


.jpg)
%20trimmed,%20VeraGraft,%20plugs.jpg)

 |
 |
 |
|
 |
 |
 |
|
 |
.jpg) |
%20trimmed,%20VeraGraft,%20plugs.jpg) |
|
 |
 |
 |
 |
 |
|||
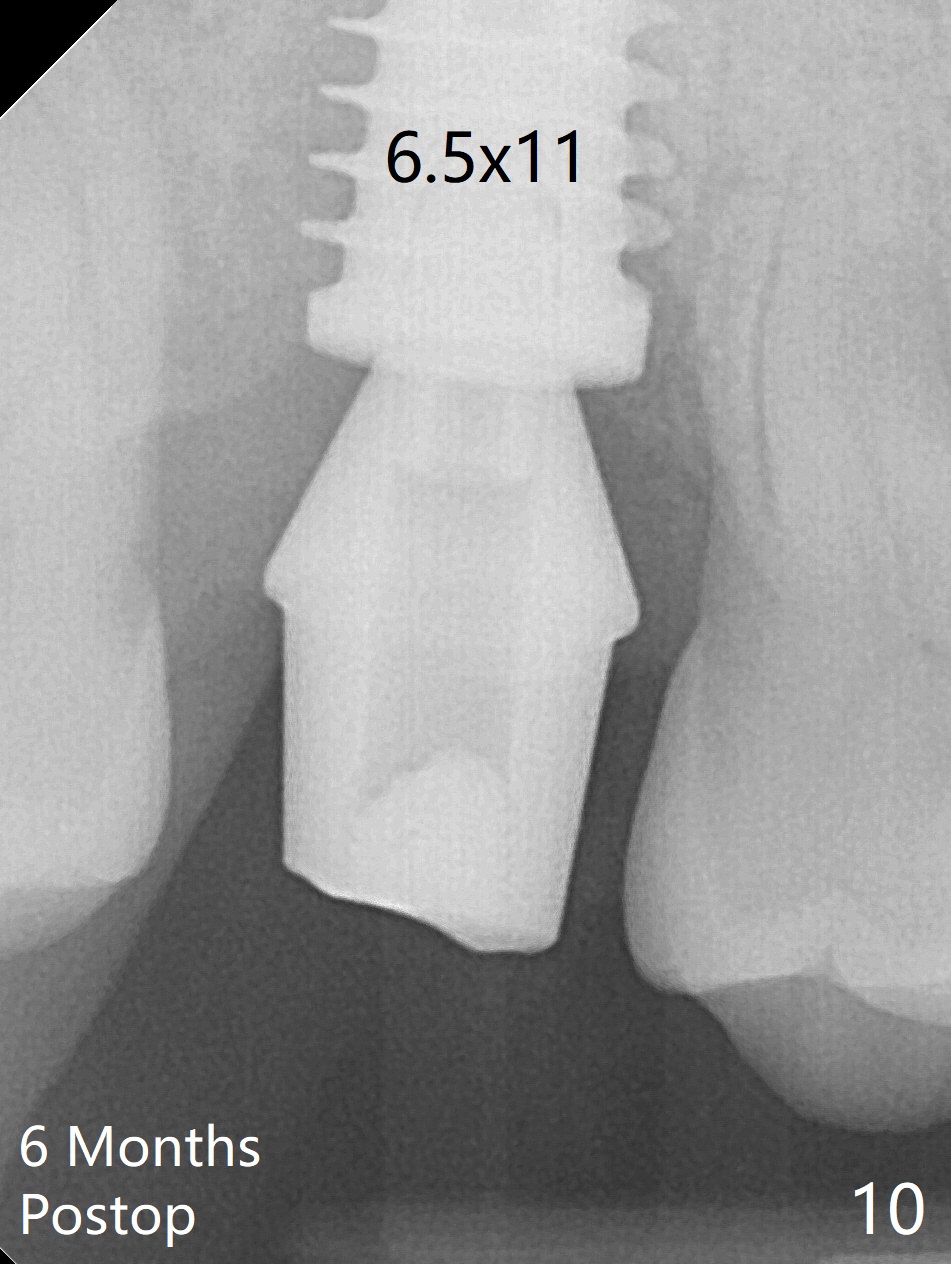
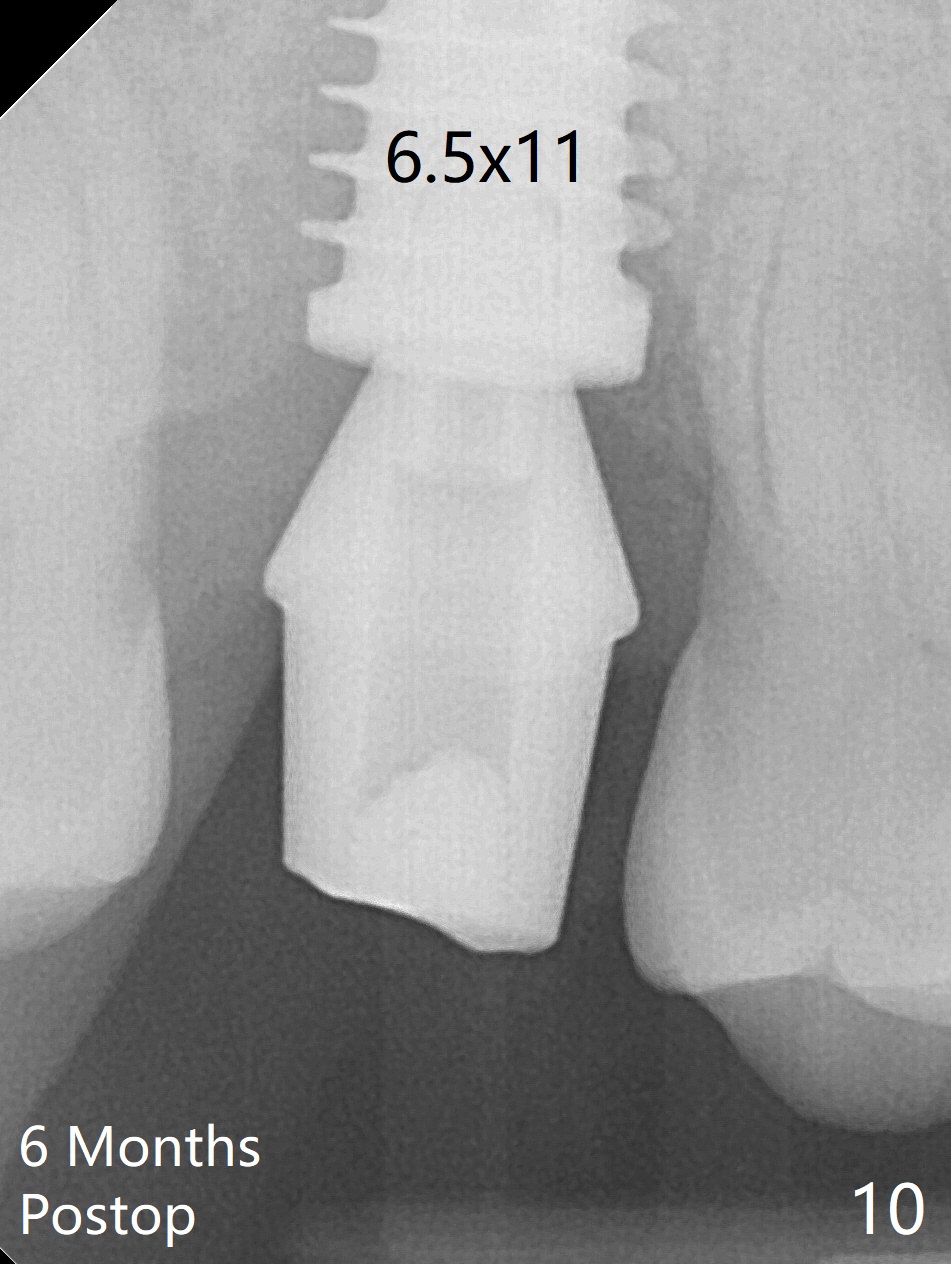
Approximately 3 mm Bone
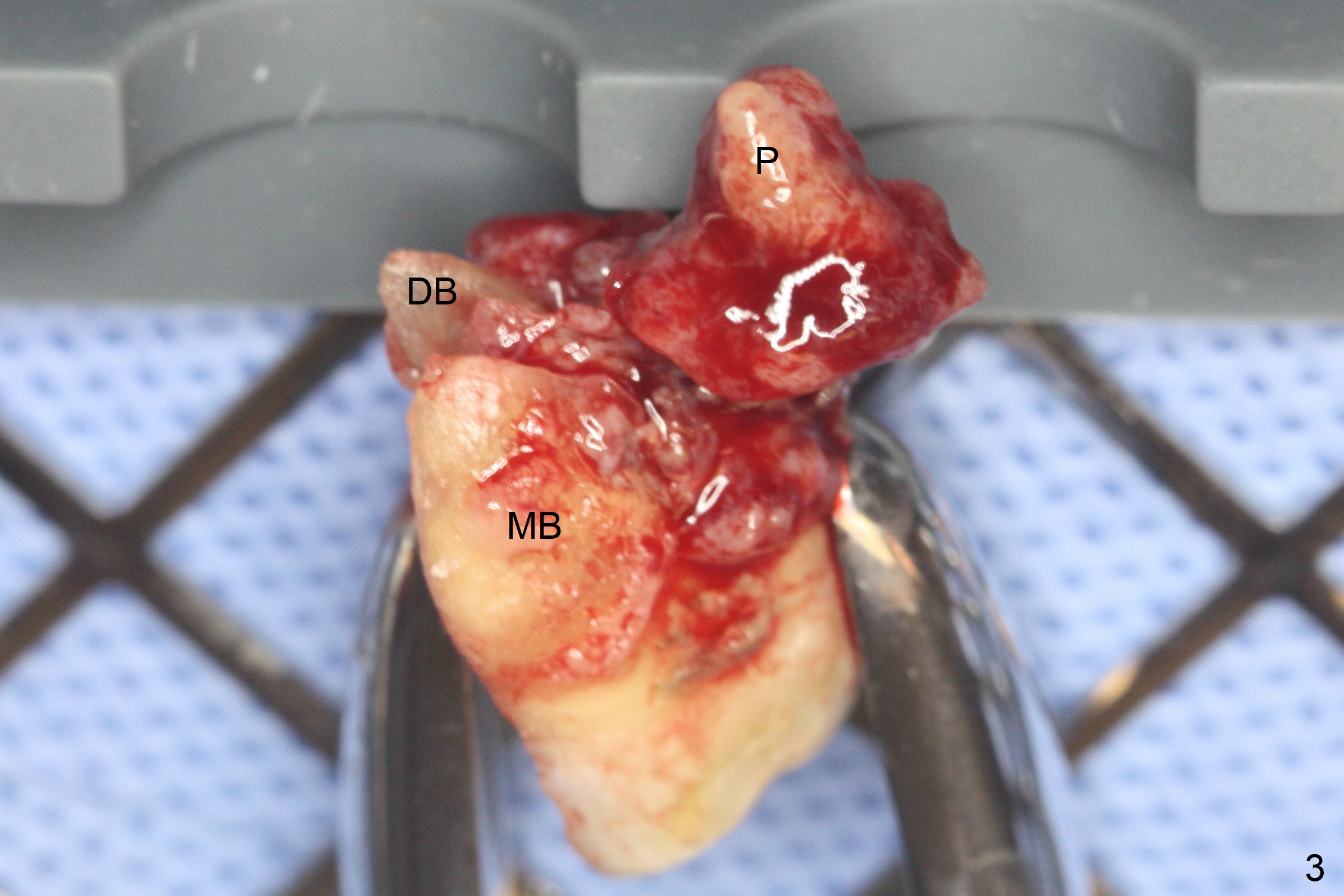
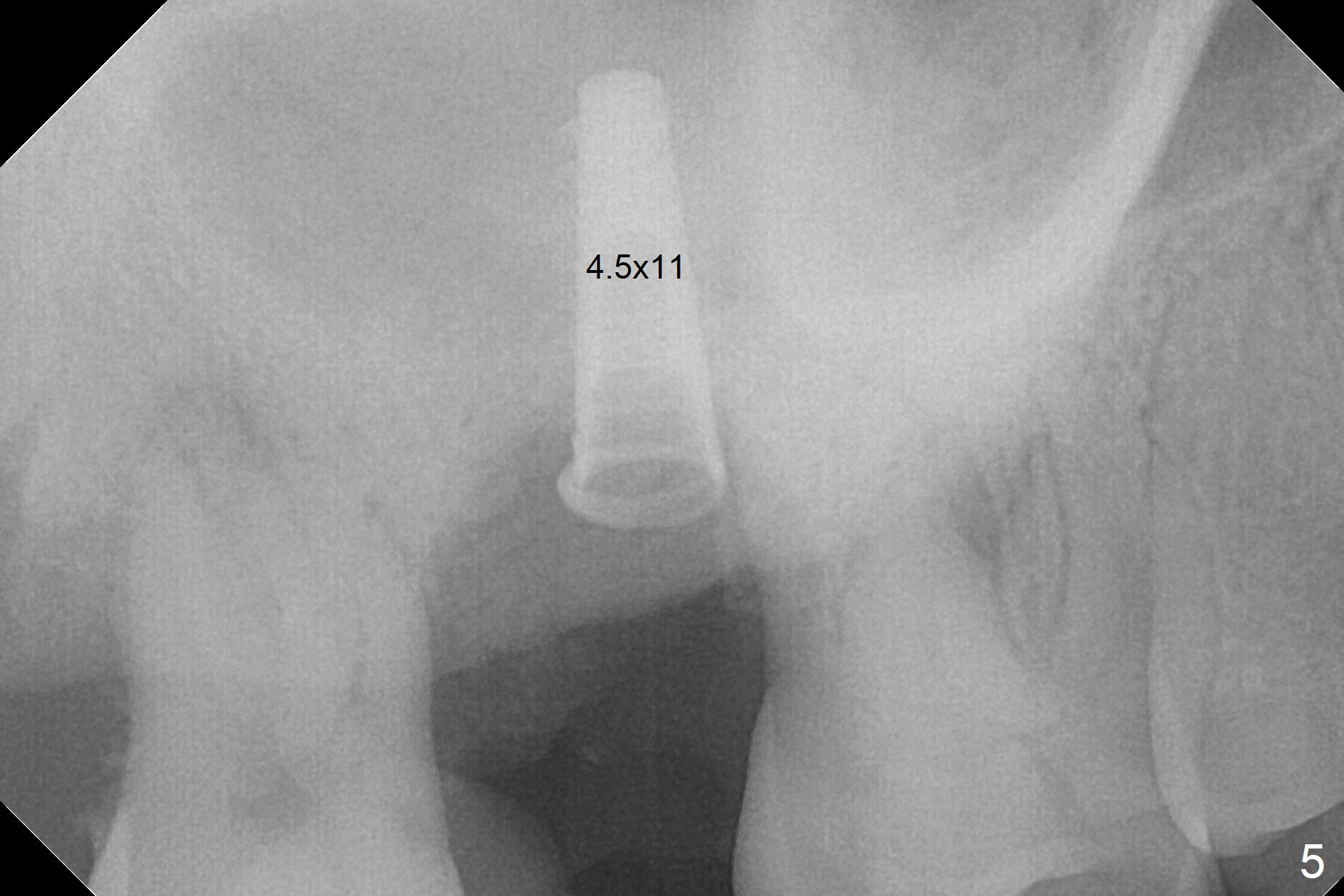
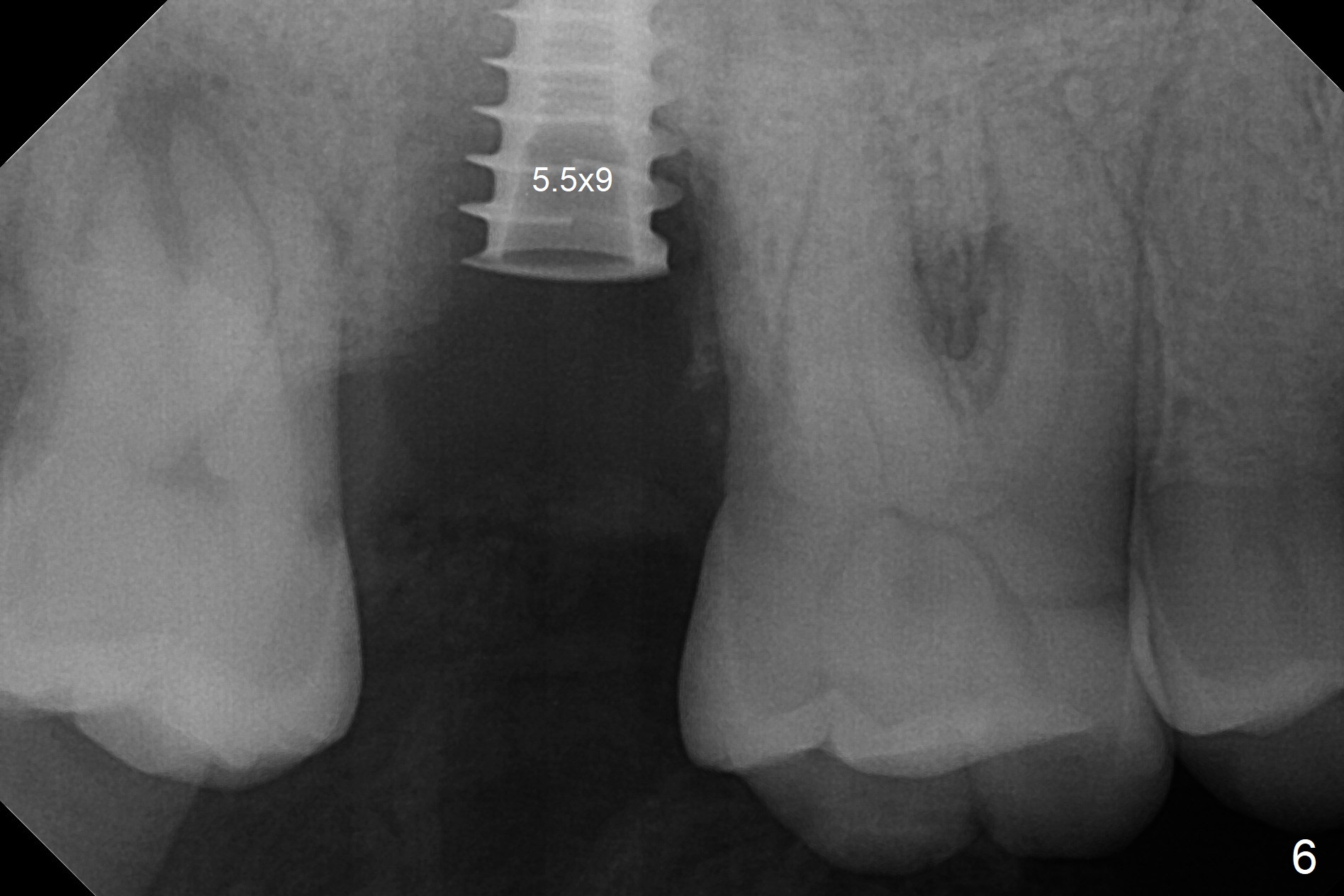
