

 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
Small Implant for Long-termed Residual Root
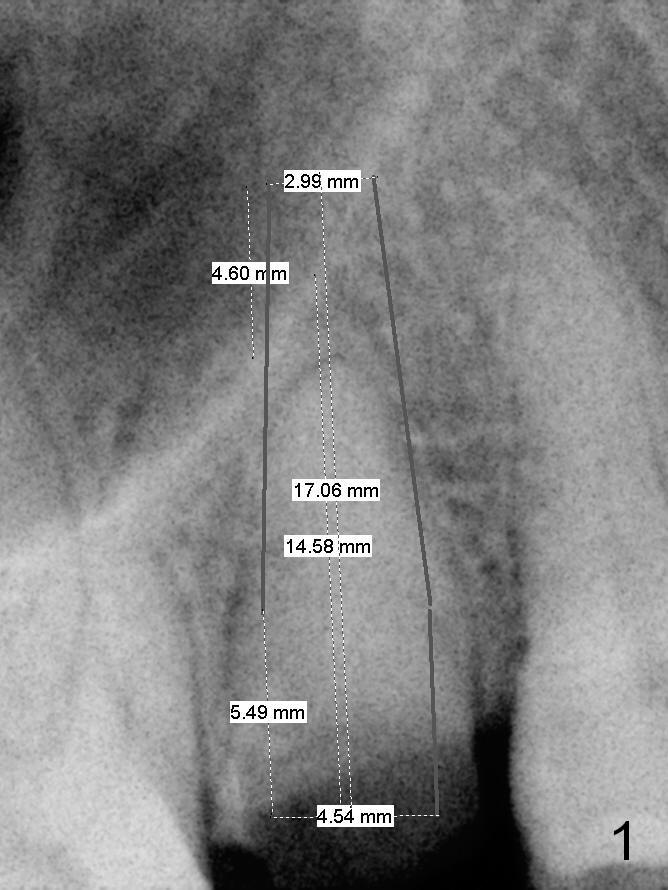
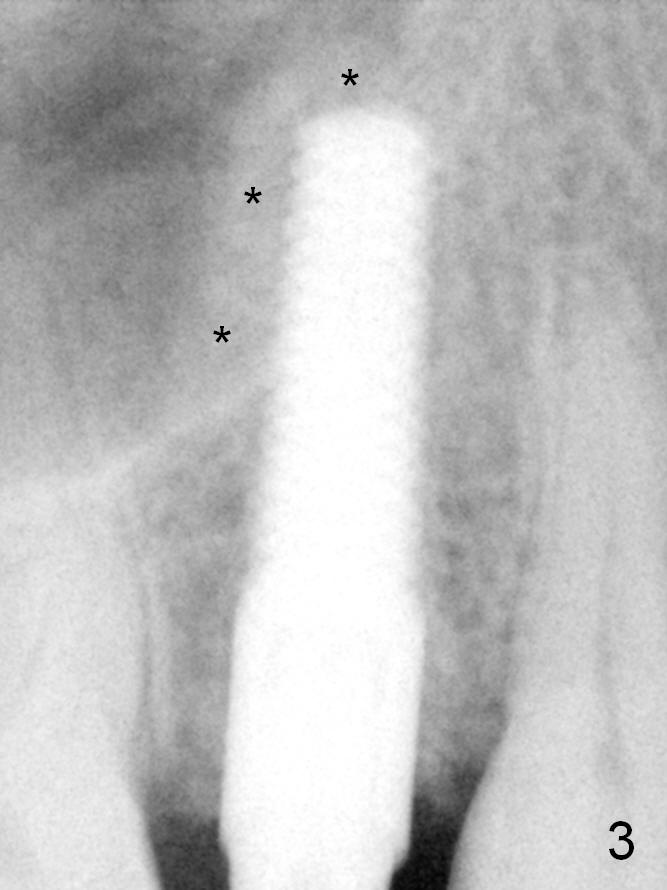
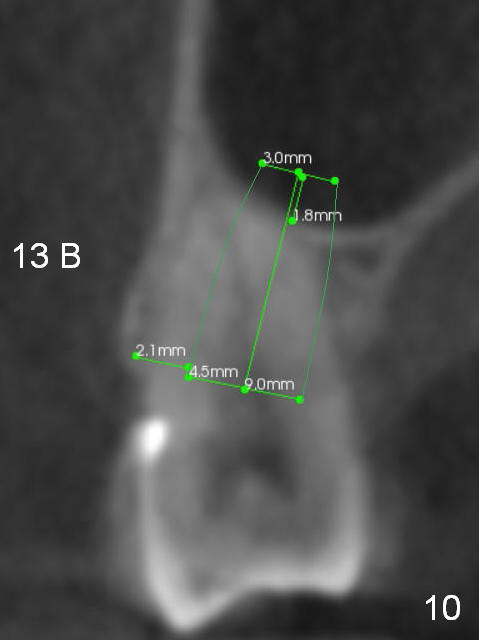
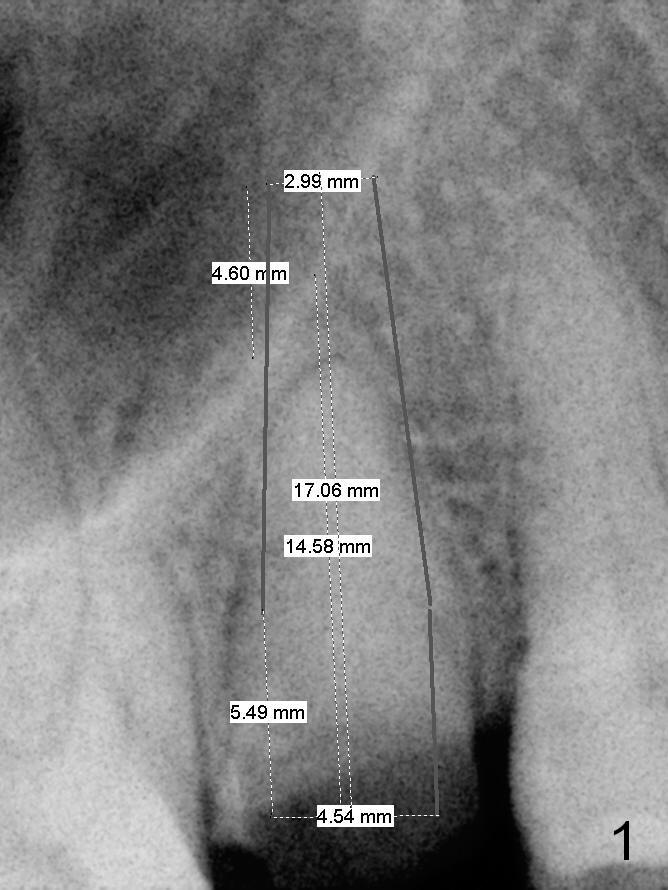
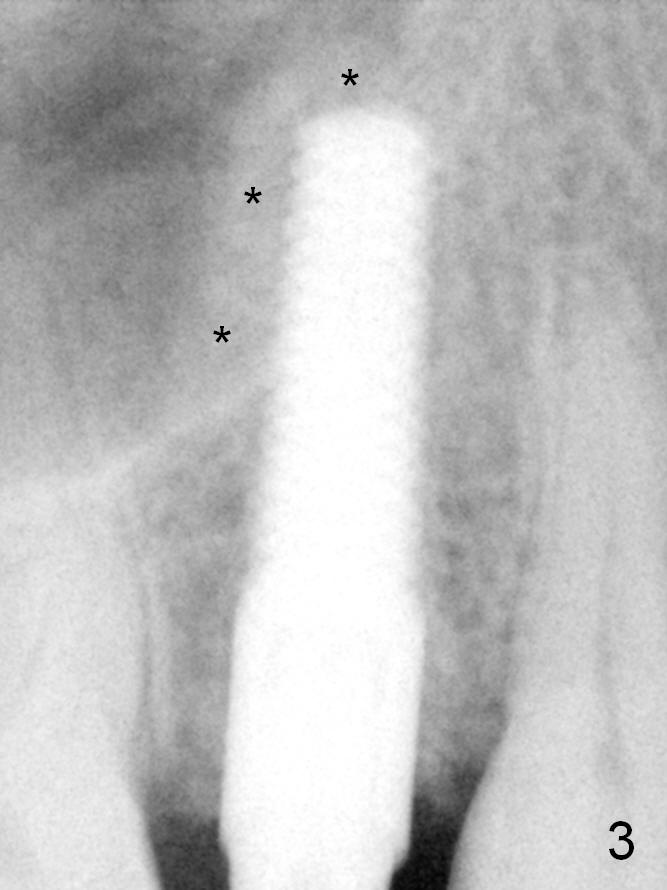
