







 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Cosmetic Issue of Anterior Periimplantitis Surgery
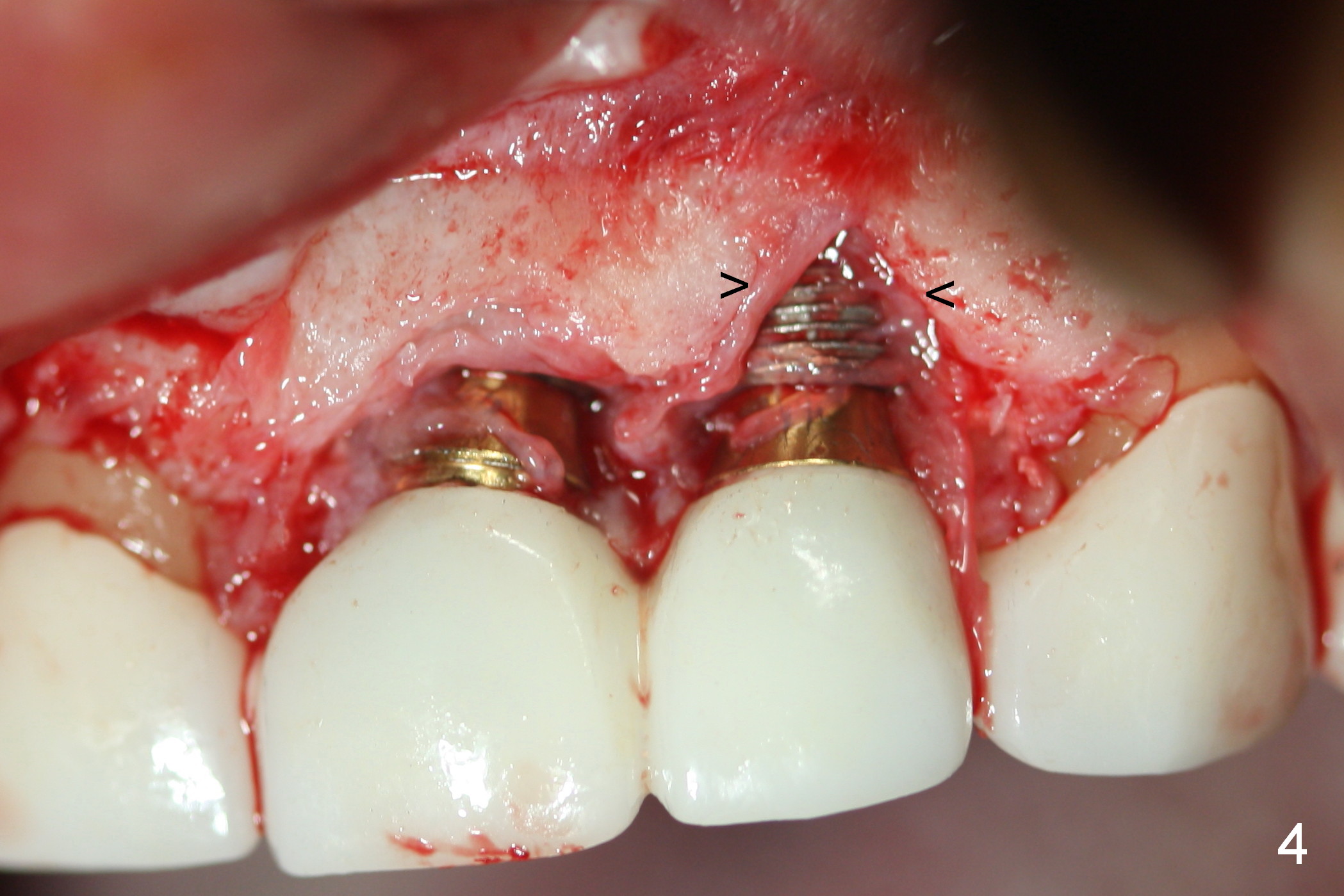
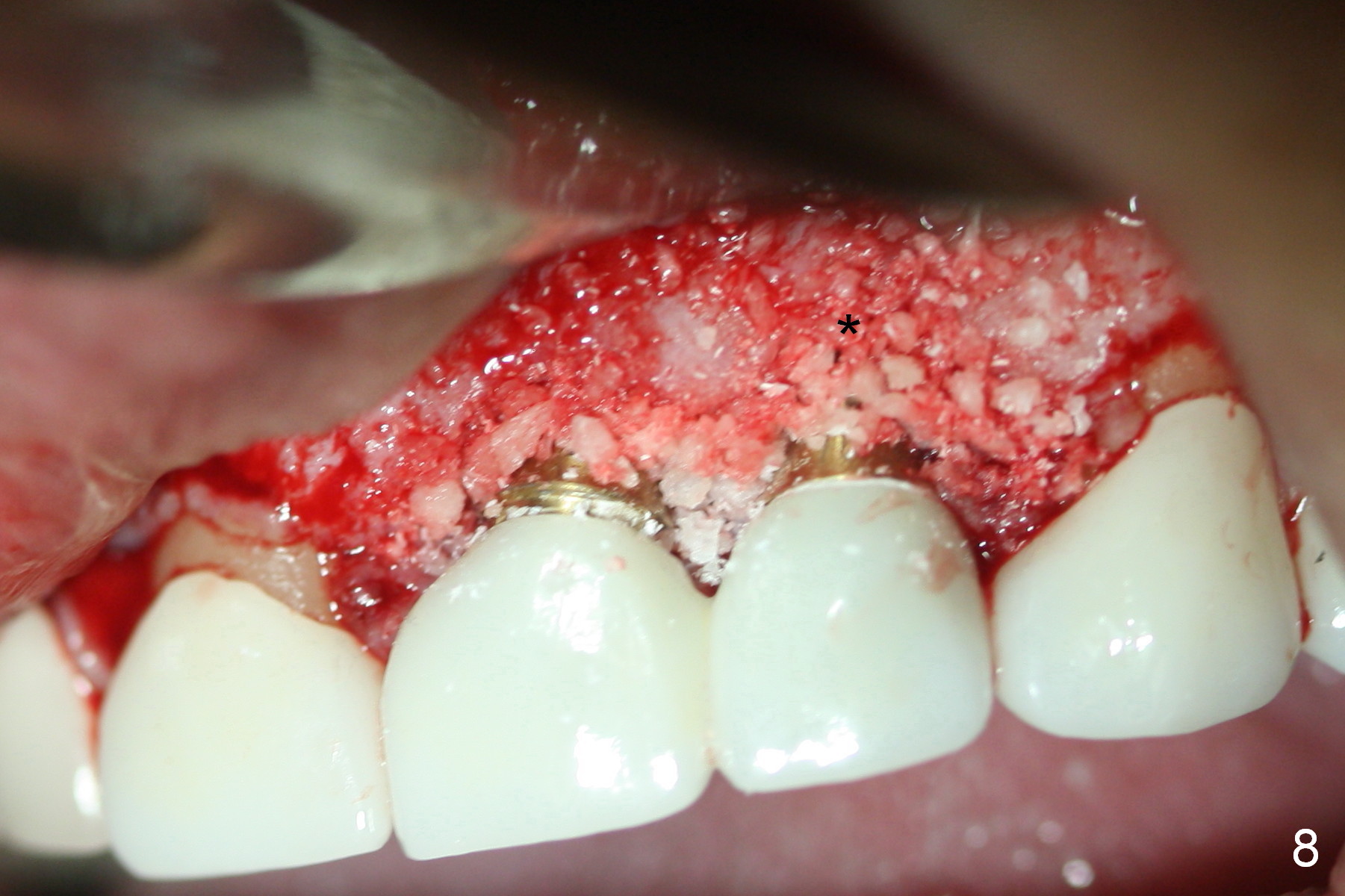
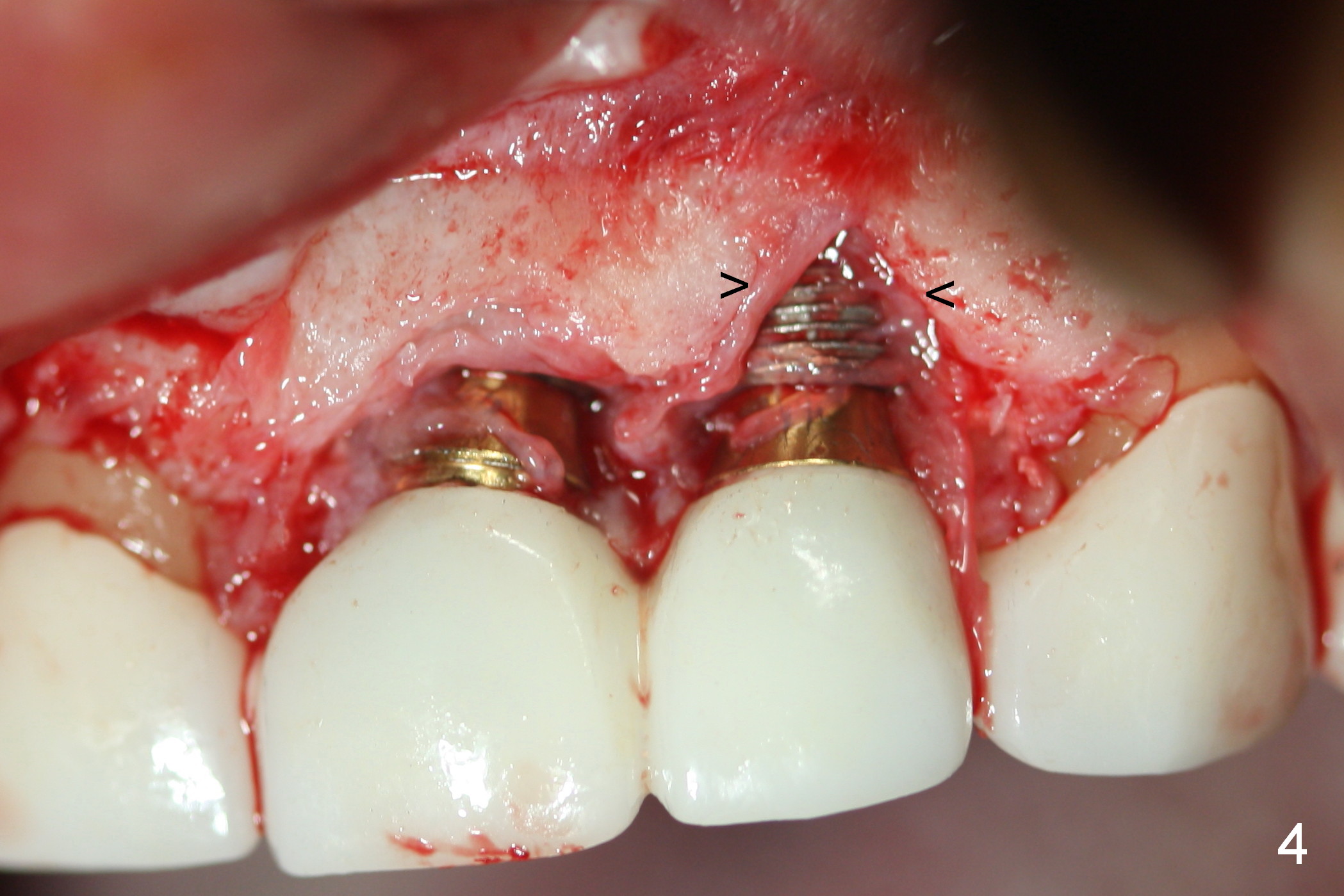
