根尖炎复发原因
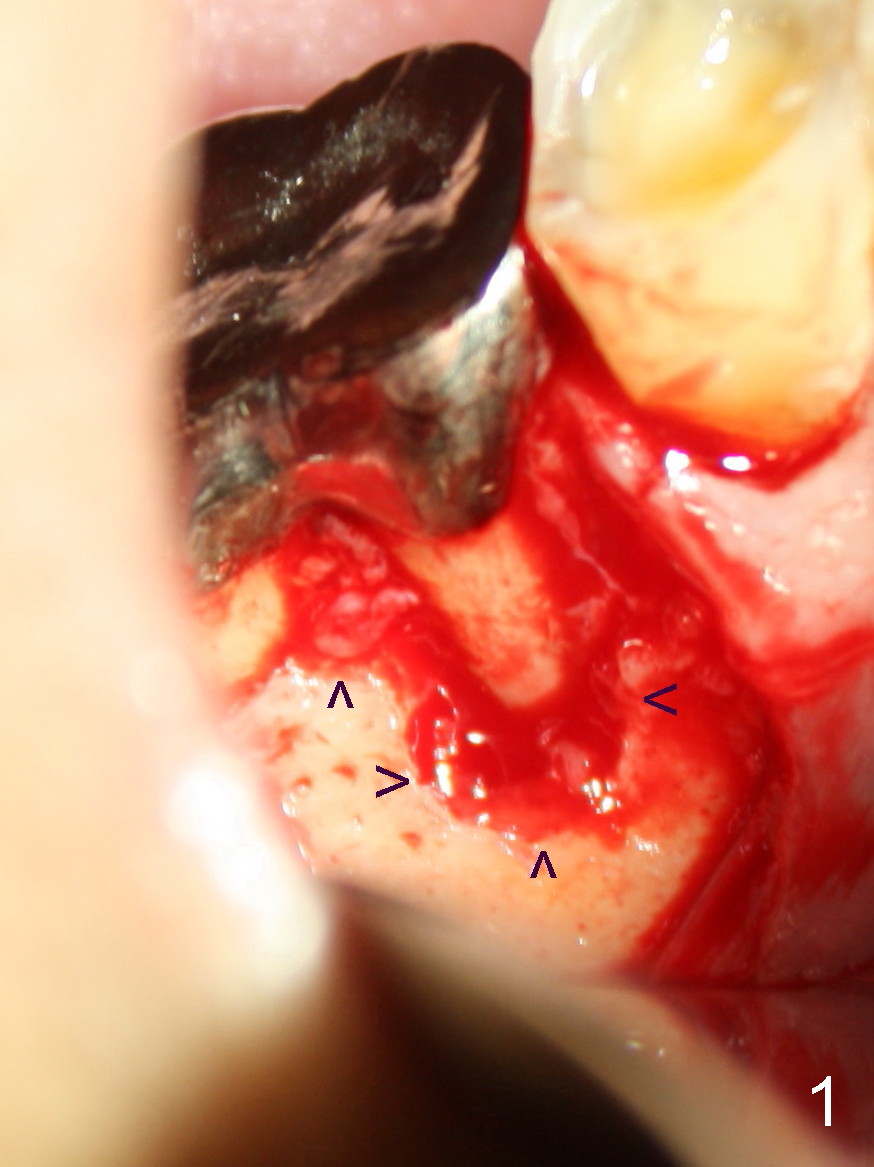
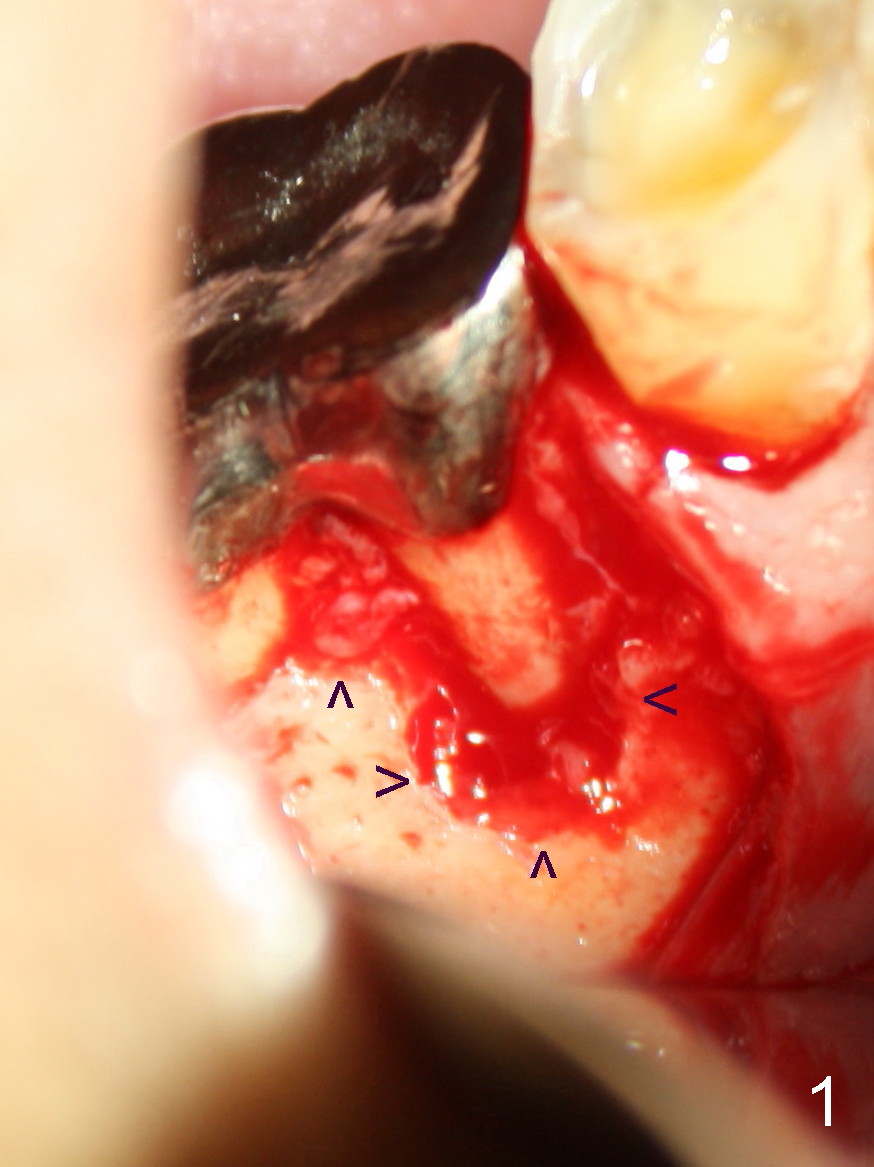
一般来说根切最难处在于翻瓣后寻找根尖病变,为什么这次不劳而获呢?整个近中根暴露在光天化日之下?当时思路不敏捷,眼光狭窄,为表面现象沾沾自喜(骨质变化(根尖周围以及根分叉(图一箭头)),忙于清除那里肉芽组织(包括之前除去根尖周围骨质),突然把注意力转移到近中根,发现本人意料不到情况(不过事先Dr.