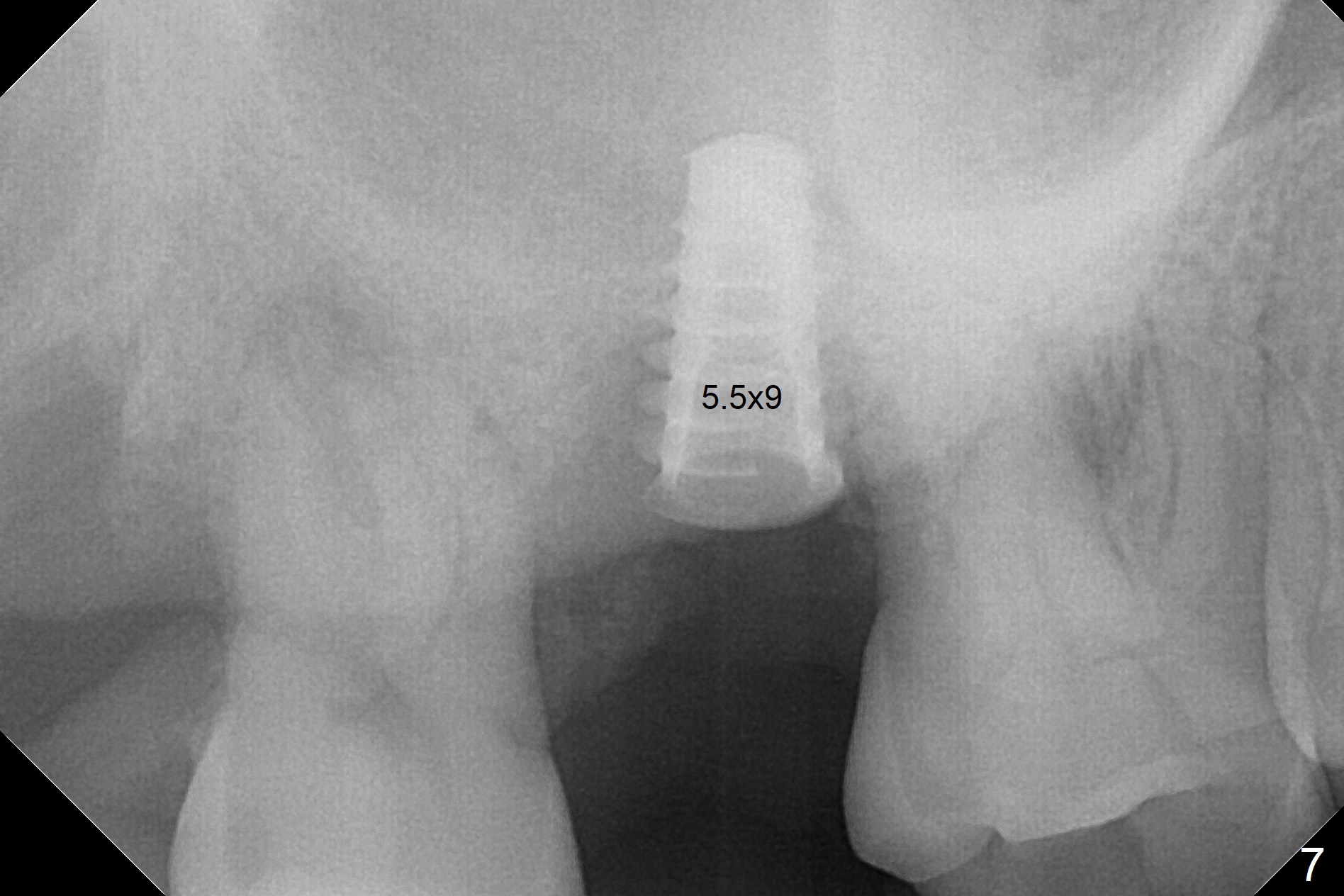
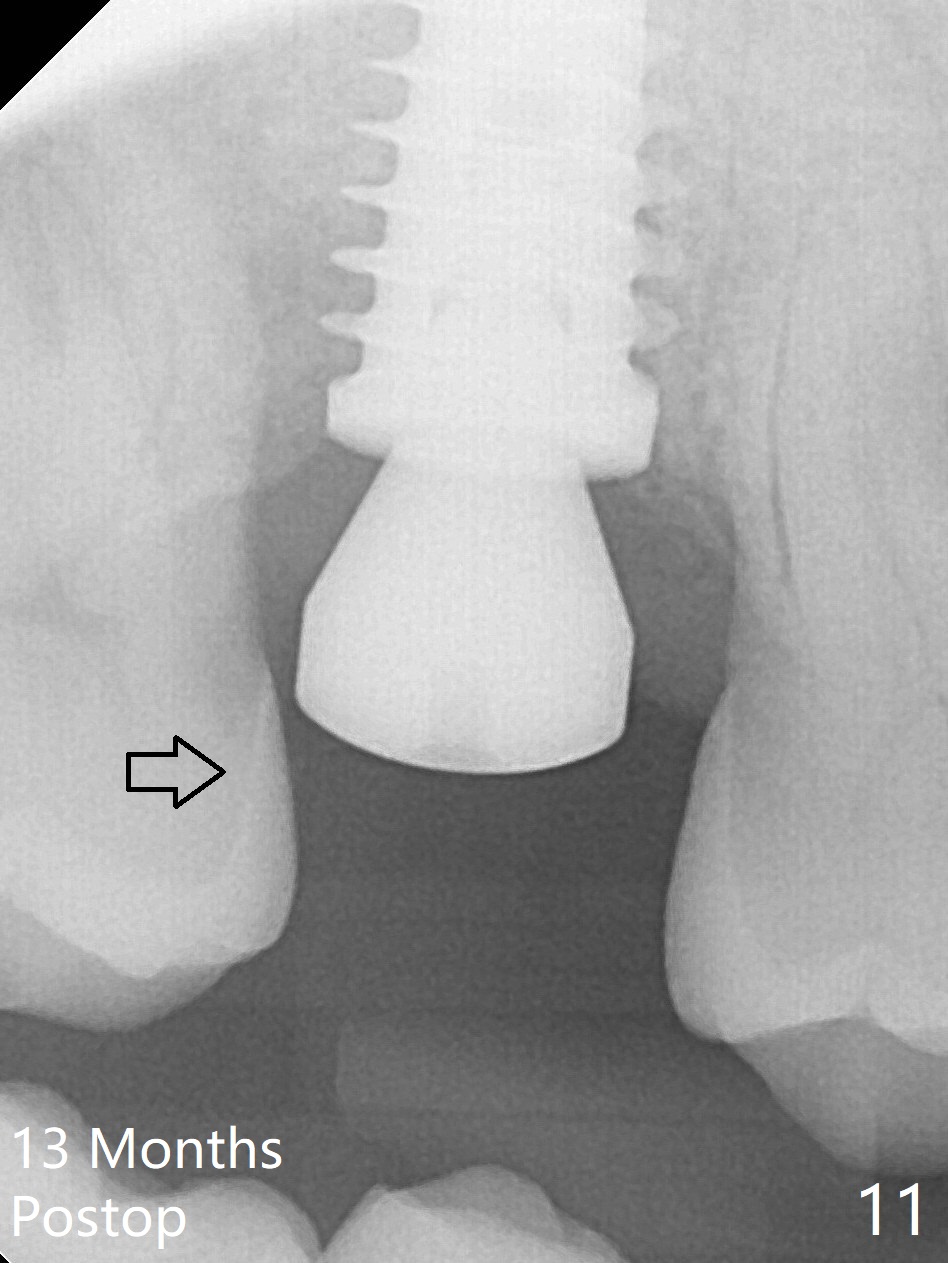
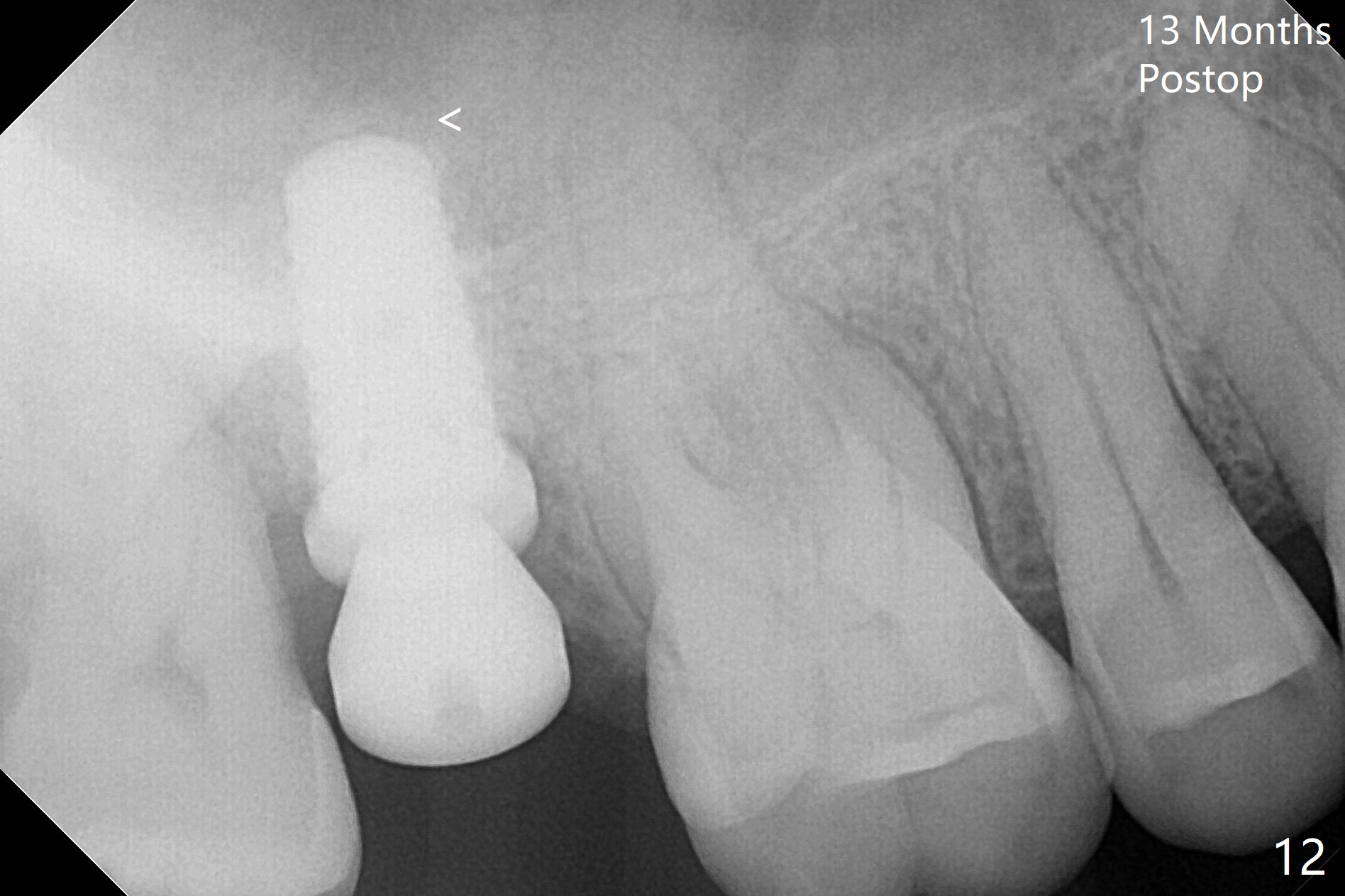
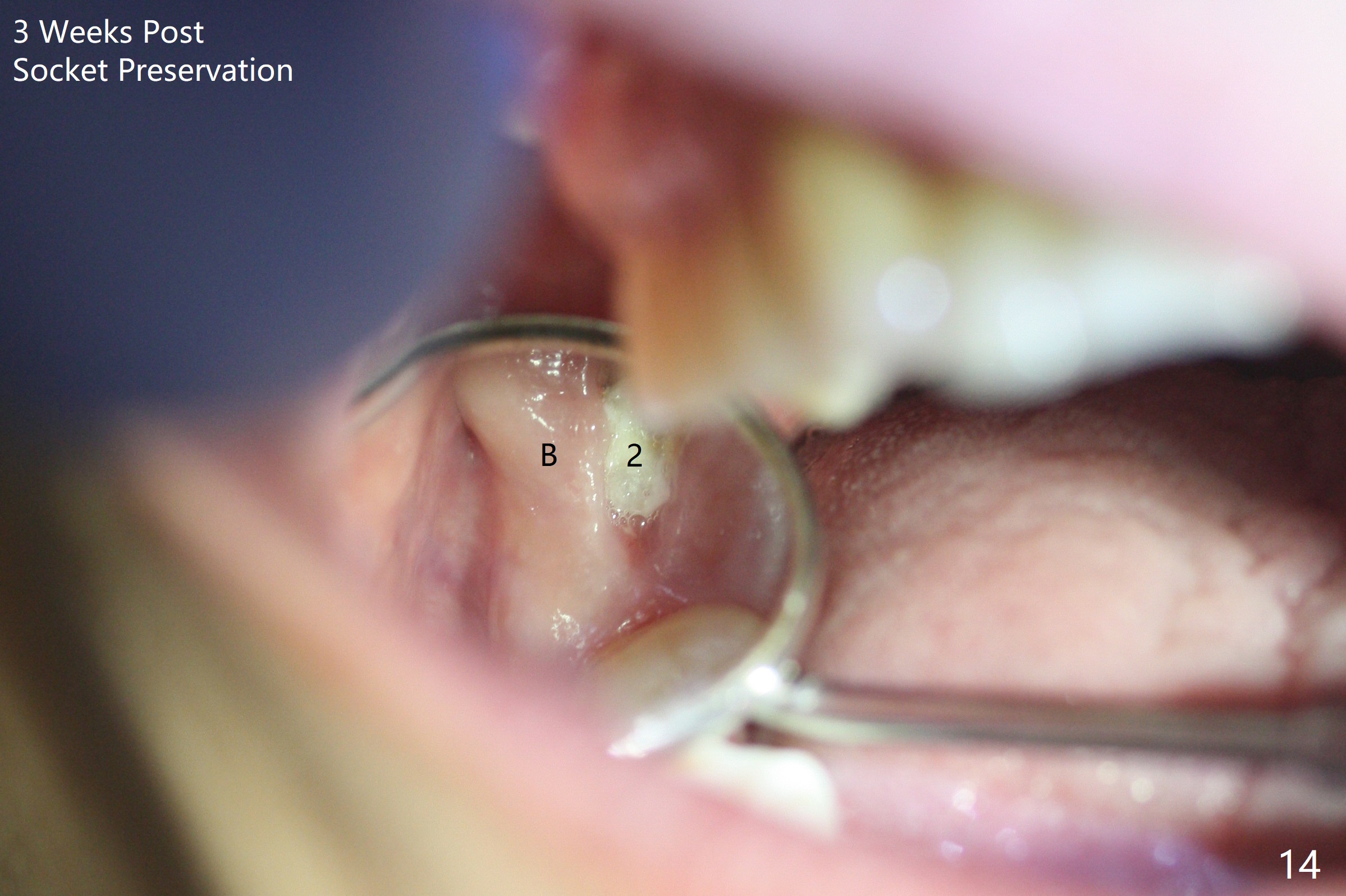
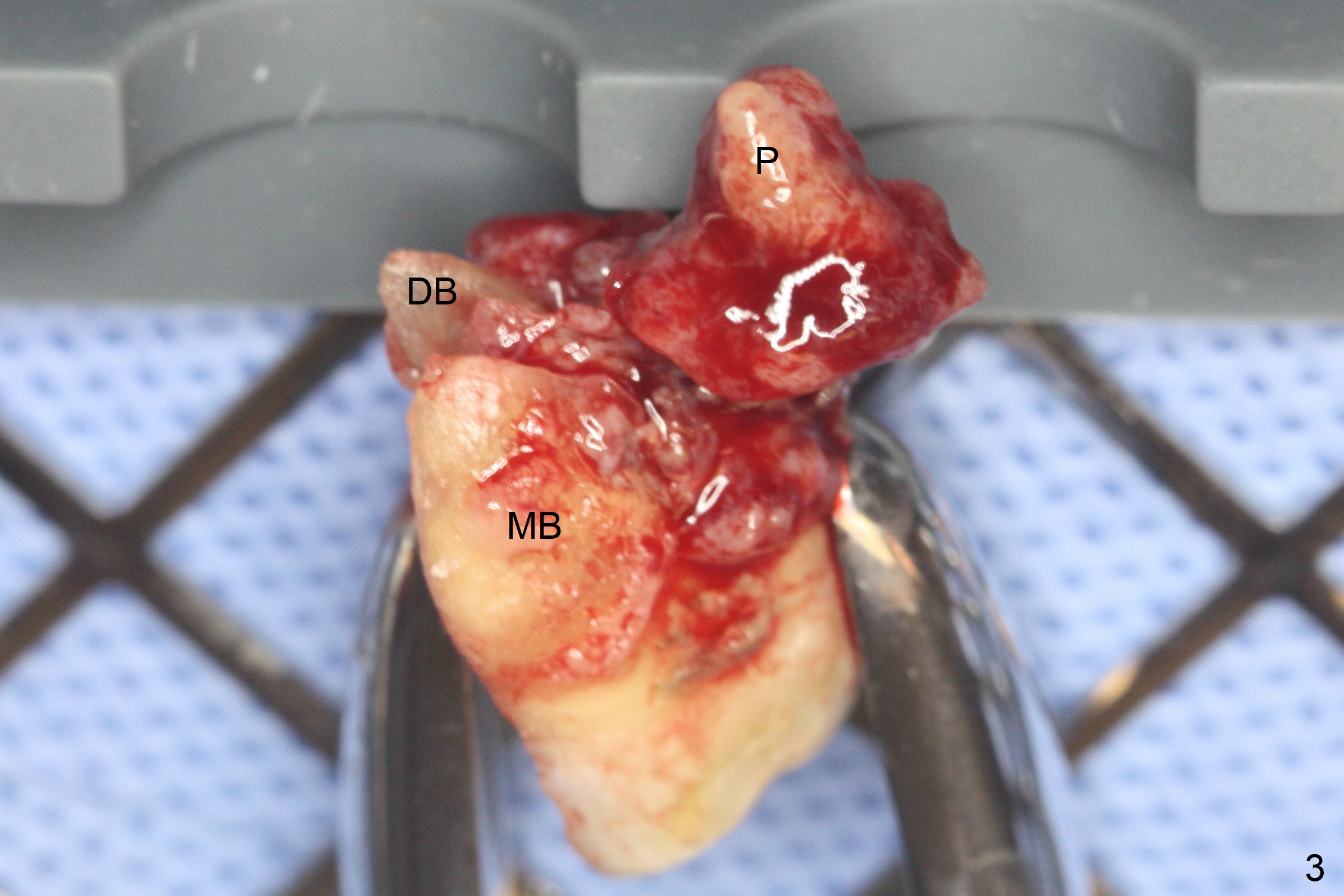
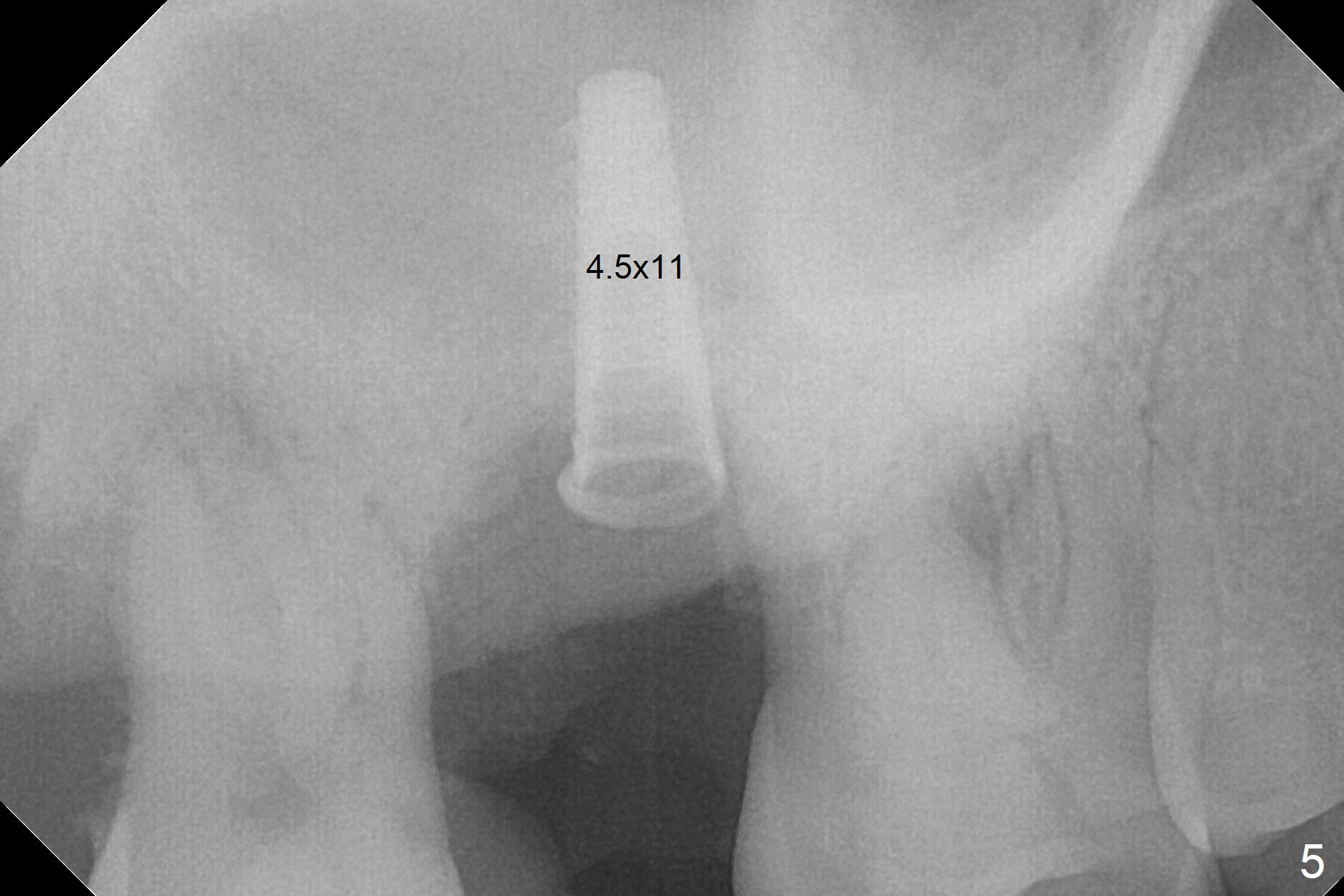
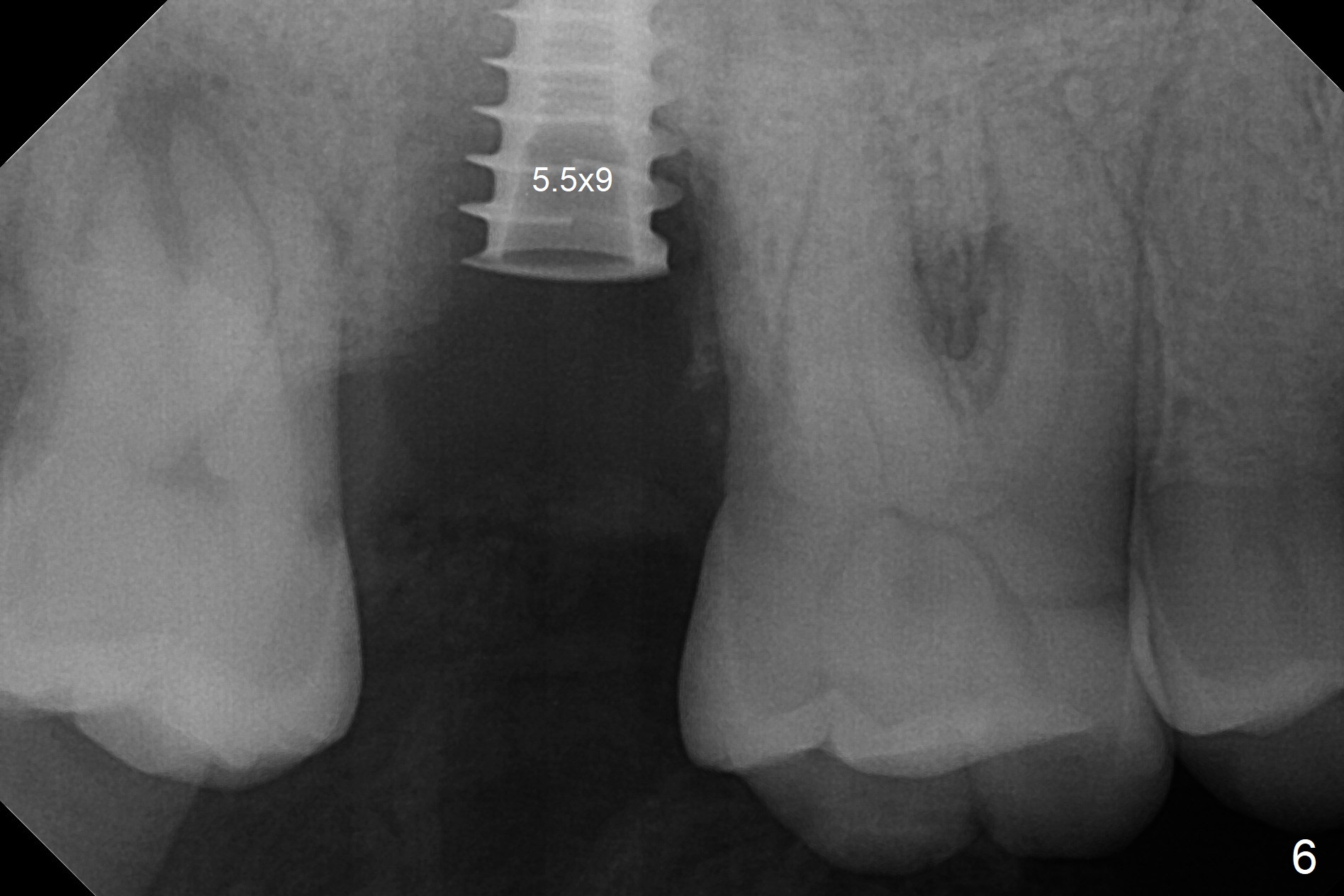
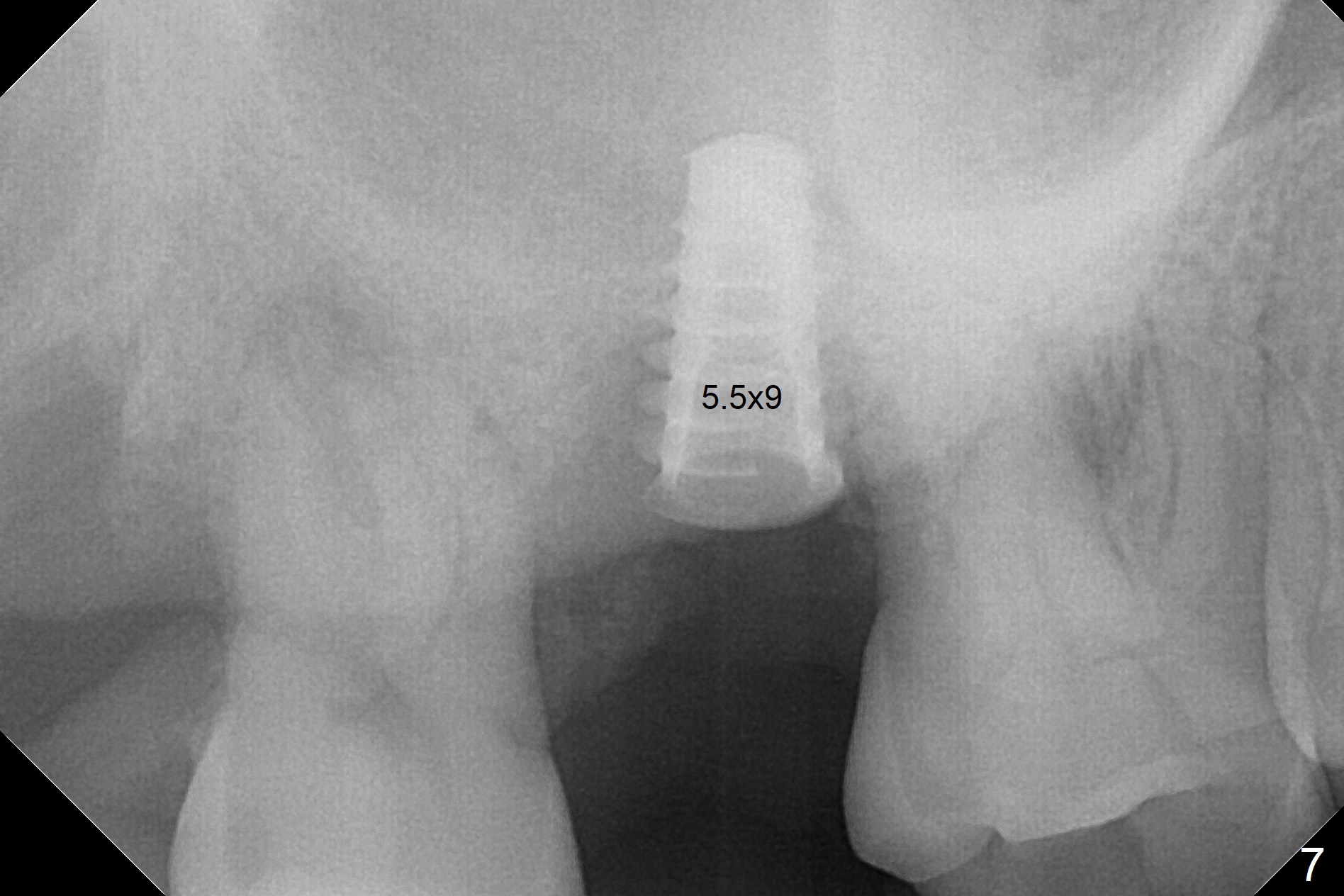
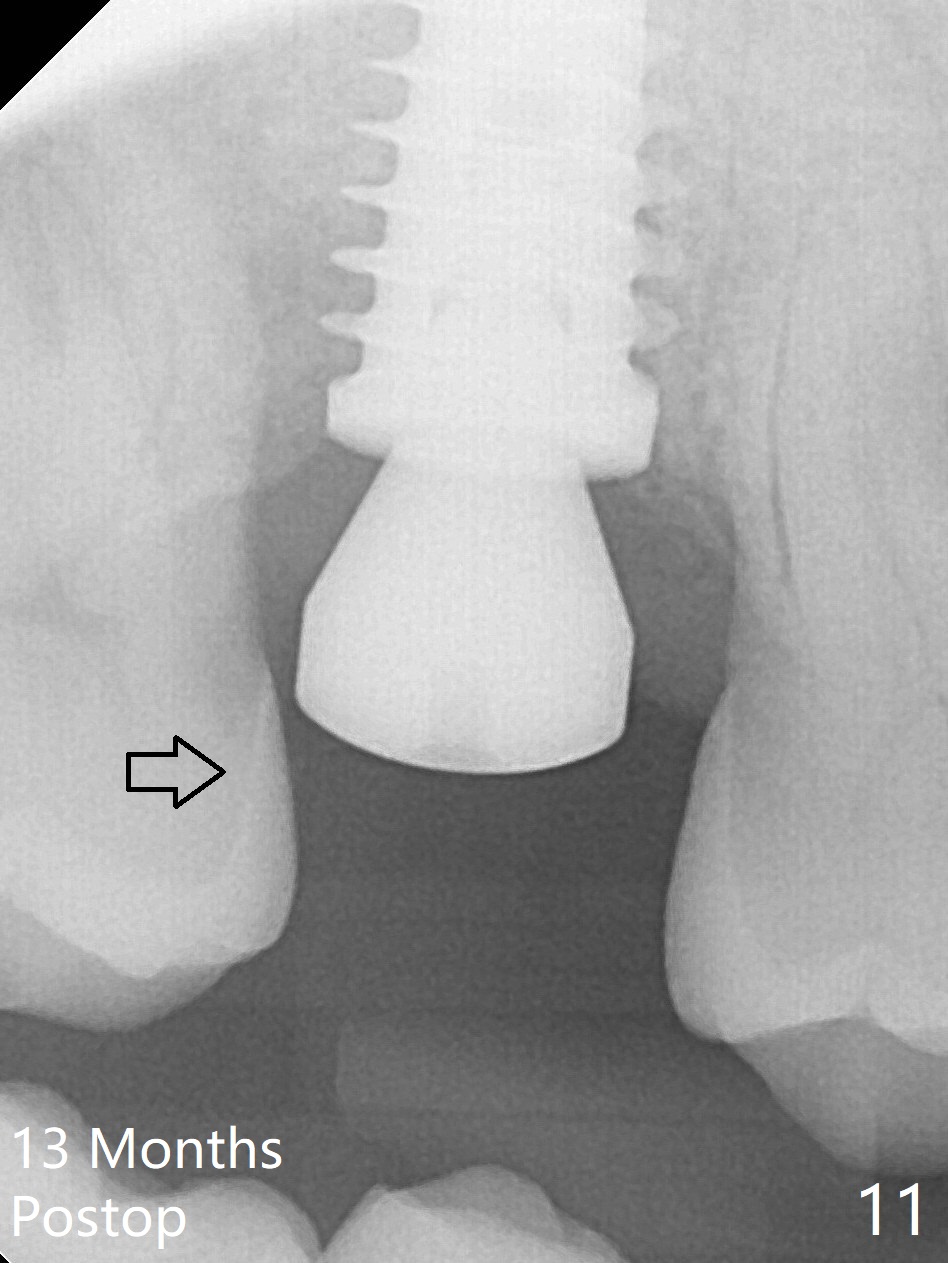
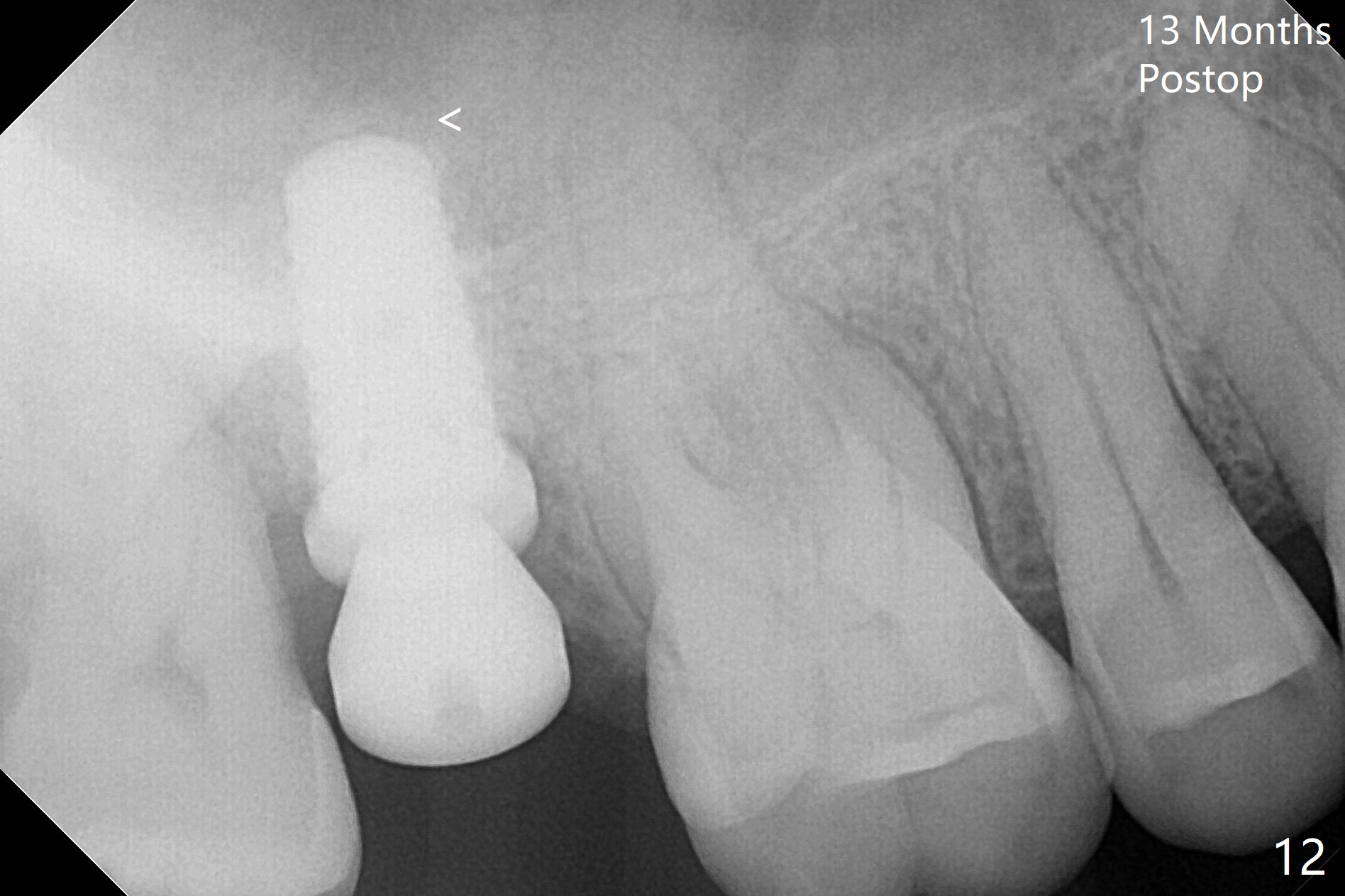