Preop design for the residual root at #4 is a 4.5x17 mm gingiva-level implant (Fig.1). After using 3 mm reamer (Fig.2), the handle of a 4.5x20 mm tapered tap cannot go through between the neighboring crowns (5.85 mm). A smaller implant is placed (Fig.3: 4x17 mm) with primary stability; note sinus lift (*) with allograft and Osteogen.
Preop PA should include not only the roots of the neighboring teeth, but also the crowns. Without the former information (especially root curvature), an implant may pinch the root of a neighboring tooth. Without the latter information, it may be difficult to insert an implant through the narrow coronal space due to long-termed non-functionality such as this case (Fig.1).
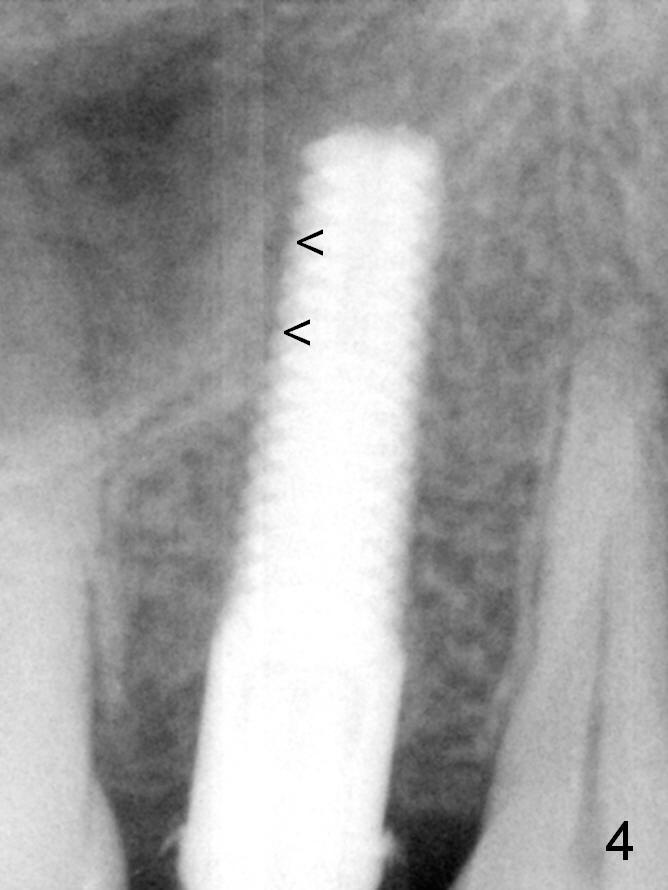
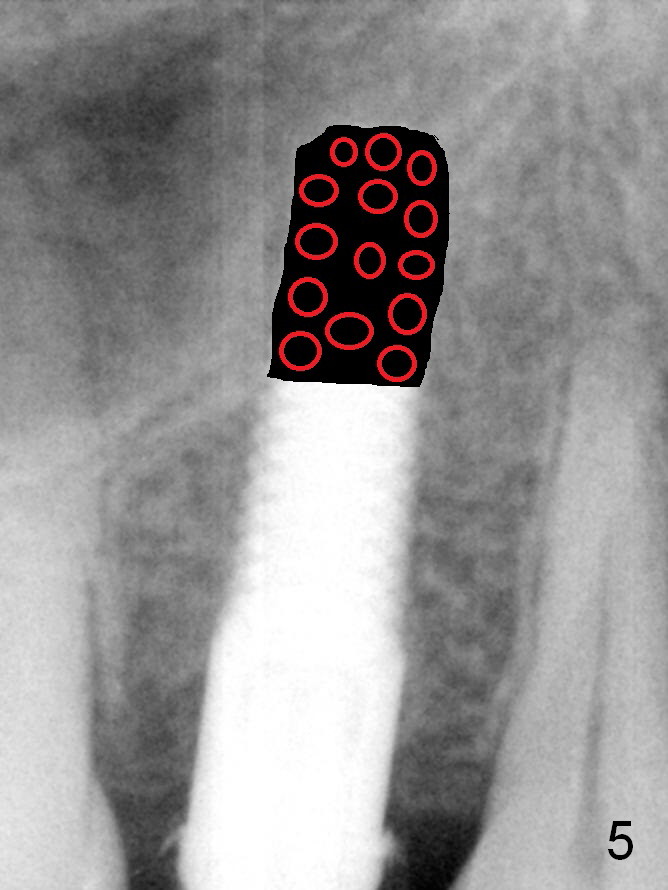
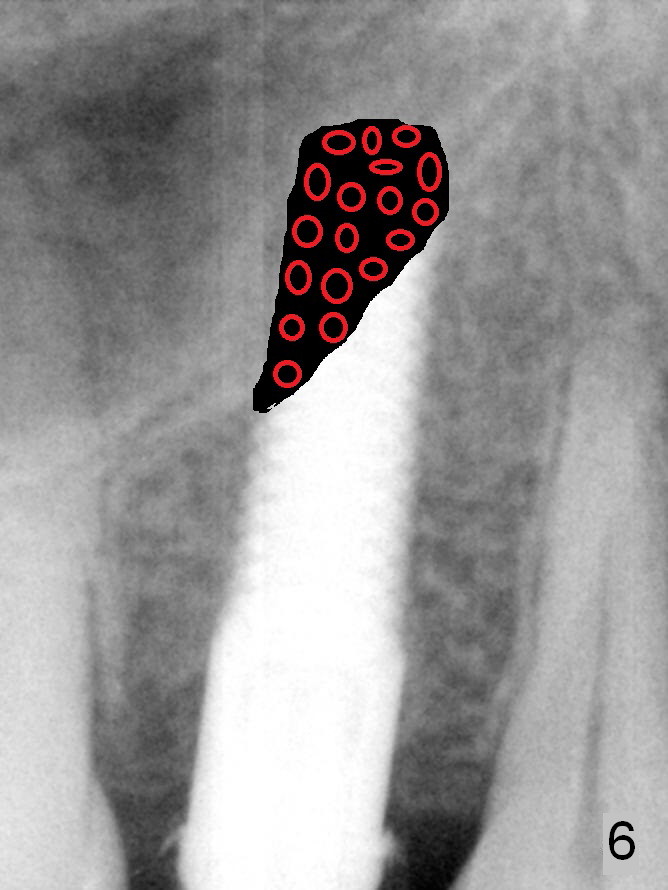
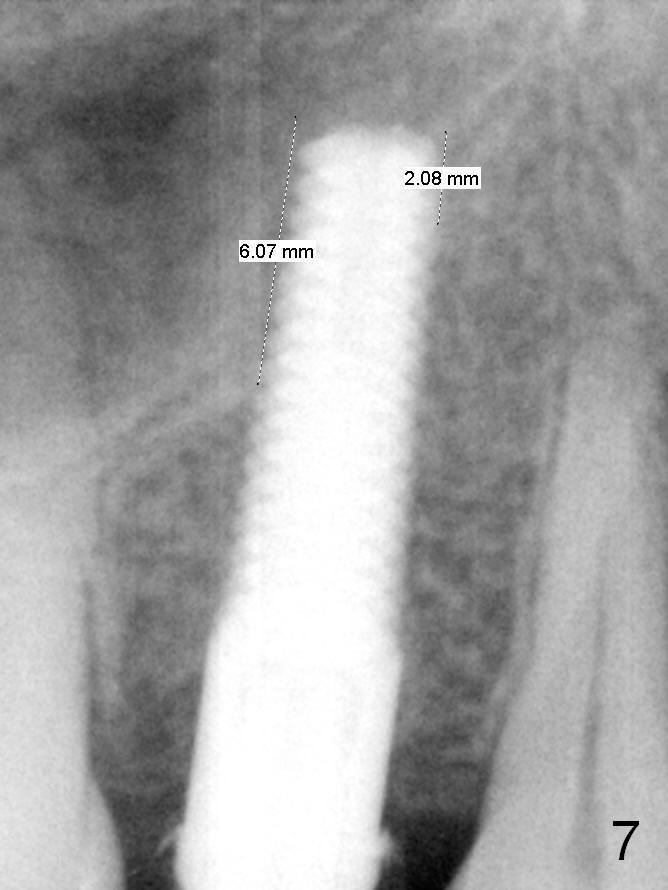
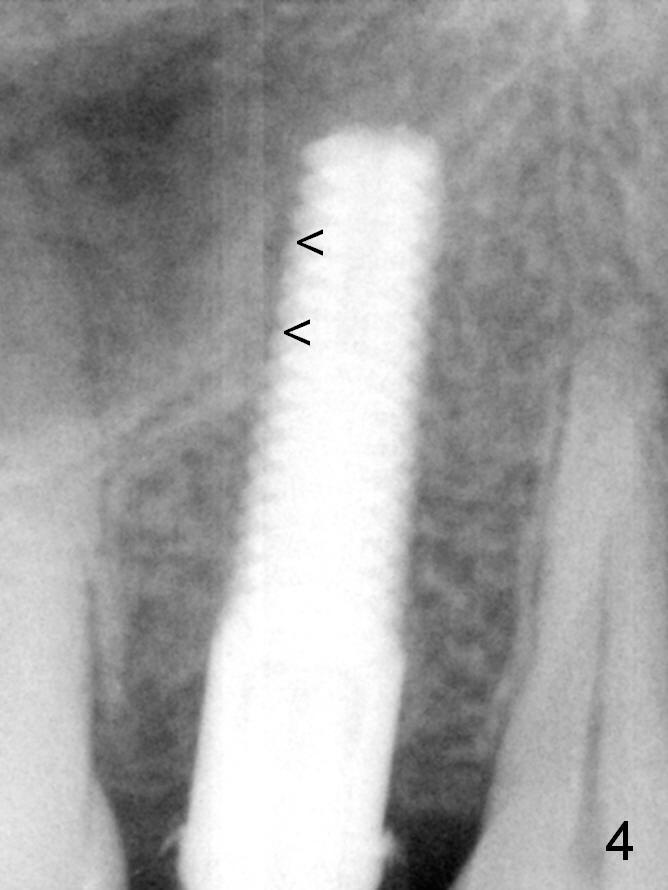
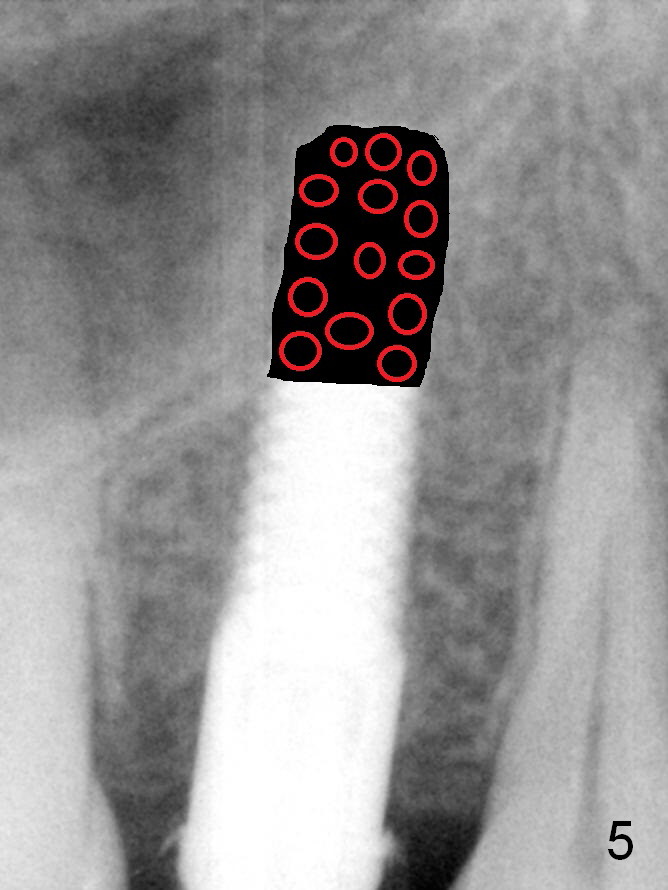
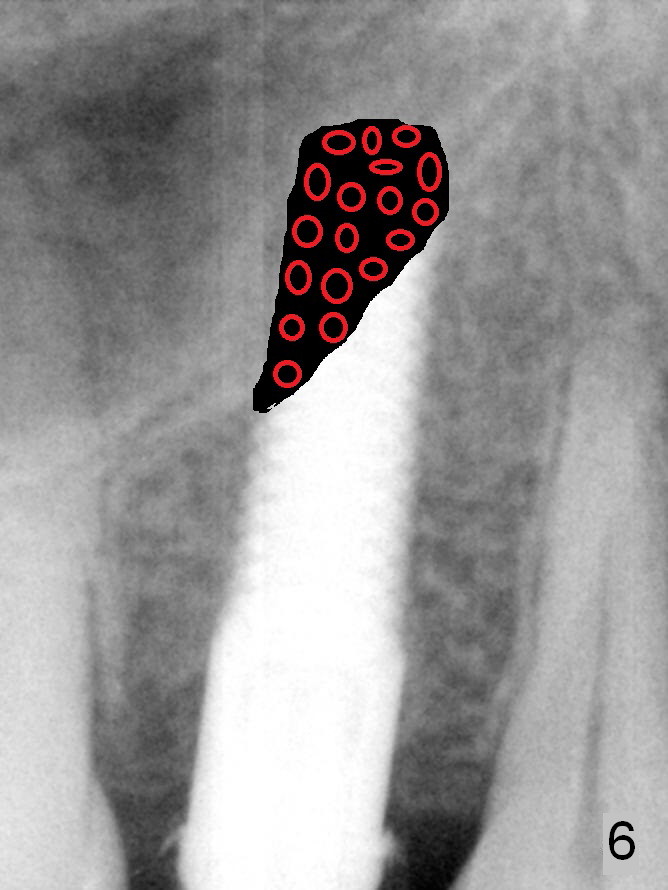
