

 |
 |
 |
|||
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
||
Complete Tooth Crack Causes Large Defect
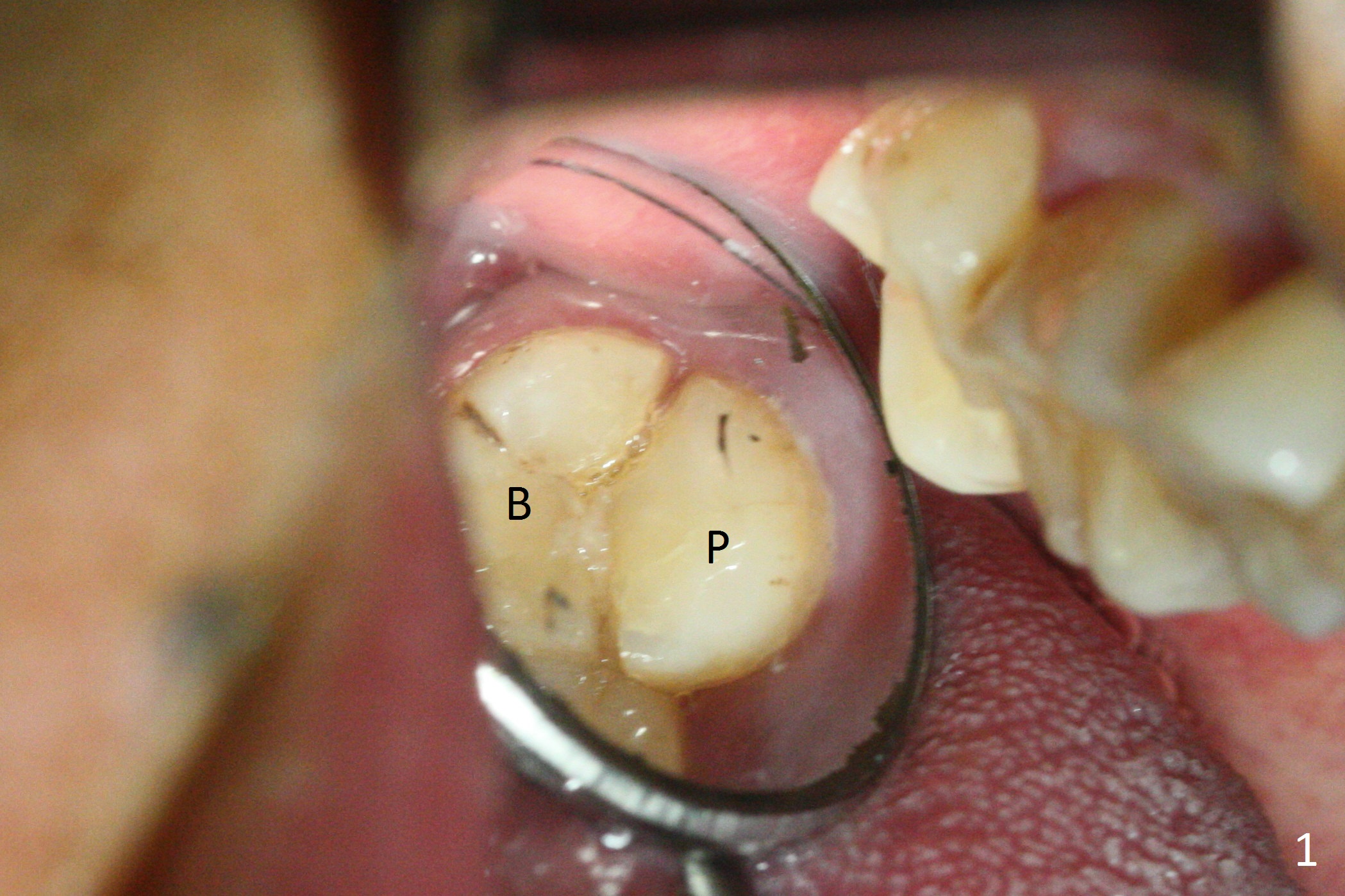
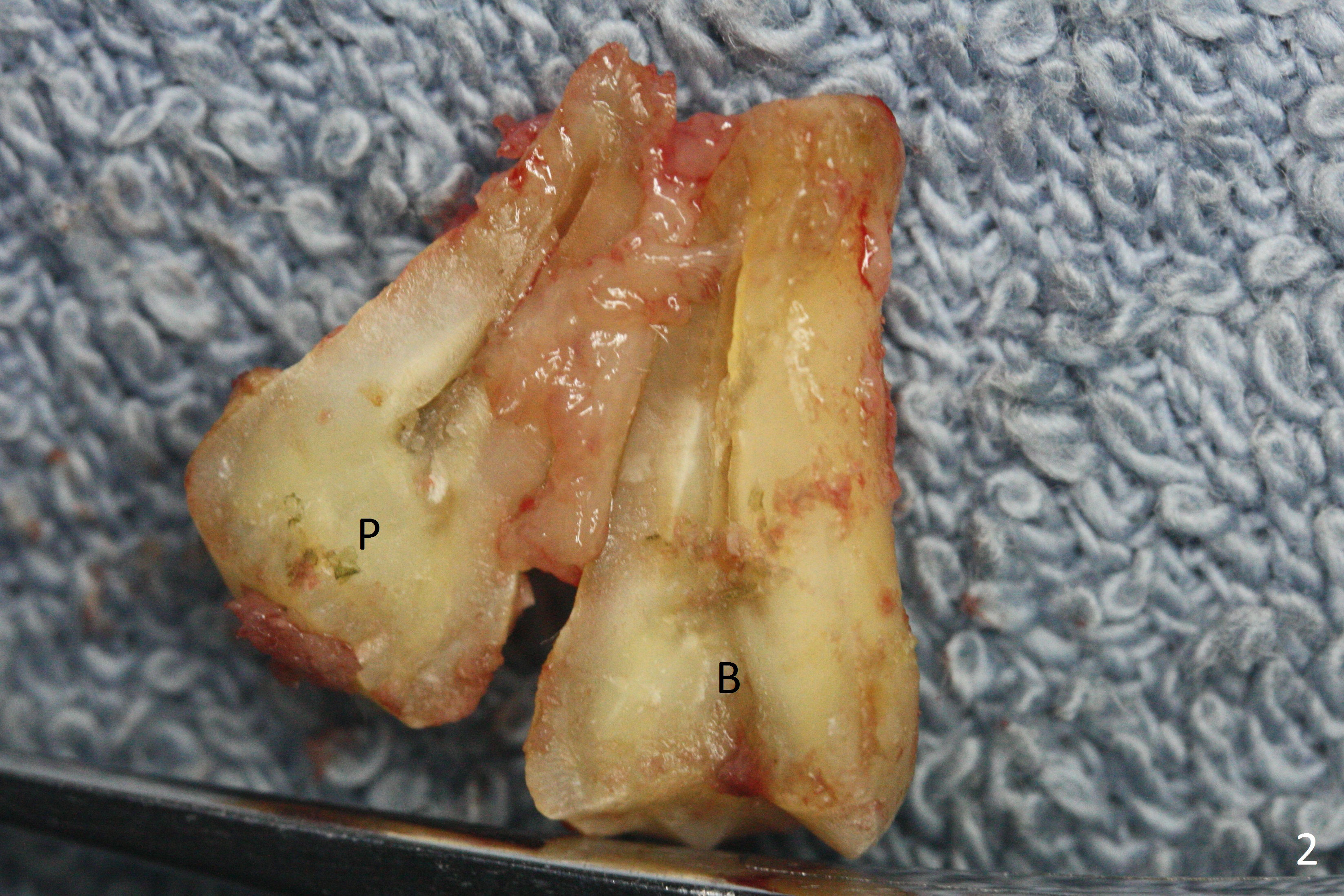
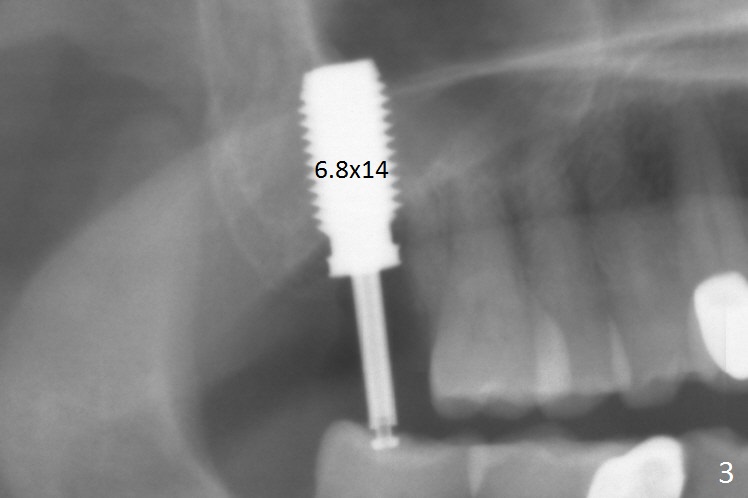
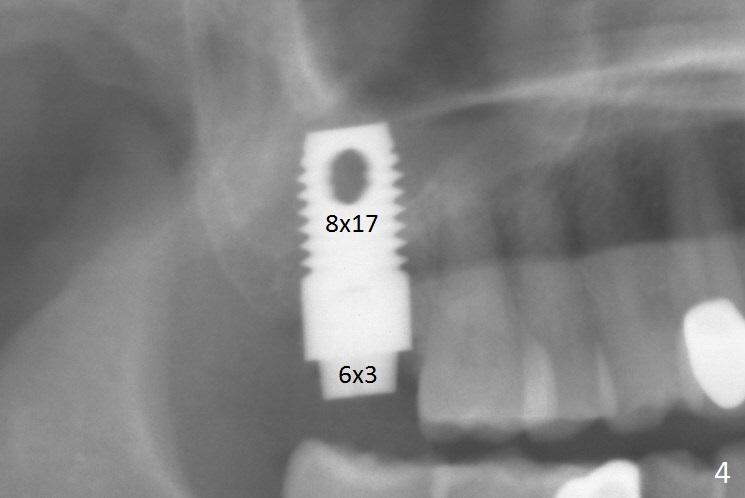
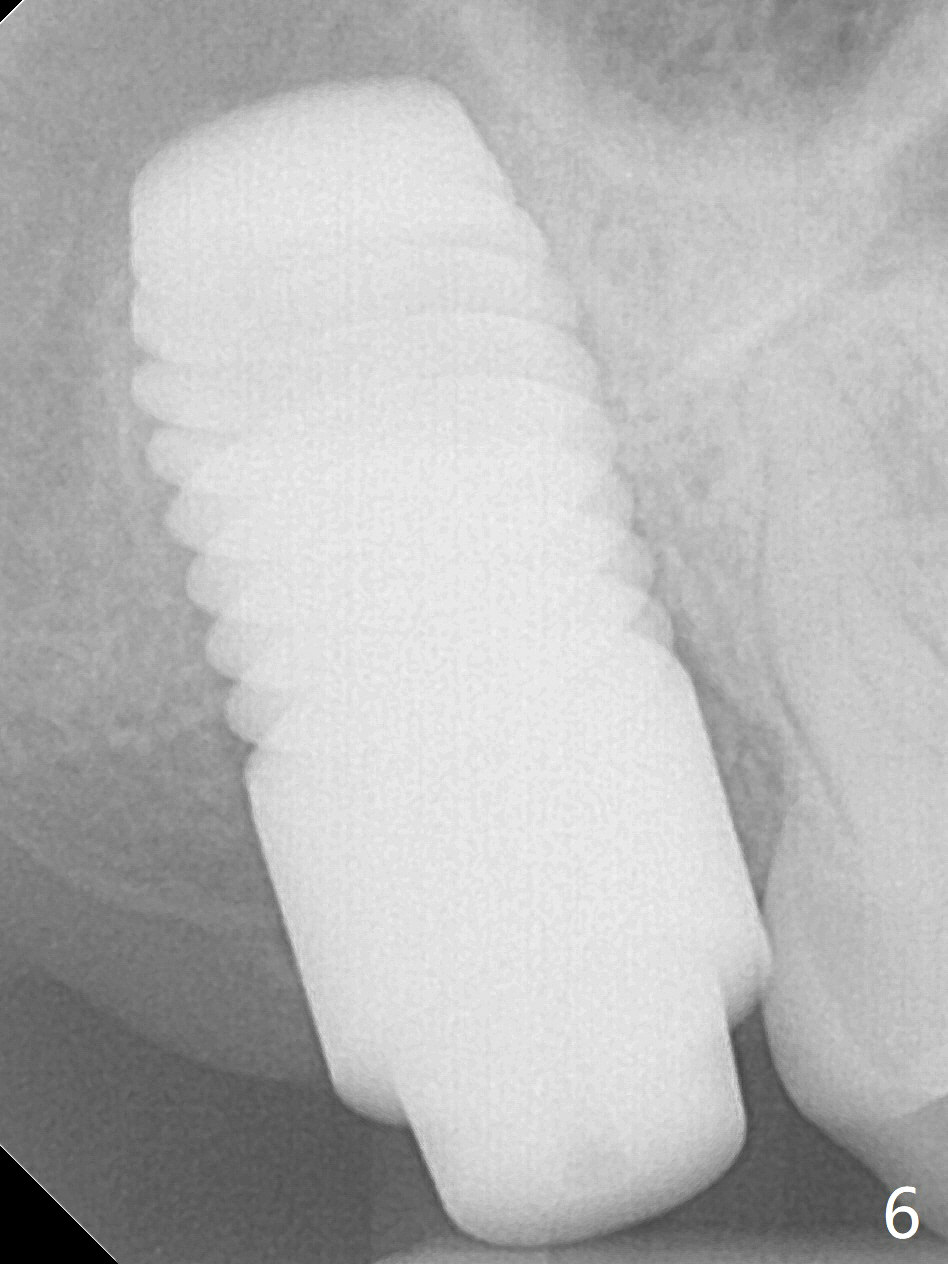
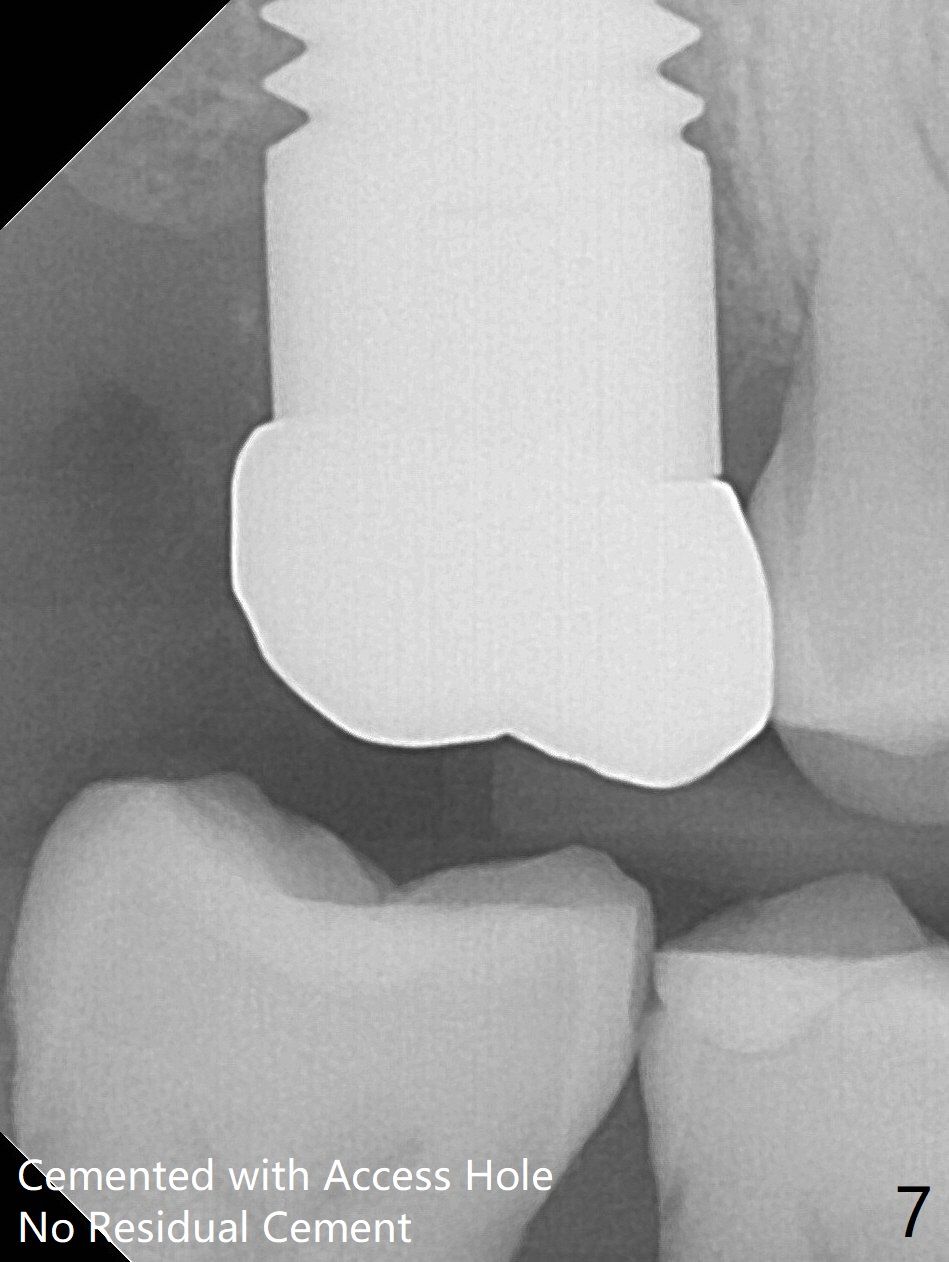
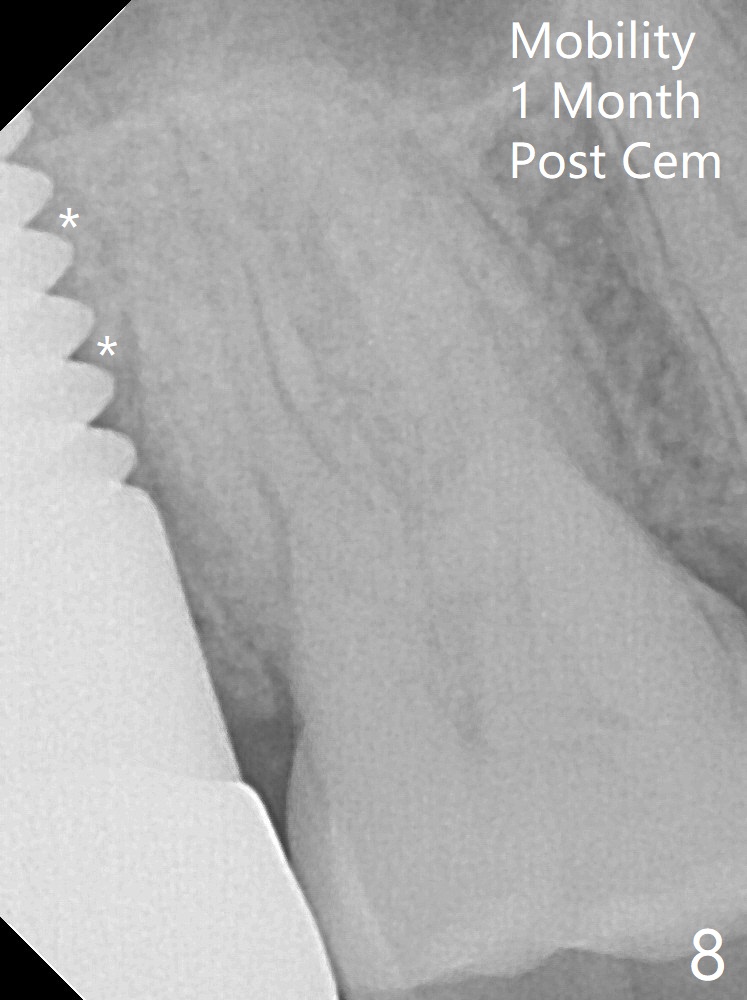