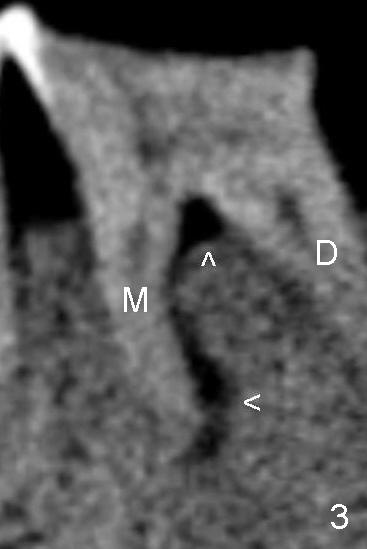
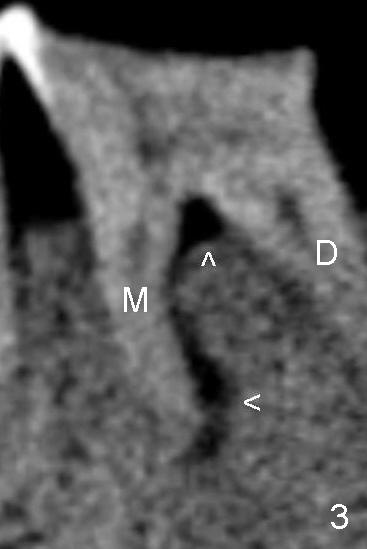
Peter Tian要求排除这个情况),使用双氧水冲洗伤口以及近中根,拍摄聚焦于近中根病变(图四),马上给病人看,向他解释这种病变可能是根管治疗原因(图三),而不是根管治疗所致,拼命摔掉背着黑锅,他回答却是“真的吗?”
更关键的是如何处理,小沐,金博一定要求拔牙,植牙,田大夫,方老师肯定推荐根切(hemisection or root
amputation),雕虫小技便是hemisection后即刻在近中牙槽窝植牙,方老师凉比不同意,但是缺损怎么大(包括iatrogenic,根尖切除造成,比较图一与图四),拔除牙根后,颊侧很可能凹陷,植骨太麻烦,不如一锅端(即刻植牙),冒一些伤口感染危险。
无论如何,病人不同意以上治疗,使用Clindamycin(溶解于生理盐水)后,关闭伤口。没有任何计划做倒充,如果根管治疗是自己做的,或者别人做的不错,才做根尖切除,估计除了根尖外充填完善,不必倒充。下颌第一磨牙根切已经够困难,倒充可能反而增加创伤,得不偿失。
今后对于不明原因根管治疗失败病例,应该做手术,切口大些,看得清楚,如果怀疑根裂,尤其是缺牙比较多,咬合力大的人,做根管治疗应慎重,象老田和方大哥所说,仔细检查,牙周袋深不深,切开探索可能是最明智的。几年前一位男士说他的根管治疗从来不成功,以为别人手艺臭,大胆给他一个牙桥基牙做根管治疗,疼痛始终不消失,最后CT和拔除发现根裂,做植牙告终。
Dear Dr.wei:
很高兴看到你的手术照片,说老实话,我很喜欢你的图文并茂的病例讨论,反复阅看,反复揣摩,可以让人得到新的启迪。
对你最后的处理,我有点困惑,我虽然常做根切,但一般都没有牙周病变,因为公司有Periodontist,
有牙周病变就先转给他们了。我的问题是,因颊侧骨板缺失,近中根颊侧完全暴露,如不植骨在表面,flap将来能不能长上,会不会将来形成牙周袋?当然根分叉处因也没植骨,也有这个问题。
我看了你以前的牙周-牙髓病例,好像你也不植骨,预后很好,看来在这方面你有独到的体会和见解,望赐教。
杭晴
Sunday, May 5,
2013 2:02 PM
Dear Dr. Jin: In fact, I am
trying to play a trick to test whether our readers are good at detecting
abormality from photos or from real patients or not. There is a vertical crack
involving the mesial root buccally (Fig.4, in which no label is used to indicate
the crack). At least the mesial root is hopeless, not to mention bone graft. The
most conservative treatment is hemisection or root amputation, but the patient
did not want to do anything right now. I plan to place implant at the site of
#31 while the infection at #30 is not so severe after apicoetomy. Once the
implant at #31 proves to work, I will persuade the patient to extract and
implant #30.
Our body has amazing ability to
regenerate once pathology is removed. I do not do bone graft unless there is
absolute necessity. I would rather concentrate upon removing pathological
lesions, by doing such as copious irrigation and soaking canals for a long
period of time for root canal therapy and thorough curettage of granulation
tissue at apicoectomy. It is consistent with yours, basically. Our body will
take care of itself. It will heal. Bone graft, if not handled properly, is a
foreign body and creates infection more likely than placing nothing. It is
personal experience, although I have to learn more about bone grafting.