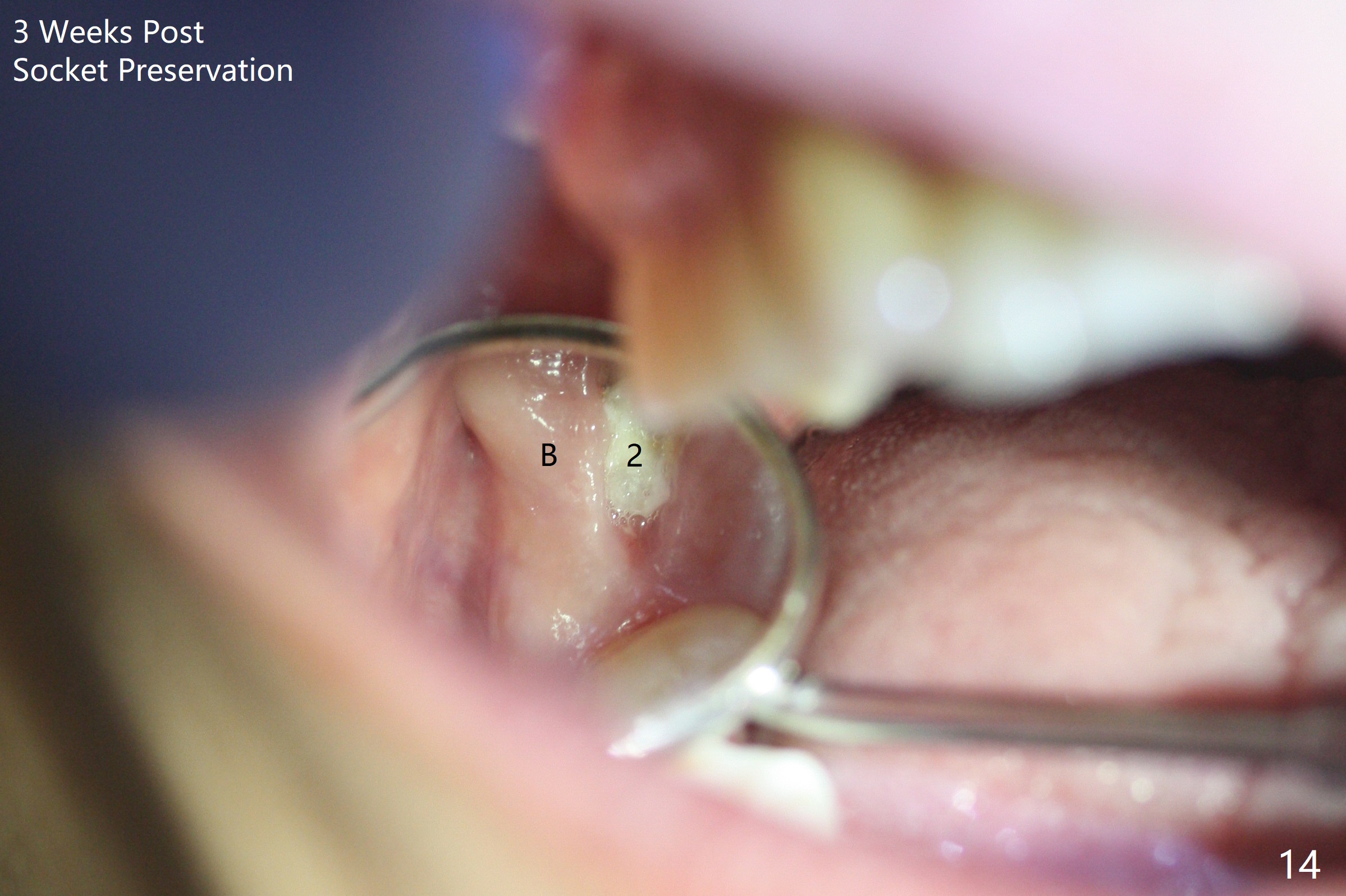
When the 59-year-old man returns for #24 implant placement, the tooth #2 is found to have crack (Fig.1,2 arrowheads), associated with buccal and palatal fistulae (*) and loss of amalgam (Fig.4 *). Abundant granulation tissue is attached to the roots of the affected tooth (Fig.3), indicating severe bone loss. There is a plateau associated