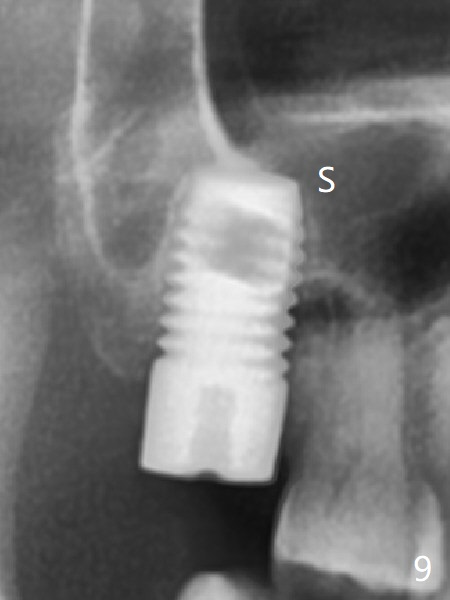
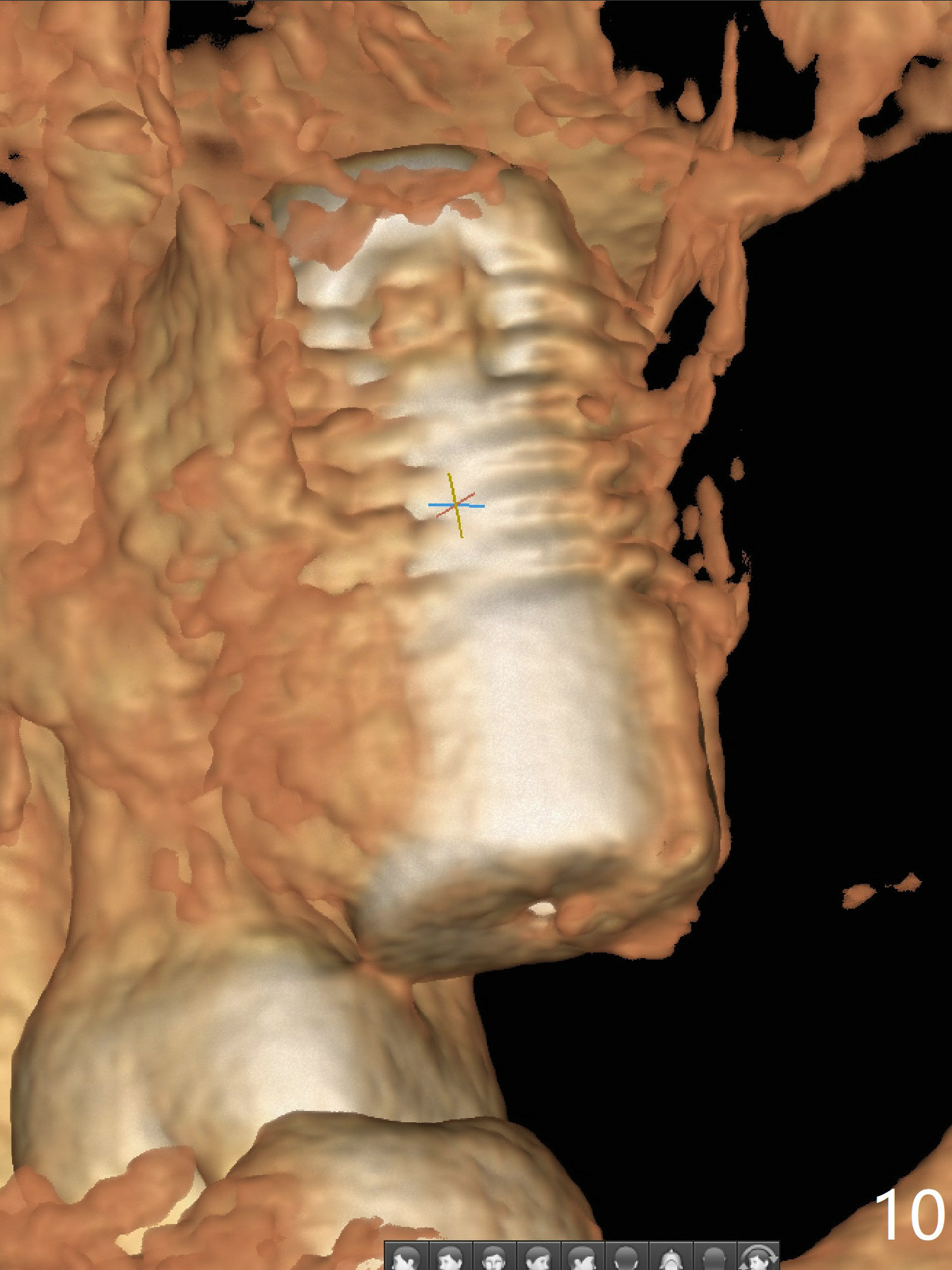
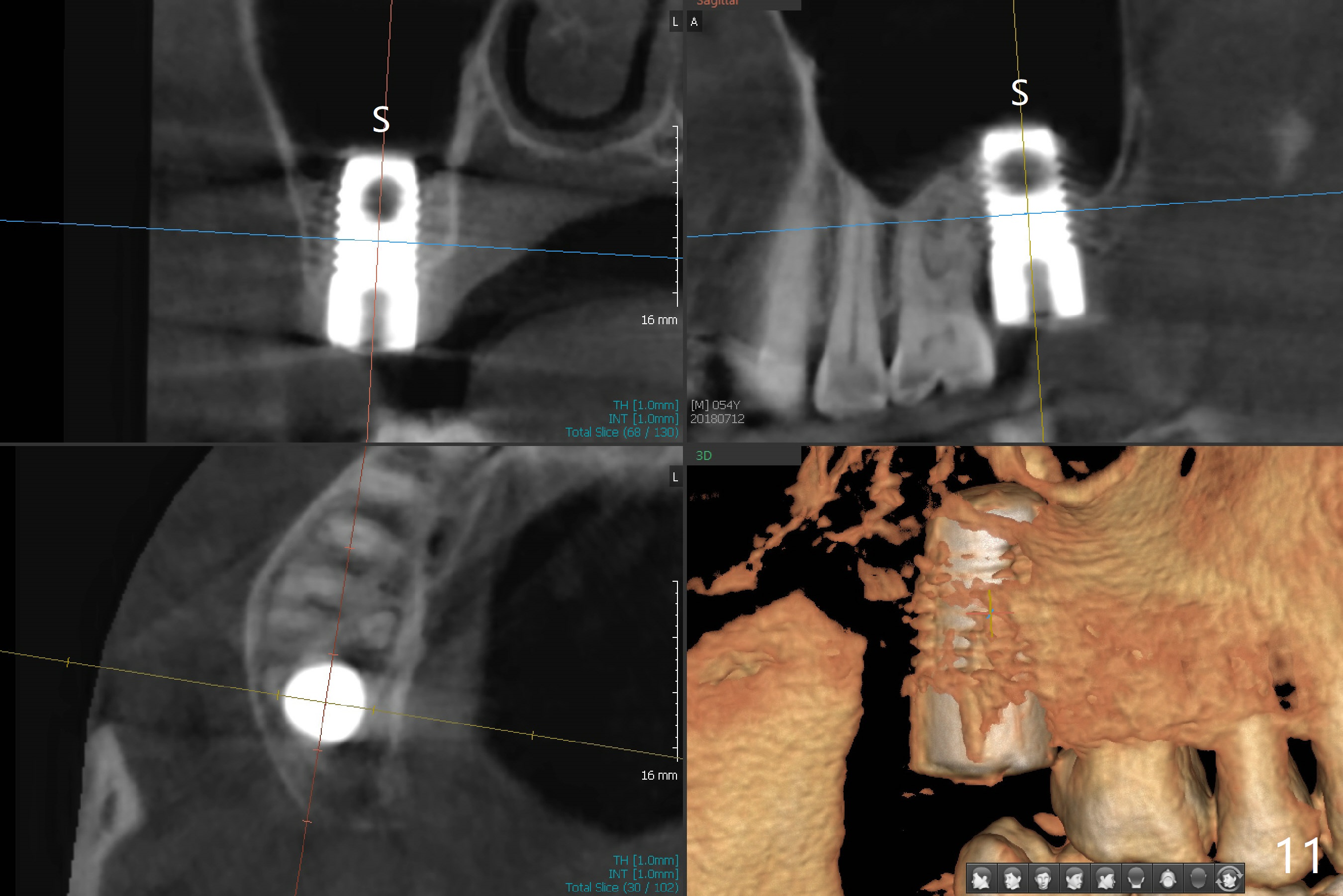
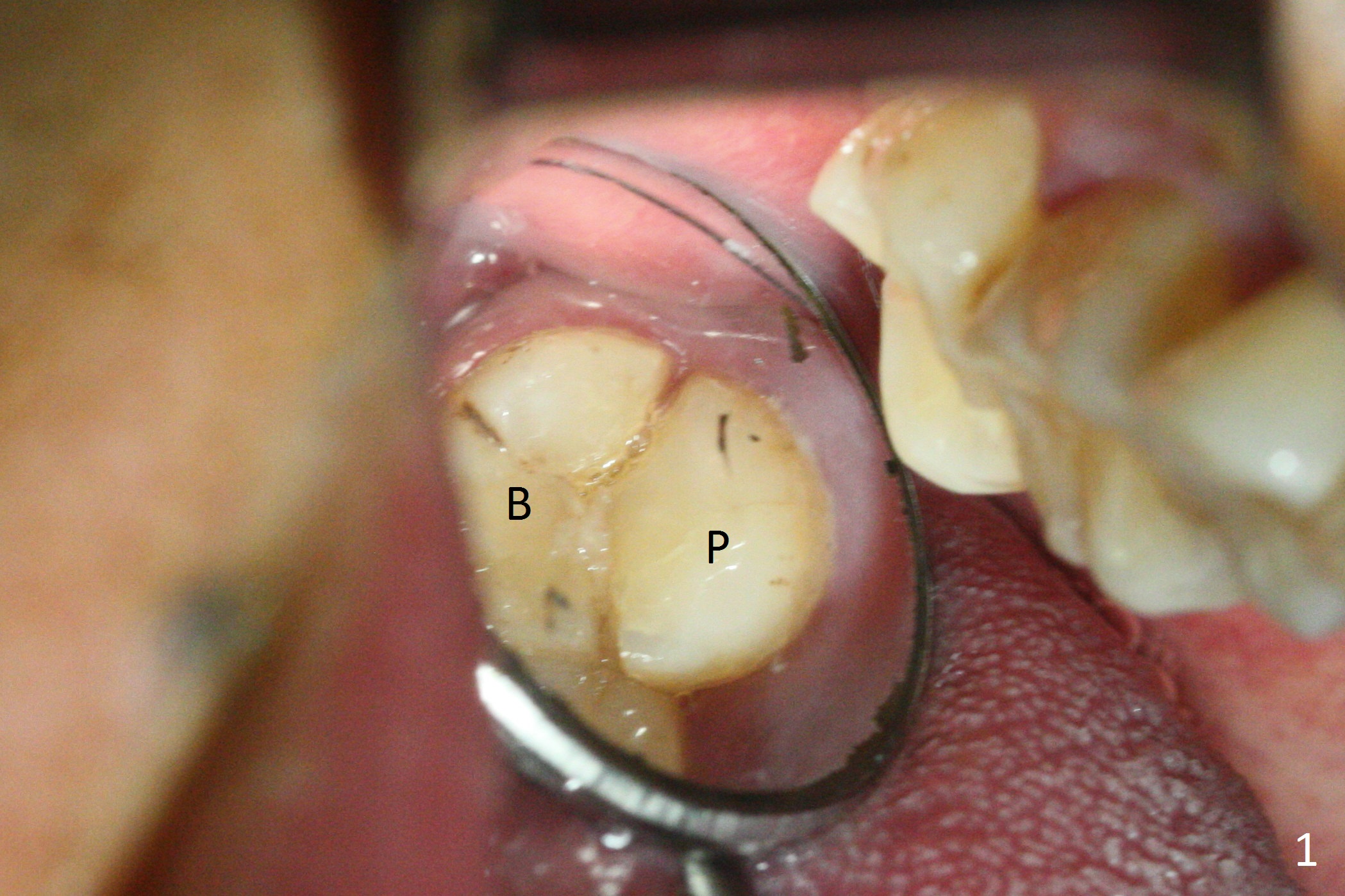
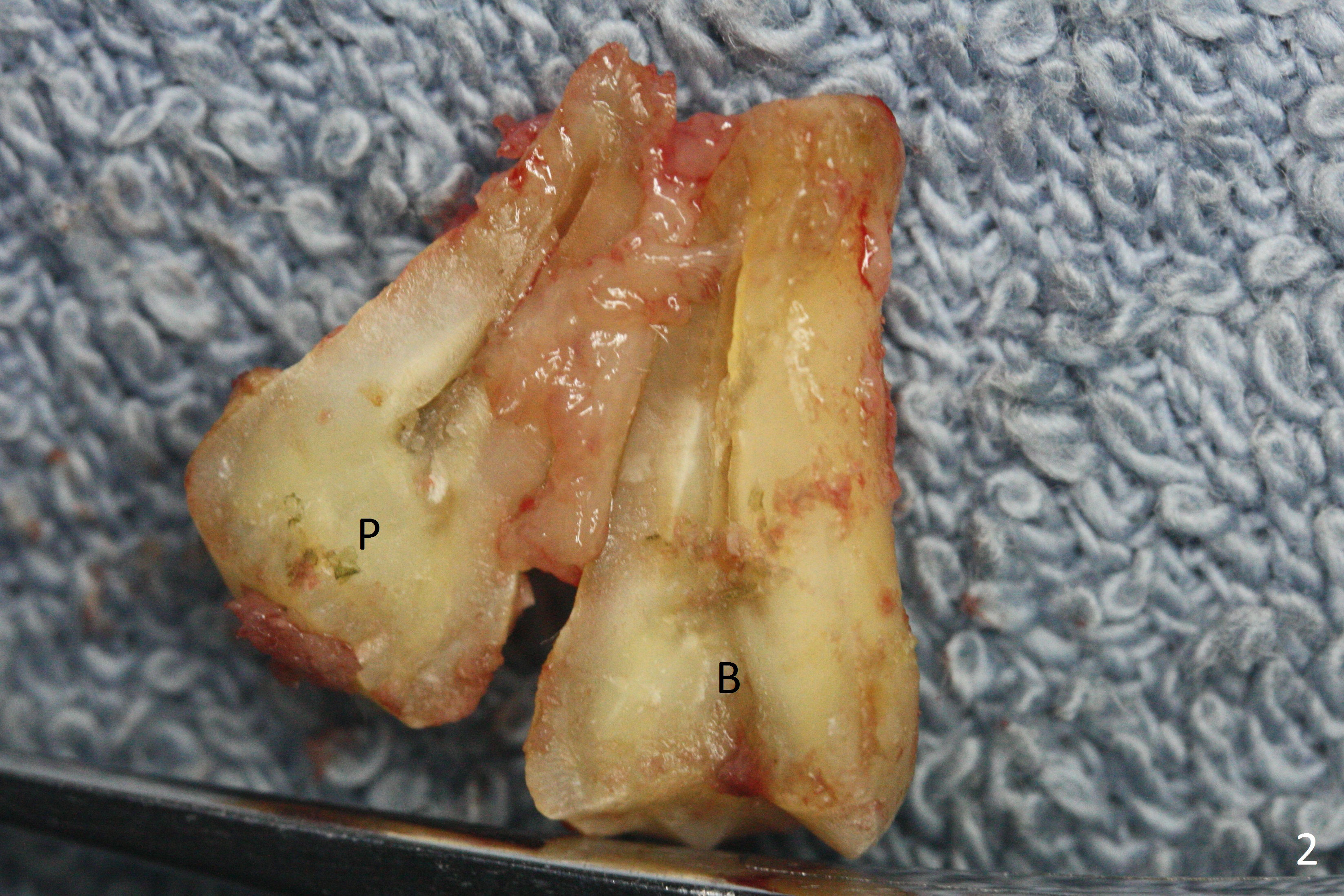
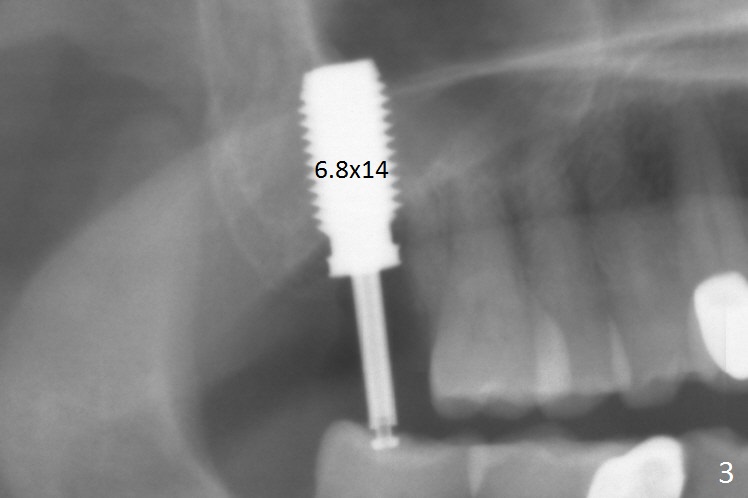
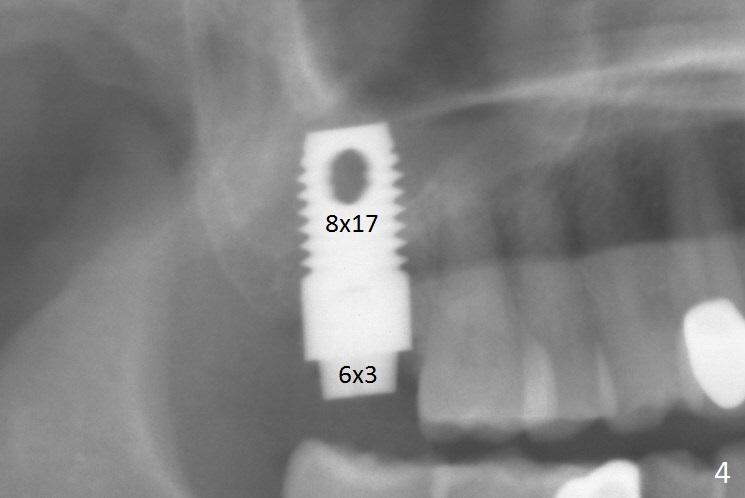
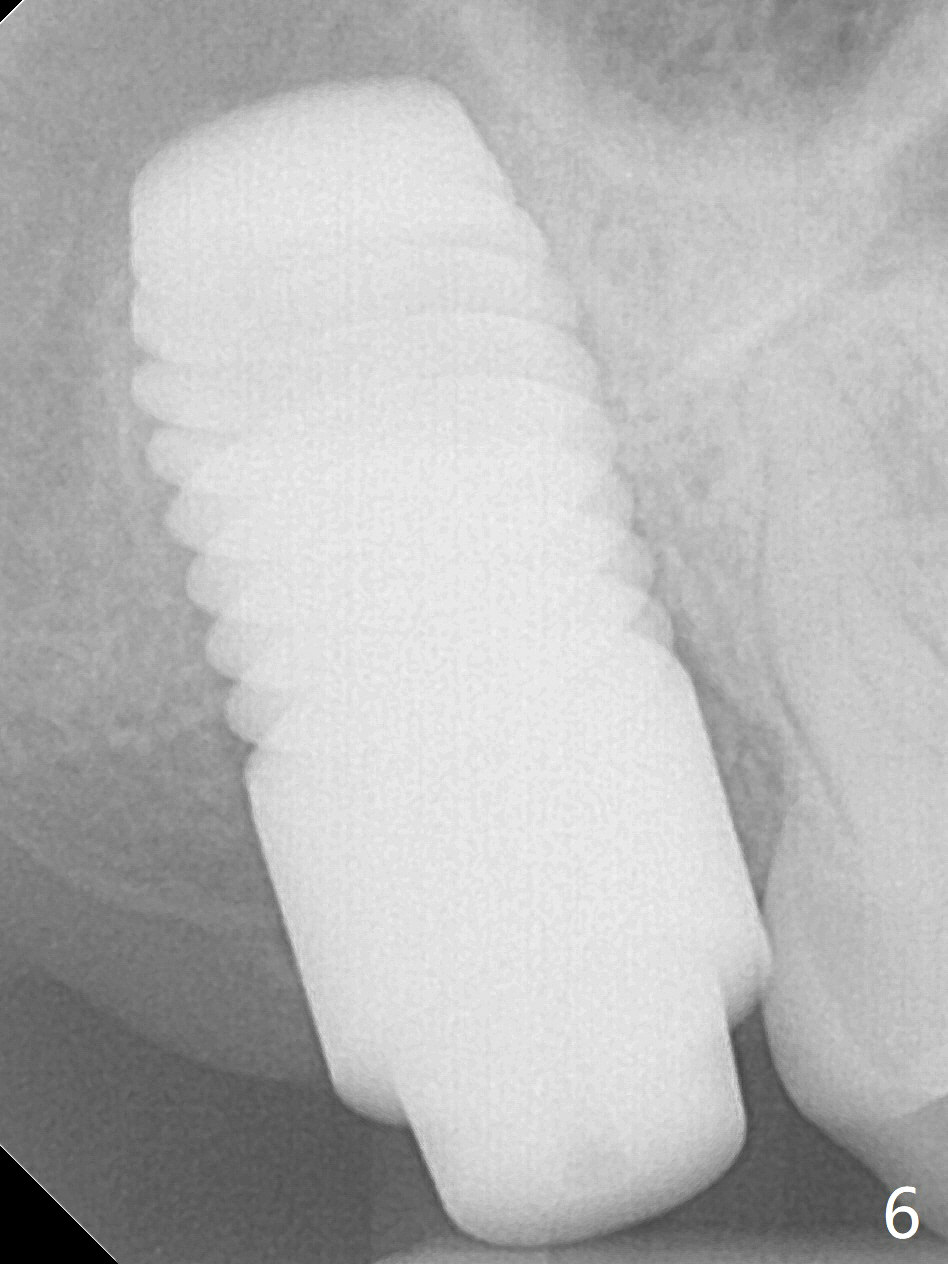
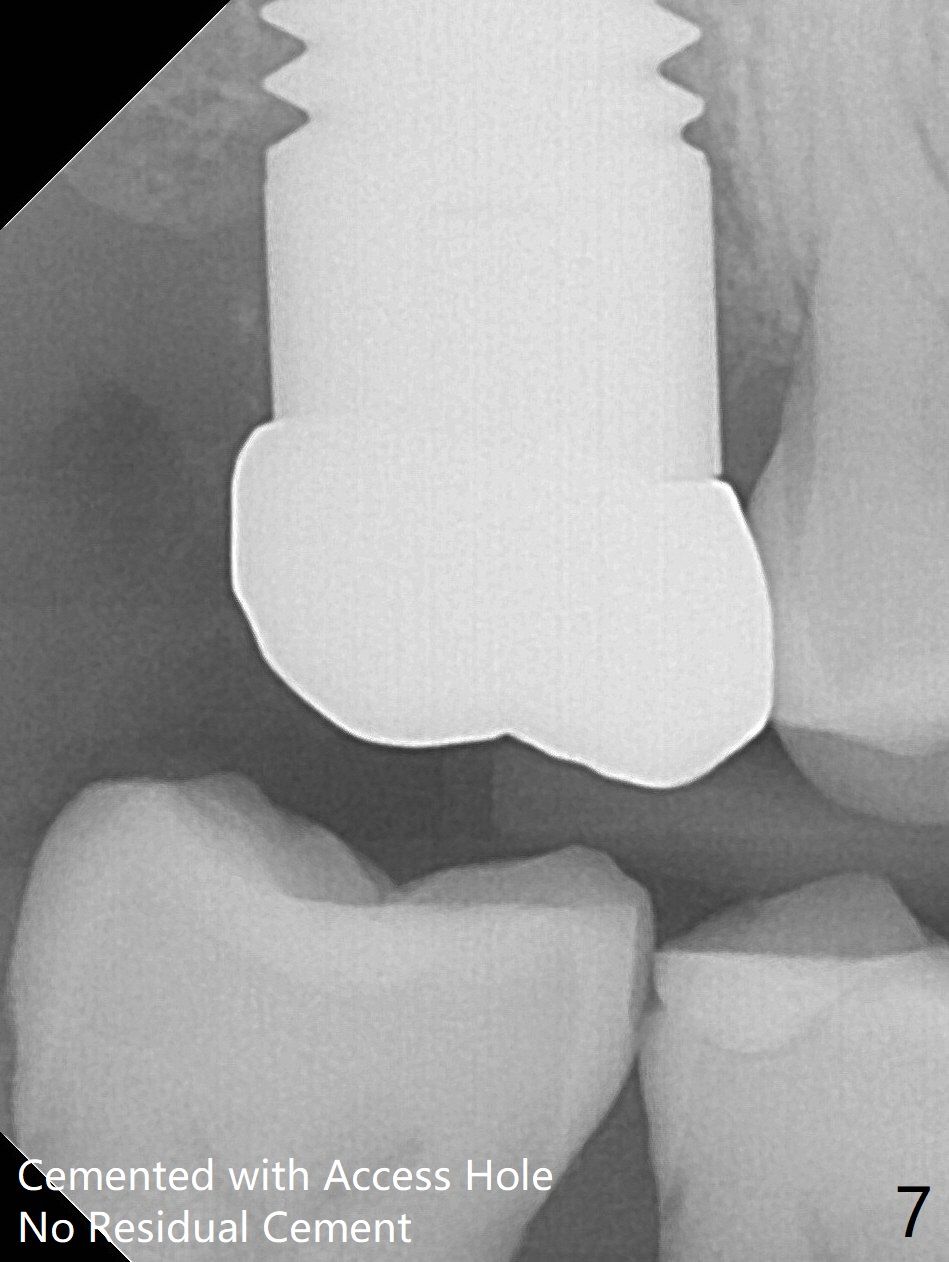