05/05/2013
Dear Dr. 魏
读了你的Conclusion,
我感到十分担忧。这样的终结,你会高枕无忧吗?我曾三次请你探查上皮附着,治疗计划与决策要慎重,你应知道含义,主要是避免: efforts in
vain.你一定知道,或有这样的经验,在某一点上的探诊深度突然加深的含义。问题是在你手术中确诊为root
fracture以后,你还是决定做单纯的根尖切除,你觉得是否妥善?我和Dr.田,都给过你暗示。
我觉得你是个非常勤奋好学,襟怀坦白,能容纳不同意见的人,我很喜欢与你探讨问题。下面我谈谈发生在我的practice中cases.
我不下任何结论。我想你一定能读懂。
1. 病人是个白人女孩,2003年,当时她是个学校的substitute, PTE
(part-time employee), 很穷,#19因牙折而RCT, Post-core, PFM,
全套我只收了她$1250. 但对她而言是个天文数字。很不幸,两年后,#19 area,mild pain elicited only on
mastication, buccal red swollen mild,牙周探查,#19颊侧分叉近中頰根远中侧,上皮附着破坏,深达8mm,
并获取针头大小量的牙胶,#19 PA略显阴影,其他区域无明显骨吸收。我Dx: strip perforation, 并Flap
证实。然后我把治疗计划告诉病人:Ext. #19, bone graft, delayed implantation then
abutment-lava,并且告诉她,no charge at all, 她脸红了,反问我,“why? I will pay for it, Dr.
Fang!" 我想她这么说,实际上,是一种自身价值观,self esteem
以及文化观的体现。是一种公平文化的体现:有付出,就应有报酬!在她眼里,不让她付,就是:look down upon her. 她现在NYC
开业,在法学院毕业后。每六个月的recall, 都在我这儿。
2. 我也有非常bad experience. 四十来岁,男,广州人,保健品销售员。2005 年,#5因慢性根尖周炎而作RCT,
因工作忙,他不想在当日做 post and core.他答应一周后再回来作post-core and PFM, 所以我只用pellet w/
cresatin (note:现在此药已不受推荐)而后cavit-G 暂封。他一直没回来完成治疗,直到两年后某一天又回来了,据称#5唨嚼痛,PA显示#5
PAR明显缩小而且变淡,但还有, 我对比原来的PA,确任RCT无失误,也无根折,percussion 似乎(+)。根据职业i操守,我不能质疑病人的主诉。我向病人解释:冠部封闭,是根管治疗长期成功的重要因素,根管治疗后,最终的修复体,必须尽快安放,一般为三十天。#5
的possible reinfection是冠部封闭欠佳因缺乏最终修复体而致。他的third party 是Blue Cross,
RCT的frequency 是24 months, 有coverage。我可以给他retreatment,
但他不同意,他执意要在别的office继续治疗,并且要求把以前insurance payment for #5连同copay一起归还。我给了他几个option,
但他执意要钱,我毫不犹豫地写下支票full refund, 并要求他签下termination of relationship between the
patient and the doctor ( 这很关键!!) 他拿了钱,去做了眼皮手术而不去治疗#5.(这是她太太告诉我的,在他们divorce后)
想不到不出一个月,他要求回到我的office,
但被我果断地婉言拒绝。他迟疑地离去。他是我的同胞,我们来自同一块土地,他也受过不错的高等教育,新闻专业,我不想评价。
Thank you for your time.
Bingzhong Fang
Dear Dr. Fang:
I
accept your comment 100%. It is extremely difficult to force to do what we think
right for the patient (extraction, or root amputation). The tooth #30 is going
to fail. Is it ok to place implant at the site of #31 in two weeks when the
infection at #30 is most likely yet to recur? I hope that the implant at #31
works well. When the tooth #30 has problem in the near future, it is much easier
to persuade the patient to take it out and replace with implant. When
apicoectomy was done last Friday, the patient felt that pain at #30 was not so
bad. I am afraid that he did not think it necessary to do any further treatment.