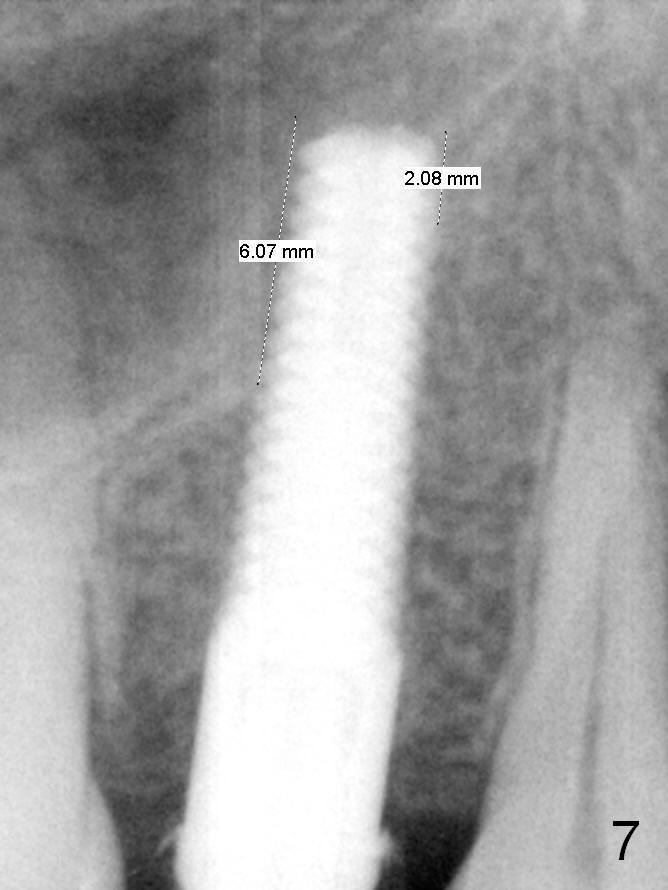
The patient has developed cervical-vertebral-disease-like symptoms without sign or symptom of sinusitis since the implant was placed. The symptoms has subsided in fact. Four-month postop PA shows a gap in the sinus (Fig.4). Subclinical sinusitis may occur. If the patient agrees, the implant will