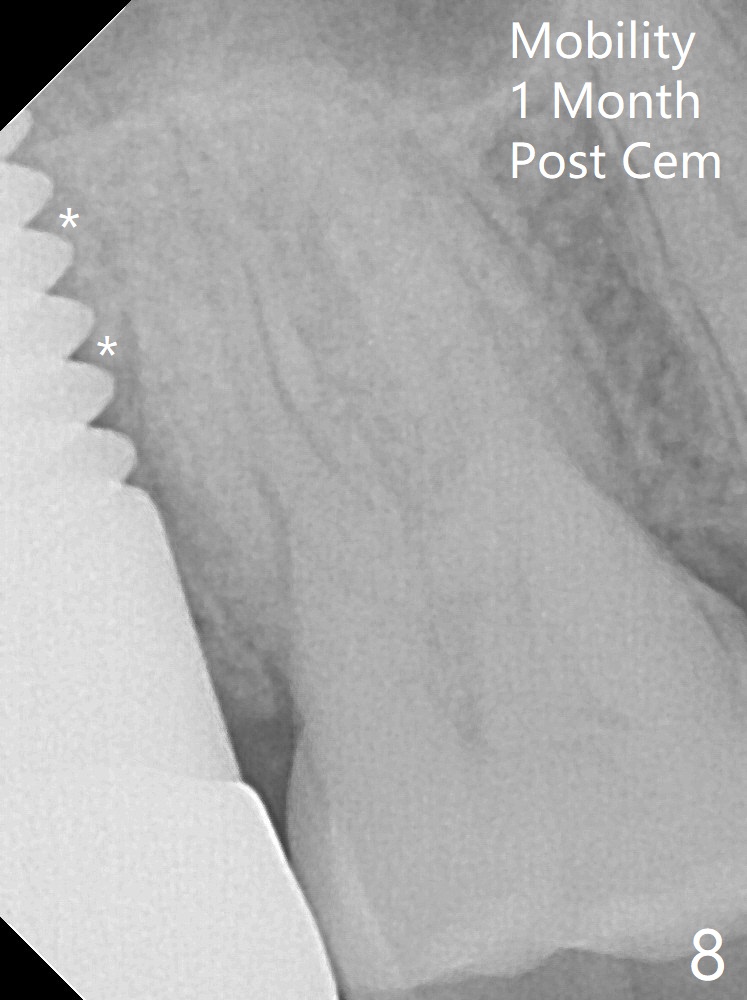
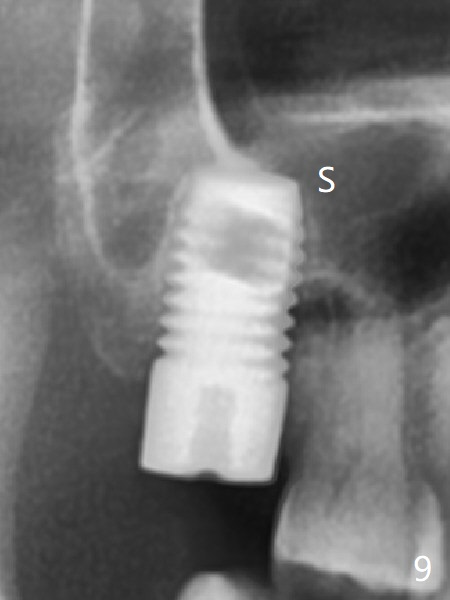
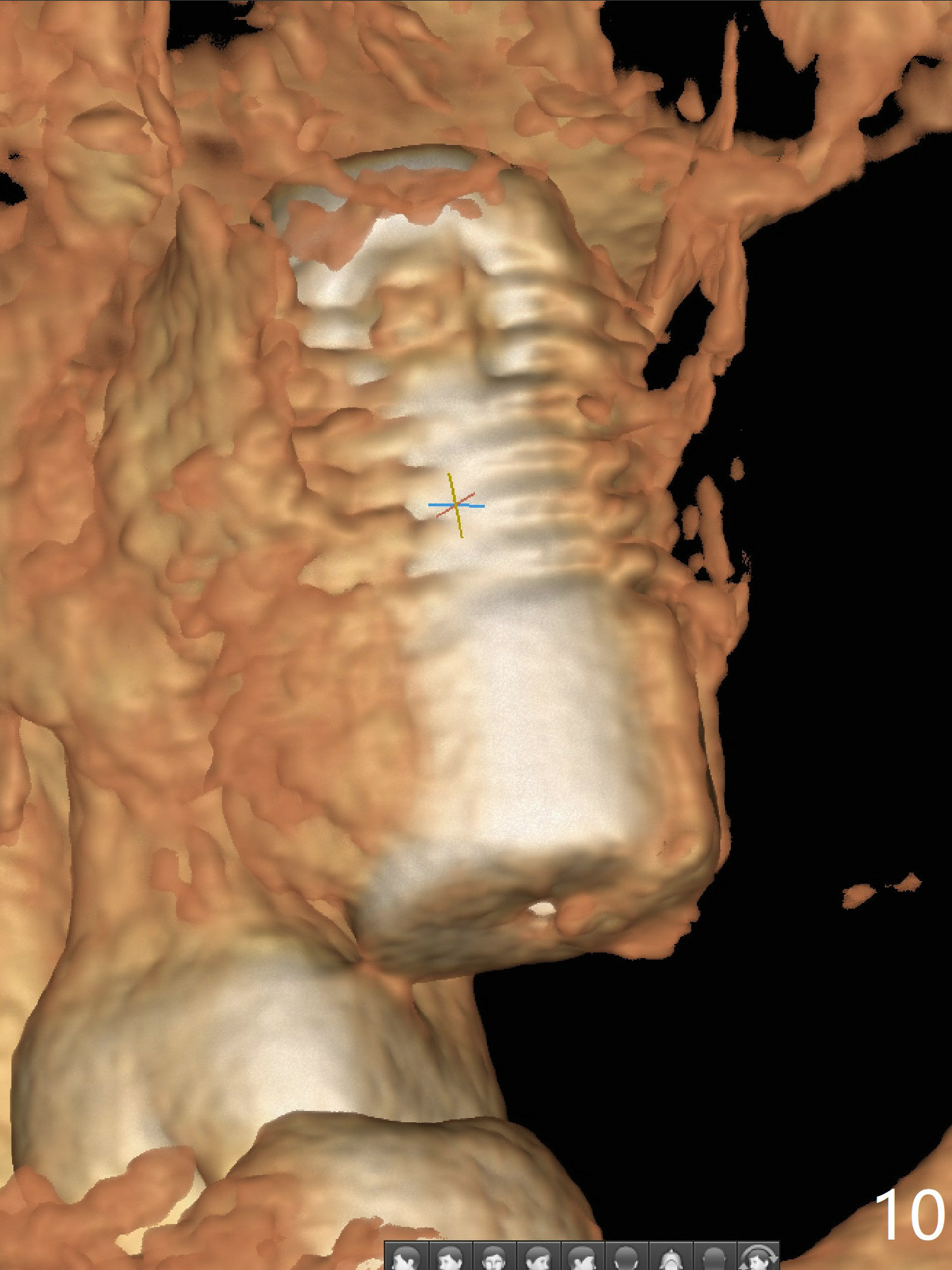
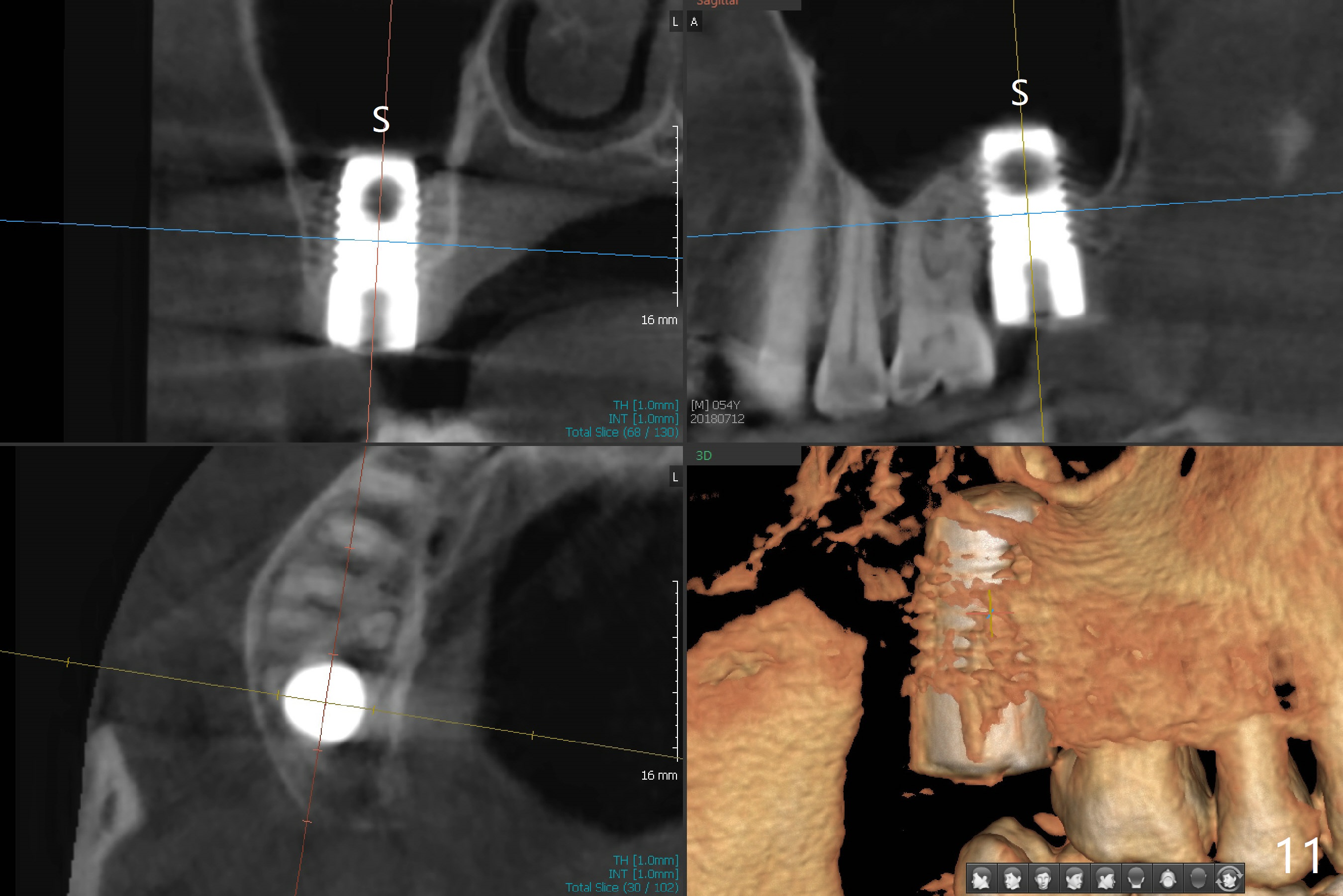
Preop exam shows that the tooth #2 has split into the buccal (Fig.1 B) and palatal (P) halves. When the tooth is extracted (Fig.2), there is a large piece of granulation tissue between these halves. The socket