I like the way you handle the two cases. May I post them so that somebody
else may get something out of them in the future? For the first case, RCT
was done in other office before the patient returned to see you? At that
time, she got a job with good salary? She must have thought that you are
better than the doctor who did RCT.
By the way, I did examine perio pockets before the treatment. Pockets were
surprisingly within normal limit. Probably I did not use certain degree of
force to do probing or angulation of the crown prevents the probe from going
into deep pockets. I mentioned the fact in the legend of one of photos. In
fact, I read all of your comments as well as others' before writing the
final chapter of the report. I feel that I followed your advice and others'
pretty well except dealing with the real patient. More importantly, I
appreciated very much indeed.
Xin
You may post both of them. At that time, she was still a substitute, PTE
and her Mom paid for the treatment. After that, her Mom also came to my
office as a patient with United Concordia ins. Now she became very rich.
I like you very much, Dr. Wei, not only your manner but also your
beautiful English.
Sincerely yours,
Bingzhong Fang
Dear Dr. Fang:
I read your message
(1st one) again. It appears to me that you are using Lava for crown in
implant cases. It is because of porcelain chip? Xin
I use zirconia lava because of strength and cosmetic.
Bingzhong Fang
你从我的两个cases可能已读出点东西了,尤其是第一个case. 实际上,我觉得,我没有任何可能造成strip perforation,
我是治疗她的#19的第三个医生。事发后,我从没有争辩,为什麽?
她来到我的office,带来了两张转诊单,并没有注明给谁,我也并无此要求。第一张是Chinese Doctor, 他仅做了access
chamber, 因为病人不停叫痛,他做不下去。据病人说:he couldn't num
b
me. 第二个是Caucasian Doctor, 病人受不了rubber dam,
她觉得透不过气来(我觉得这可能不是理由),医生不停地冲血,并三次让她咬住cotton, 她并且说: needle was so hot,
and hurt me. 我当时没有太在意,因为他是在Pasadena 颇有名气的,从信件上可以看出他已完成“shaping and
cleaning" and ready for "obturation ",
他没有提及出血和加热尖烫及软组织。说实话,我根本不太当一回事在当时。PA 与clinical exam后,consultation,
informed consent and fee discussion, then Tx started: sodium
hypochlorite irrigation并停留,WL, apical gauging, hand GT file
试合以发现锥度而无任何filing motion, 我并没有使用GG.或 任何 rotary files
,
obturation 技术:dual directional spiral tech. 而不用continuous
wave of condensation 因为病人对如上的医生叫苦连天“needle so hot".
我的操作中,没有一步会造成"strip perforation"。
有人也许会发问,为什么,不把事情搞搞清楚?有必要吗?病人非常安静并没有claim我,而且所有的charting, informed consent,
documentation 都是保护我自己而不是claim 别人。在做RCT的当时,我并没有任何质疑以及consult w/ the other
doctor who did tx.。
从这件事中,我觉得当时最合适的决定是:polite refusal, 不接受这个case.
从那以后,我有very strict policy: 1) 别人做过的RCT, 我原则上,不做crown, 要求病人go somewhere
else,但也有很多例外,有细则;但specialist不在这条细则内,因为我有太多的例证在手,最近就有一例。这不是我的傲慢或对他们技术与教育的否定,完全仅仅是出于对我自己的保护。This
may sound like fingernails on the chalkboard. If you feel this way, would
you please disregard it? 2) 别人placed implant, 我不做upper structure.
只有接受全套implant 服务的病人,我才接受。 3)Endodontic retreatment 的病人必须sign alternative tx
plan: possible extraction 以及将来可能的endodontic surgery, 于此,我向大家慎重推荐ADA
的informed consent, 连费用问题也想到了!善良和诚实而致的教训,是人性的呼唤,还是让我们变得更加worldly-wise?