be removed, truncated about 6 mm transversely (Fig.5) or obliquely (Fig.6,7) and re-planted following bone grafting (red circles). Prepare Metronidazole for irrigation (~30 cc) and mixture with allograft (only).
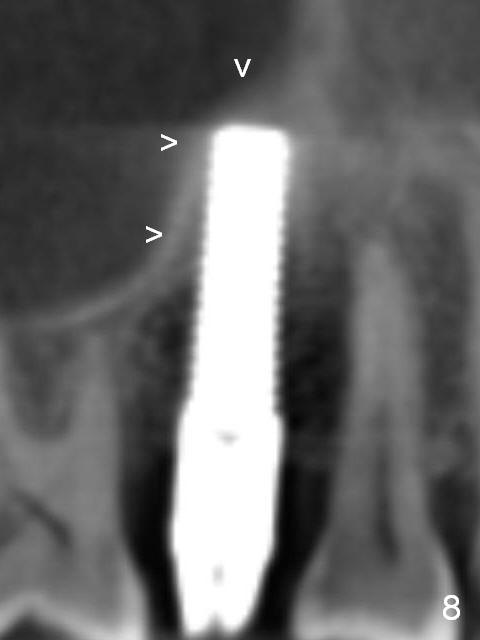
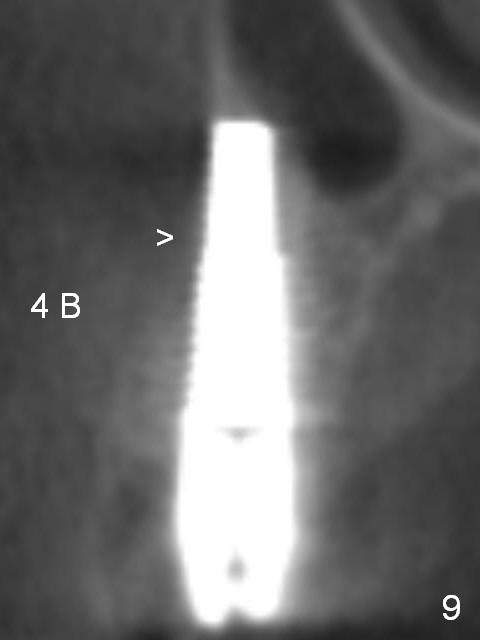
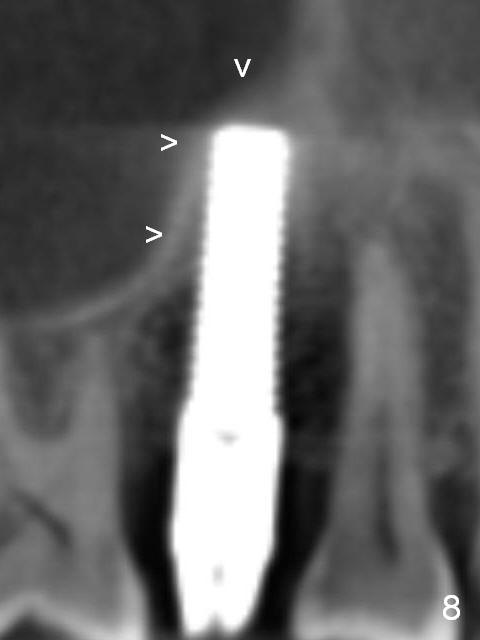
