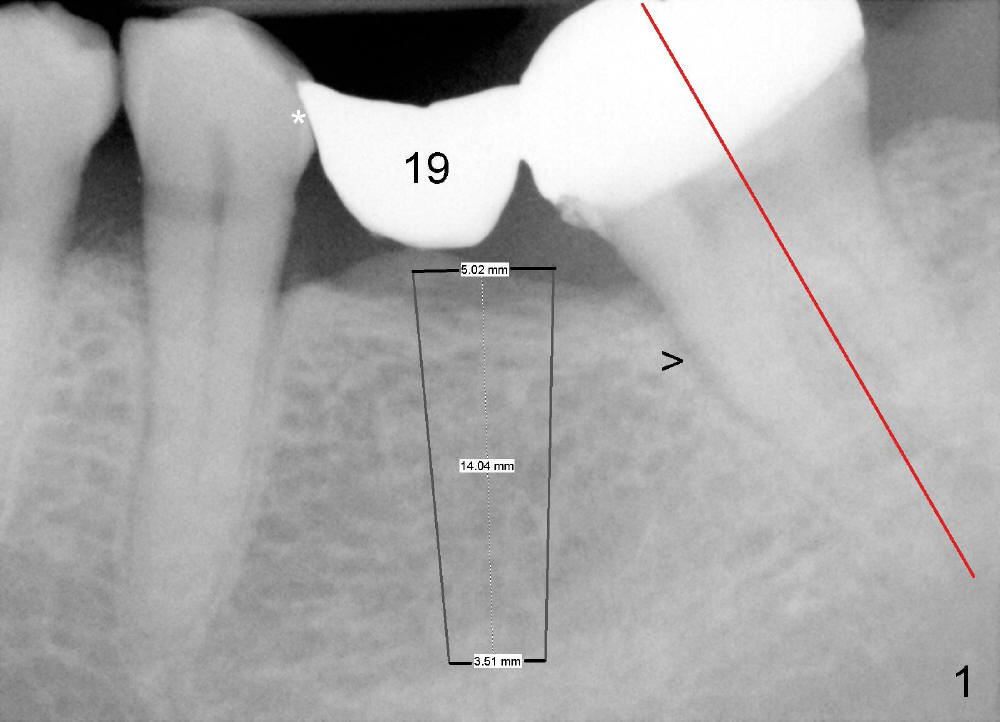
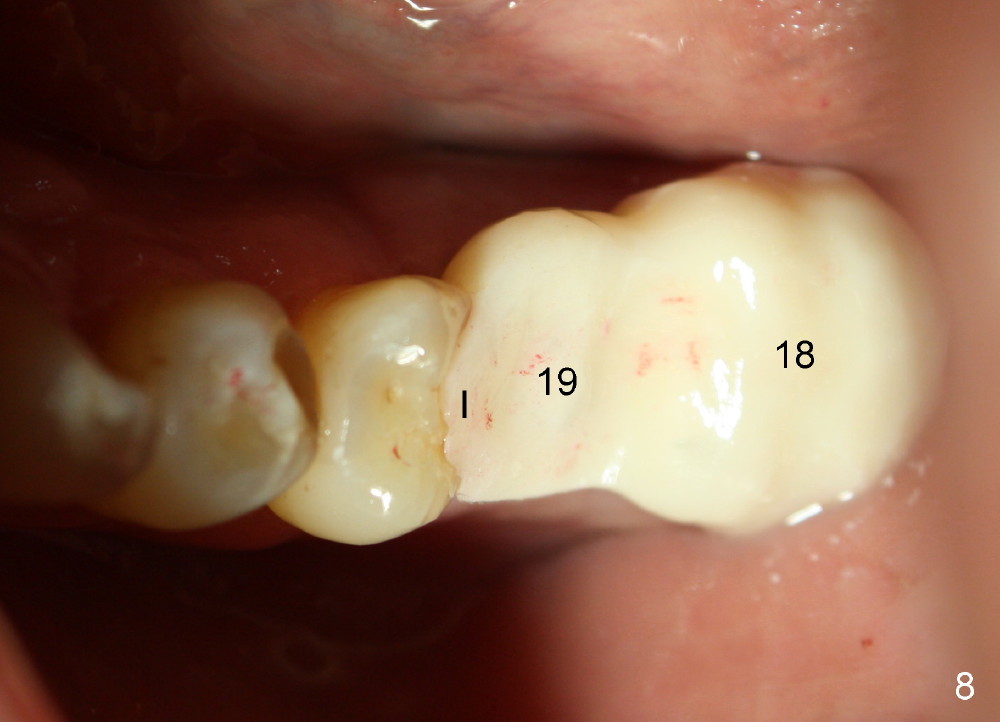
One week postop, the perio dressing stays in place (Fig.7). Then the patient is out of town. When he returns 3 weeks postop, the provisional bridge is fabricated as mentioned above (Fig.8). The provisional breaks down soon and are repaired multiple times, since there are multiple missing teeth. The patient is not eager to have ideal occlusion and wants restoration quick. We may try ortho in the upper right area.
Return to Implant & Ortho
Xin Wei, DDS, PhD, MS 1st edition 09/23/2014, last revision 03/01/2015