敬颂
方炳忠
Dear Dr. Fang:
Thank you for taking time writing down your experience. I have read it
twice, because of my dyslexia. I have never doubted that you caused strip
perforation. Two things are the most important to a patient: no pain and make
him or her comfortable. Gentle initial injection and keep injection until being
numb, including intrapulpal injection. After placing rubber dam, check whether
the nostrils are blocked by dam or not. Cut part of the dam PRN. If you do these
two things right, the patient is most unlikely to suspect you. Dr. Fang, does it
sound that I am teaching you? In fact, I think that you have done these two
things wonderfully.
I
will not blame you even if it is your fault. I never suspect that any dentist
wants to cause complications. We learn from complications and try to make them
less likely to happen again. I love to figure out anatomical basis for
complication. More important is how to handle complications. If I feel guilty, I
will surrender openly, saying that your case is tough. It may be nosalvageable
in the first place. I am sorry that I was unable to figure it out initially. Can
we extract the tooth and place an implant? Can you pay the difference between
the two treatments? No teaching, either.
I like the way you protect yourself about informed consent. Because of my
结巴, can you help me in written format? Go to
www.xinweidds.com, Chinese version,
2. Adult, under Endo column, click RCT consent. Thanks.
Xin05/08/2013
魏心,小金:
由于各种原因,我不能再在网上与大家聊了,最后还想说几句话,就作为一种“Good-bye" 吧!下面几句话,“it may sound like
fingernails on the
chalkboard“,听起来或许有点不舒服,但确实是我想说的。同学与朋友之间的互相帮助,互相弥补,不存在“教不教我或你“的问题。 如果换一种角度考虑,我不懂的,你教我,这是化钱都买不到的好事而且又省时间,又走捷径。我将会很高兴的,真是何乐而不为。二位在大陆都有"OS"的background,
这点给你们的工作与学习带来了很大的方便,我和你们相比之下,相形见绌。我这个只具备"music" background“
而不成器的“musician",我样样都得从头学起,而且脱胎换骨,彻底换脑袋。我非常向往和怀恋以前美好的音乐生活,虽然没带给我财富,但我却拥有充实与激情。你们应知道这个世界是千变万化的,千万不要仅以background在工作中被假象所迷惑蒙蔽,事事朝一个方向想,某一种技术的应用取决于cases的需要,而不是千篇一律的。最重的是赶上时代的潮流,尽一切努力,学习最好的技术,理论与材料,
更新自己的知识。这点是再强调, 也不算过份的。于此仅举一例,二位所推崇的 Apicoectomy, (Endodontic
surgery中的一个步骤),你们已在大陆受过多年训炼,而我是来美后,在BU毕业后才学的,你们的经验一定比我丰富得多。在很多方面我学到的与你们习惯使用的不一定都一样,这一点我在Dr.魏的图片上已看到。我现在只拿你们的切口为例:1)Mandibular
Flap ( Triangular or Intrasulcular) 中的vertical incision
绝不是切在乳头上的,这点很重要;2)你们的vertical incision
的位置,从解剖的安全性,视野暴露以及将来的缝合这三方面考虑是最好的吗?从我的老师教我的以及目前的文献来看,我的回答是:NO! 3)当vertical
incision and horizontal intrasulcular incision 完成后,raise flap
时,到底从哪儿以什么方向开始,会最轻松而不弄碎flap?
这么简单而幼稚的问题,还需问吗?但在临床上看到的事实却相反。如果能在经常的交流中,根据自己的判断,学到对自己有用的,或者对错误作出识别,使自己更强大,所谓心理上感受到的“教不教我或你”的问题,
有这么重要吗?
顺致敬礼
方炳忠
方医生:谢谢来信!