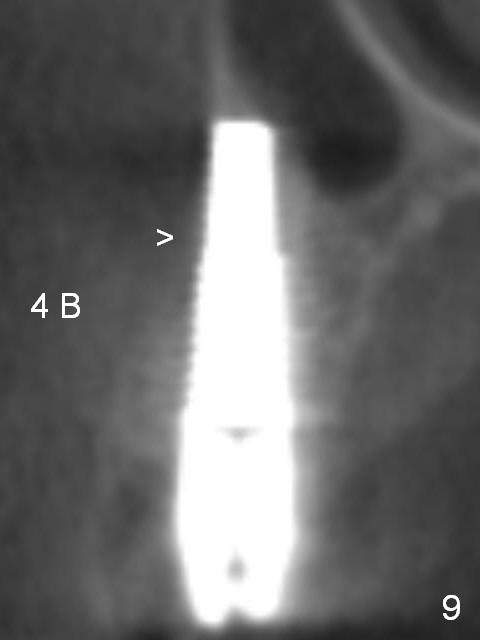
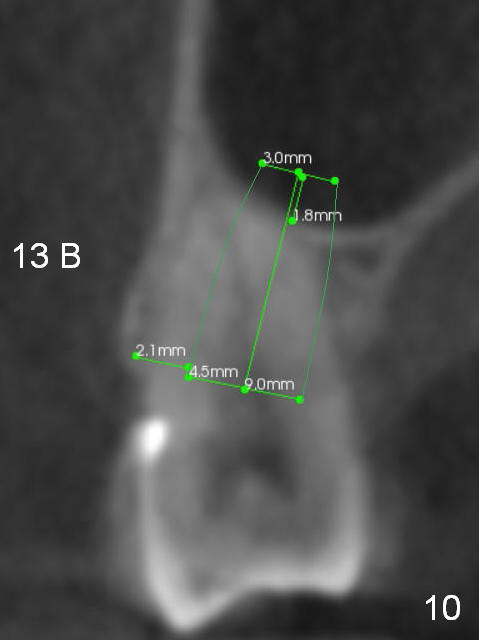
In fact, the patient does not want to have any more surgery. The abutment is cemented and impression is taken. CT taken 6 months 20 days postop shows that the elevated sinus floor heals over the implant (Fig.8 arrowheads). It appears that the apical portion of the buccal plate (B) has atrophied (Fig.9 (coronal section) above >; Fig.11 (axial section), as compared to Fig.10). The discomfort may derive from the tooth #28 (untreated pulpal exposure).
Return to Upper Premolar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 05/26/2016, last revision 12/16/2016