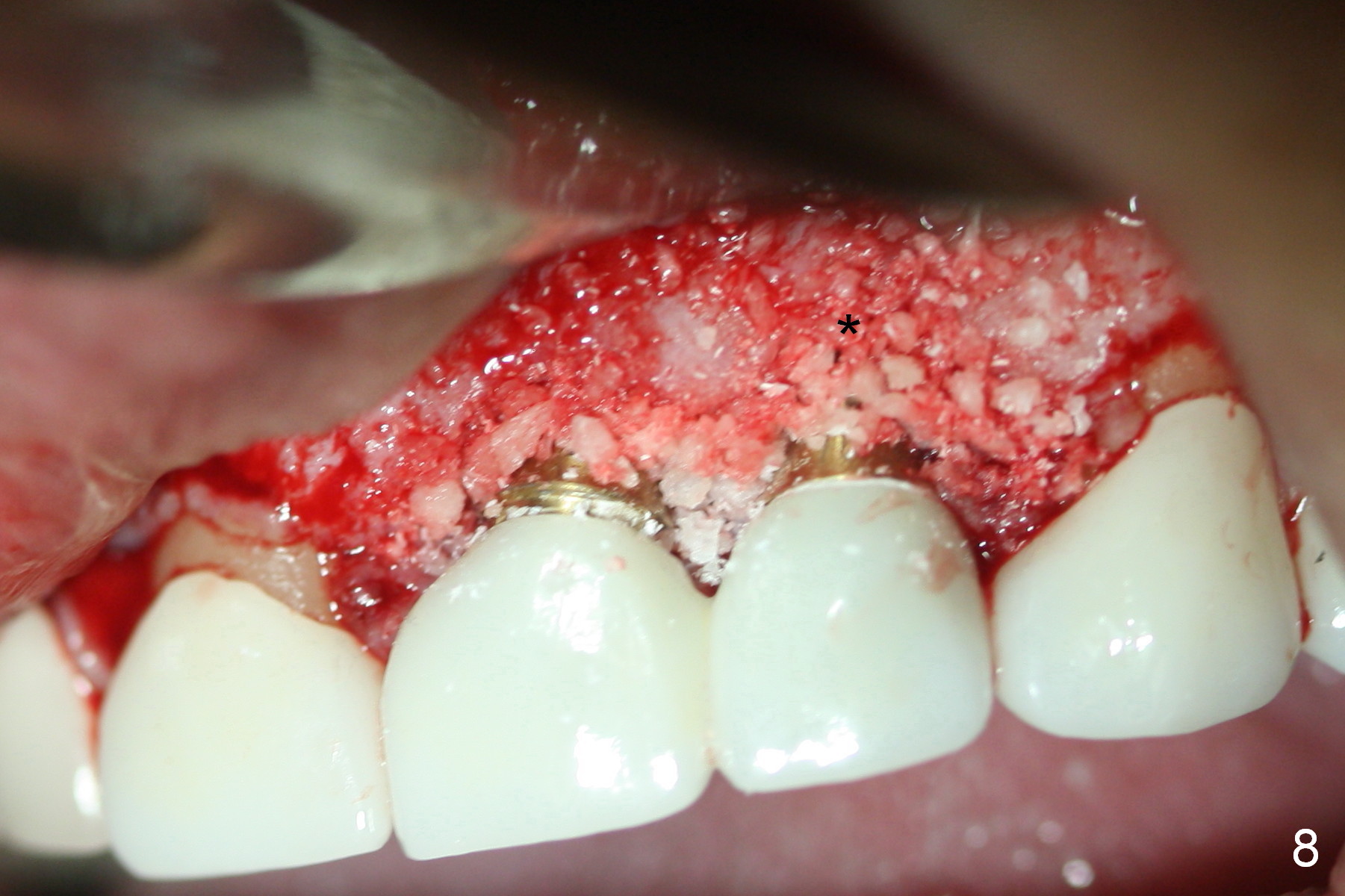
Periimplantitis develops in the anterior region 6 months postop (Fig.1,2). Predisposing factors include smoking, seniority, multiple missing teeth and bruxism. Flap elevation reveals granulation tissue (Fig.3 *) and bony defect at #10 (Fig.4 arrowheads). After granulation tissue removal (without Titanium brush) and copious irrigation, the affected sites are soaked with Metronidazole gauze (Fig.5 *). The exposed implant threads look clean (Fig.6). Exposure is more likely due to coronal placement (Fig.6) than buccal one, since there is buccal space (Fig.7 *). In spite of the best effort of curettage, there appears to be residual infected tissue (Fig.7 ^). Bone graft (cortical and cancellous) is placed in the defect area (Fig.8 *).