with the septum and buccal sockets, which is the site of osteotomy. Magic split and 3 and 3.8 mm Magic Expanders are used to initiate osteotomy. After use of 4.3 mm Magic Drill for about 3 mm, Osteogen plug and allograft are used for sinus lift, followed by insertion of a 4.5x11 mm dummy implant (Fig.5). When a 5.5x9 mm dummy implant is placed with stability, it appears to be seated cervical (Fig.6,7). When a 6x9 mm IBS implant (definitive) is placed with a 6.5x5.5(4) mm abutment, they are seated too deep for provisional (Fig.8). The implant/abutment are removed and replaced by a 6.5x11 mm one in a shallower position; after trimming the same abutment as mentioned above (Fig.9), an immediate provisional is fabricated to keep bone graft in place. Fabrication of Tap with soft tissue markers will reduce the chance of miscalculation and waste of implants. The coronal threads of the implant are covered with bone 6 months postop (Fig.10). One month later when a permanent crown tries in, the implant is found to be loose and tender. A healing abutment is placed. Six months later, the patient returns for crown retry-in. The tooth #1 seems to have shifted mesially (Fig.11 arrow). When the abutment is placed, the implant remains tender and loose. After implant removal with a wrench, there is no granulation tissue or bony defect, including the intact sinus floor (Fig.12 <). Since the tooth #1 has deep periodontal pockets and mobility, the tooth is extracted with abundant granulation tissue. After debridement, Osteogen plug is placed in the socket of #1, while Vanilla graft is placed at the site of #2 (Fig.13 *). Three weeks later, the socket of #2 heals with exposure of Osteogen plug (Fig.14 (B: buccal)).
Return to
Upper
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table),
Clindamycin,
Failed
Case One Day Earlier,
Course
2
3
4
Xin Wei, DDS, PhD, MS 1st edition 08/05/2017, last revision 09/23/2018