我们同学之间交流,对大家都好。三十多年来我一直把您当作良师益友(更多老师)。上封信中,我害怕观点发表太多,伤害您自尊心,才说“no
teaching”,半开玩笑,但愿您没有真生气,千万不要由此不再发表意见。我从来没有因为口外背景而感到骄傲,当年没有好好学习,一心想出国,到了美国,又进不了口外专业。现在有问题,随便游览internet,从来没有静下心来学习。
至于切口,只要不违反血供原则,完全可以大刀阔斧,随便切,包括乳头,后牙不在话下,就是前牙我也不在乎,好像没有后遗症,不过前牙漂亮病例寥寥无几。切口关键要暴露好,上次暴露好,马大哈的我才能最终发现根裂,不过最后乳头切口有些难缝,下周病人回来,我力争拍照,露露丑(乳头伤口裂开?)。
方老师:还生气吗?要不要我打电话向您赔礼道歉?I am looking forward to hearing from you.
05/10/2013
魏心,小金:
我是年过六十的人了,遇事不会这么“小气“,这儿不存在“致歉“。我的确有很多其它原因,大块的文章,根本不会有时间了。冬生与Dr.
田,读过很多文献而且上过很好的seminar,可贵的是他们很具敏锐及悟性;海雄对implant dentistry
情有独衷,并且很有经验与体会。如果大家能经常与他们聊聊,一定会有很大的启发与帮助。
我提出的对于mandibular flap的切口(
Triangular or Intrasulcular)的三点看法,你完全误解了,这不是我个人的看法,你在当前的文献中都能找到。如果你在碰到不同观点的问题时,先根据别人给出的索引,思考一下,甚至再讯问一下,结论可以暂缓,可能帮助更大。我只给你谈两点,第三点,你一定找得到,花点时间想一想。
1.vertical incision 切不切在乳头上的问题,这不是life threatening issue, 你可以坚持你的所谓:flap
design不危及血供可以大刀阔斧地切。现在是什么年代了,我们当医生的,不但要让人活下来,而且要活得有质量,这是“life quality"issue.
这是个quality care 的问题。不切papilla的原则,在许多的文献中有警示的。另外告诉你一件事,“军中无戏言“, 在加州,Beverly
Hills, Bel Air, Santa Monica 等地方有一个"organization"称为"papilla police",
他们正在“抓“切papilla 的医生,对他们进行业务教育, 这是加州的几个Dental Schools 在lectures
中反复强调的。请你改掉这样的习惯吧!这儿也根本不存在前牙或后牙的excuse. 2. 这第二点,
应查一查文献,可能对二位的帮助更大。魏心,你误解我的意思了,这一点与第一点是不同的,不是指切不切papilla的问题, 而是更大的问题,不要掉以轻心!
还有同学之间的讨论,都是practitioners之间的商榷,大家的地位是同等的,不存在" who is superior to who"的问题,
更不要觉得会在"fair","even"上出现问题,因为一切都是自由的而且自愿的。
我不可能再有时间了,因各种原因,而且我妻子只容许我发不超过一行的短讯,从今往后。否则,她将强制性“剥夺“我继续使用internet.
最后,感谢魏心创立的这一文坛。Good-bye, 我的朋友们!
顺致敬礼
方炳忠
方老师:您好!
谢谢回信,虽然大家都没有时间,但是没有辩论,不动脑子,您我都会憋死,是吗?如果您太太真正爱护您,她会放行(let you do what you want
to)。发表一两句话也行。
至于切口,谢谢您提醒,我会收敛些,也不想太过分,与旁边牙医做不一样,免得失去执照。大刀阔斧后,有时要为自己收尾,最后我会吸取教训。不过如果说乳头切口不妥,牙龈最低点切口会容易造成牙龈退缩吗?
我们每个人时间有限,见病例一样不多,包括那些写书的权威,他们也不一定正确。如果上次根尖切除使用根尖小切口,我很可能发现不了根裂,可能真的要向病人赔礼道歉,免费植牙。
对不起再次打搅,再见!