is large with sinus floor having pointed perforation. The latter is enlarged with rounded tapered Tatum osteotomy 2-4 mm, followed by tapered and then rounded taps. A 6.8x14 mm rounded tap has barely enough stability (Fig.3). Following placement of 2 PRF plug and 2 PRF membranes and allograft/Osteogen, a 8x17 mm cylindrical implant is placed with 60 Ncm (implant machine reading), however the implant is unstable (Fig.4). More graft is placed around the implant. With placement of 6x3 mm abutment, an immediate provisional is fabricated to close the socket. There is nasal discharge for a few days postop. PAs taken nearly 6 months postop show no bone loss (Fig.5,6). The definitive crown is cemented with access hole; there is no residual cement (Fig.7 (9 months postop)). The crown is loose 1 month post cementation (last March, Fig.8 with periimplant space (*)). The unipost was not cemented due to gag reflex. He refuses treatment immediately because of the allergy season. When he returns, spray a topical to his throat. Following crown removal, implant is found to have mobility. Panoramic X-ray (Fig.9) and CT (Fig.10,11) show fibrointegration (space) and implant intrusion into the sinus (S) without bone formation. After implant removal, the sinus floor and membrane are found to have been perforated. Osteogen plug is placed, followed by Vanilla/Osteogen (Fig.12 *) and Osteogen plug. It appears that an immediate implant is contraindicated when there is severe infection (Fig.2) with sinus floor perforation. In this case, the bone density at the upper 2nd molar is low (Fig.10 distopalatal view of 3-D image). Bone expansion and condensation is needed for implantation. Progressive loading is also necessity prior to impression.
Return to Upper Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), IBS, #7,10, 19 Xin Wei, DDS, PhD, MS 1st edition 05/02/2017, last revision 11/03/2018