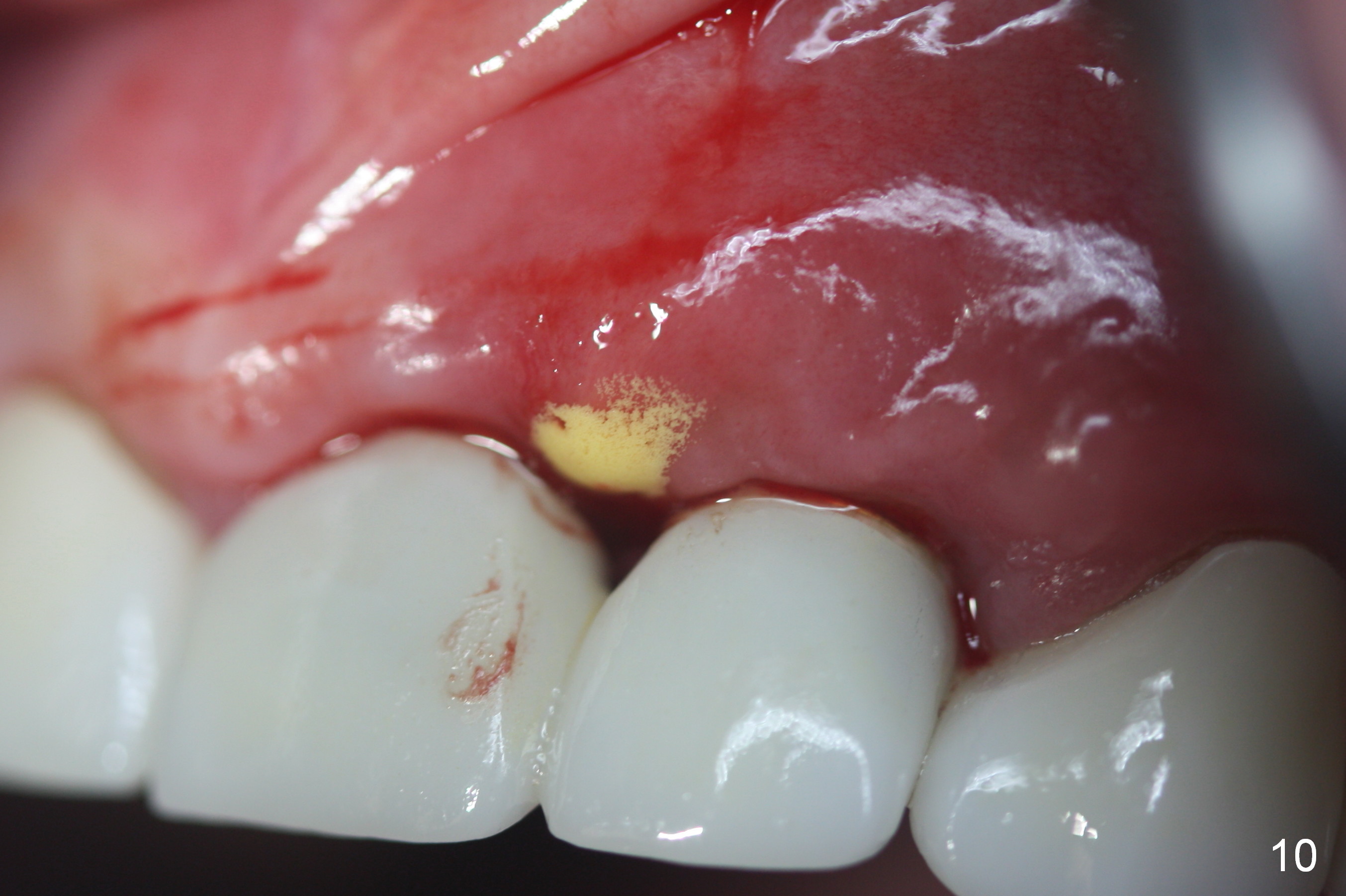
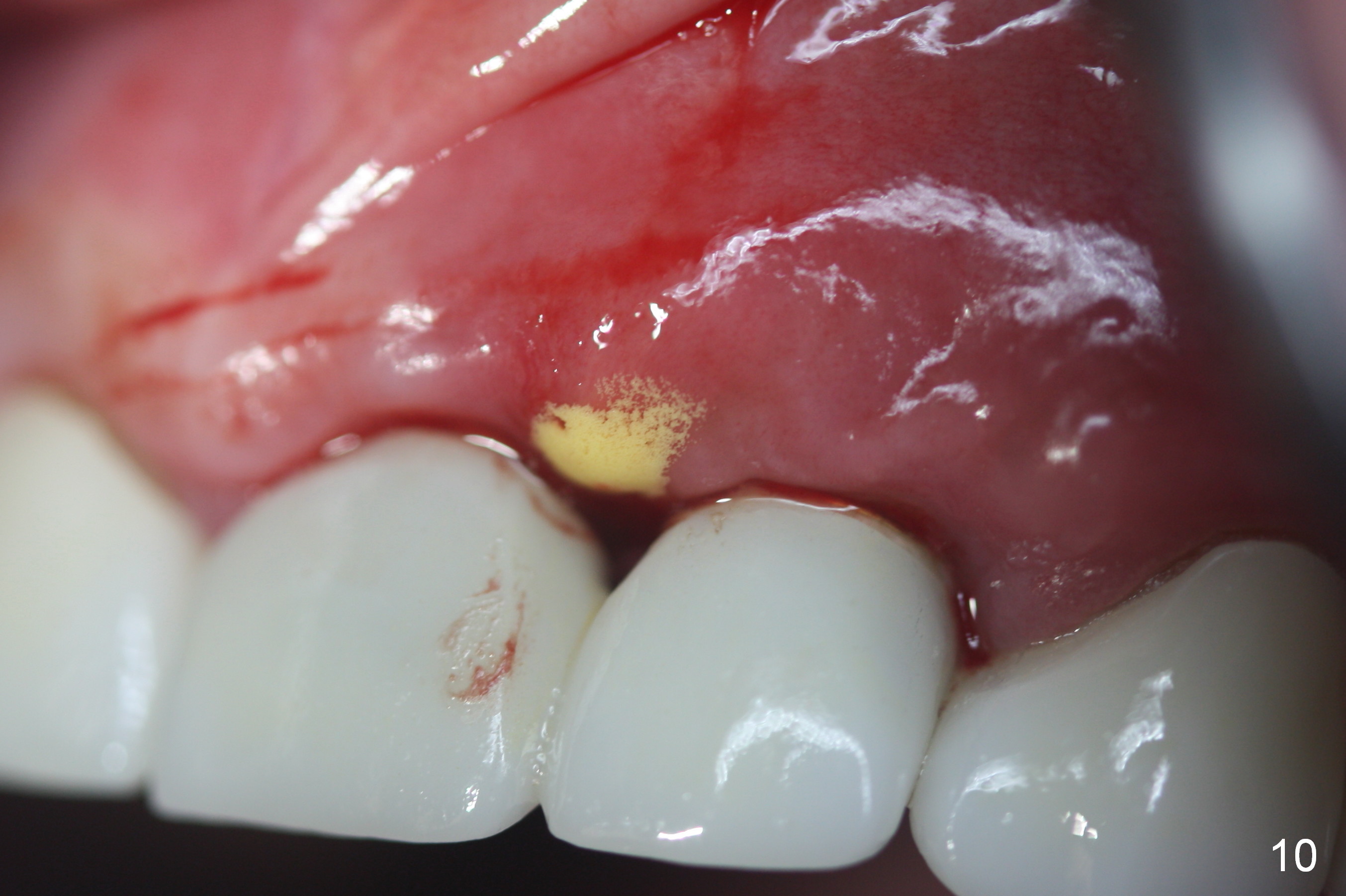
There appears more pain associated with the debridement surgery than implant placement. More critical is papillary recession (Fig.9 >) with residual infection (*) 3 months post debridement. Sharp instrument is used to break the mucosa for gentle curettage, Chlorhexidine irrigation and Arestin placement (Fig.10 yellow). Fig.11 shows mild erythema (*) between these implants with light tenderness. The patient is reluctant to receive further treatment because of potential cosmetic compromise. Non-incisional approach seems to be necessary. Finally the implant at #10 is loose.
Return to Upper Incisor Immediate Implant,
Periimplantitis
Xin Wei, DDS, PhD, MS 1st edition 02/22/2016, last revision 01/19/2018