You misunderstood me completely again and again. Would you please read two
of my short essays one more time? I have never done any semilunar flap in my
life because I hated it.. Come on, here nothing to mention anterior
Ochsenbein-Luebke flap or anything else. I just talked to you about the
mandibular flap (Triangular or Intrasulcular) two days ago and today, and my
incision was more aggressive (or larger) than yours, however I neither cut
papilla vertically, nor violated the parameter for the vertical incision
according to the standards of this kind of flap. You could find this
parameter or standards in many famous books, articles and good lectures. OR
simply disregard what I mentioned at all, and keep the way you prefer.
Sincerely yours,
Bingzhong Fang.
Dear Dr. Fang:
I
did not mean to upset you. I am willing to discuss something with you, because I
respect you. I will not discuss the incision anymore. Even though, I got
something again from your last (in fact this) message. Have a nice weekend.
Xin
My dear weixin:
If the purpose of your platform is to make a profit through a classmate's
discussion of your case please disregard the following. However, if the
purpose is for the patient's best interest please consider the following.
I have read the conversation between you and bingzhong fang regarding
mandibular flap. I may be wrong but it seems to me that you think a
successful flap is dependent on successful healing. However successful
gingival healing is not just dependent on primary closure but also restoring
initial soft tissue contour such as minimizing recession. To achieve this,
vertical release flaps should be avoided. If it is necessary, the gold
standard is to make the incision at the line angle of the tooth. You know
why? If you know, you don't need to read the following. With line angle
vertical incision it is easier to raise a flap for ease of suturing but most
importantly, it minimize osseous defects and thus subsequent recession,
dehiscence or fenestration, creating dark triangle. Cutting at the papillae
is the most unfavourable release. Also by cutting at the base of the scallop
you are incising on radicular bone, prone to osseous defects. Dark triangles
between teeth, below contacts, in anterior zone is very unaesthetic. They
also cause food impaction in posterior dentition.
Today recreating papillae is still the biggest challenge for dentists. Thus,
I don't understand why you are making incisions at papillae. As a good
dentist we try to minimize iatrogenic damage and feel proud about our work.
You will probably stick to your ways but I encourage you to consider this
matter to improve your professionalism and standard of care for best of
interest of everyone.
One thing I don't understand is your lack of knowledge or wanting to speed
up to increase production. Just be careful if you have demanding
knowledgeable patients who may seek second opinions. I always ask myself did
I do it or did I do it well.
Good luck. This is purely an academic discussion, please don't take it
personally. Thanks.
Sincerely,
Dongsheng Wang
Dear Dr. Wang:
Thank you very much for sending the message. I am not upset whatever. Instead I
am so excited. It was told that you are as crazy about dentistry as anybody else
in our class. Now you have finally shown it. What is more is that your written
English is so wonderful. With that we should not have problems understanding
each other.
First of all, I have never mentioned or recommended vertical
incision made in the papilla. Instead an oblique incision was made at the line
angle (thanks for your mentioning. I did forget the terminology) as shown by #4
photo in the topic #3 (复发性根尖炎
3, incisions
for apicoectomy). Would you please go to
www.xinweidds.com, Professionals, Classmate, Endo column
to check it? If the incision was not made more or less at the line angle
of #29, please let us your version by showing drawing or photo. The worst part
of me is to play trick on my classmates. Occasionally, I do not make clear on
writing or labeling on photos. The purpose is to test whether readers are
careful or not. It simulates clinical situation. The patient or complicated case
will never tell you what is wrong. It all depends upon our ability to make the
best judgement by seeing and thinking clearly. Or I just do not have enough time
or think it necessary to make it clear when I write.
Secondly, 大刀阔斧随便切 is just exaggeration. Within realm of standard care, I
might make a little deviation. When it is attempted, I am aware that I need
to fix it when complication happens. It is certainly not
my intention to hurt the patient. Anyway, I have to stop here.
回牙科学术讨论园地
Xin Wei, DDS, PhD, MS 1st edition 05/03/2013, last revision
05/11/2013