,%20bone%20graft%20distal.jpg)

,%2015%20M%20bone%20graft.jpg)
 |
 |
 |
||
,%20bone%20graft%20distal.jpg) |
 |
 |
,%2015%20M%20bone%20graft.jpg) |
|
 |
 |
 |
 |
 |
Bone Engaging Power of IBS Implant Fins for Sinus Lift
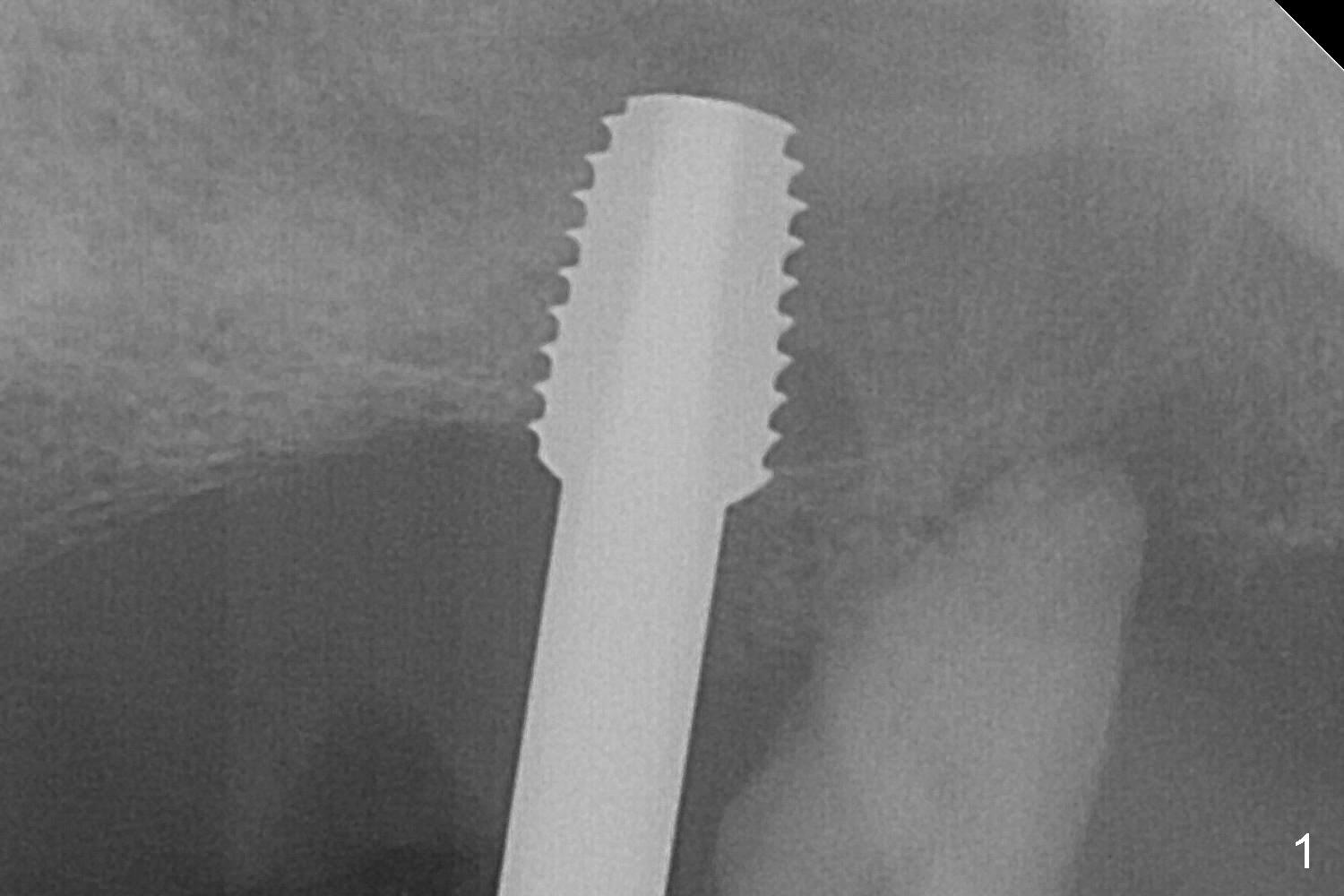
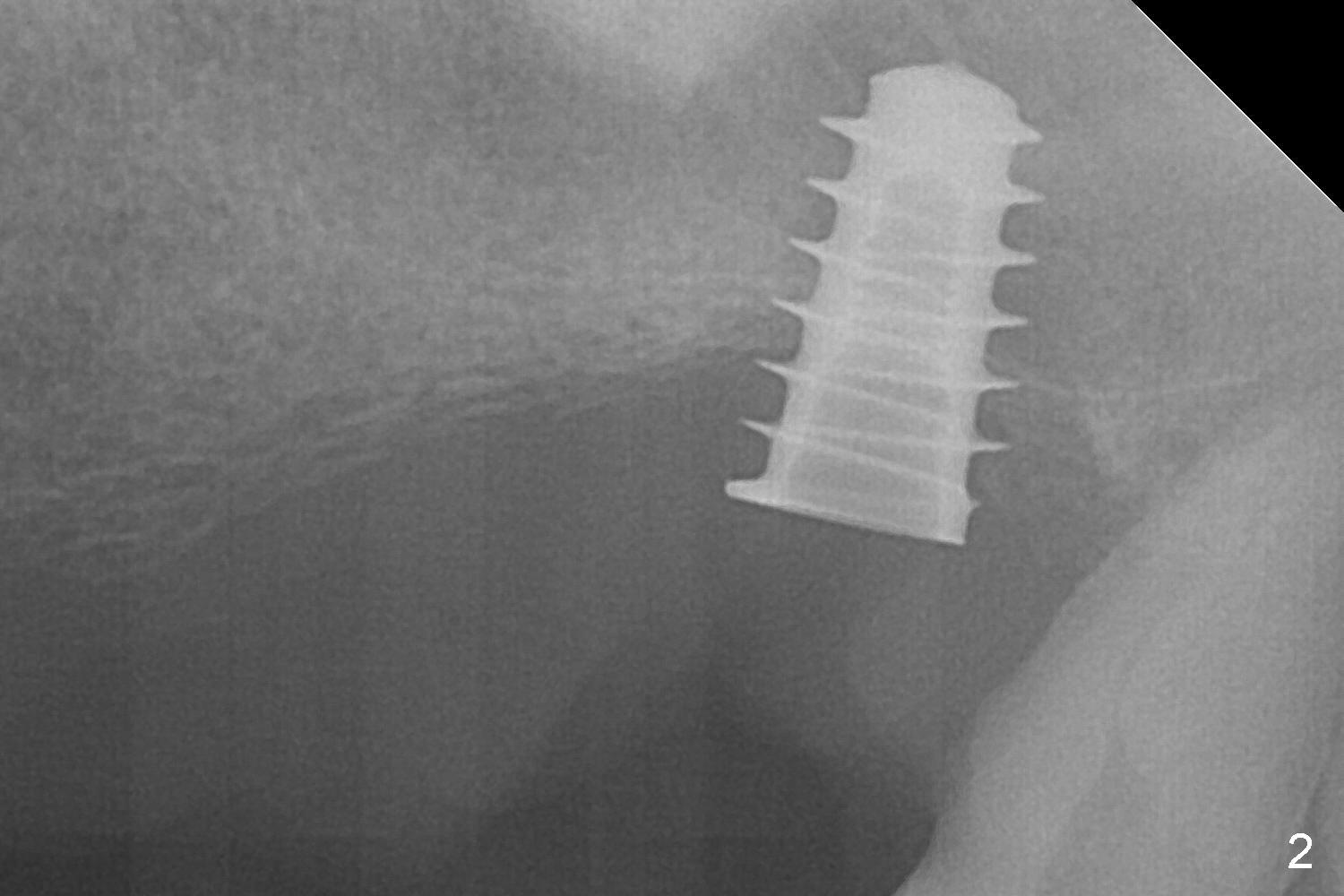
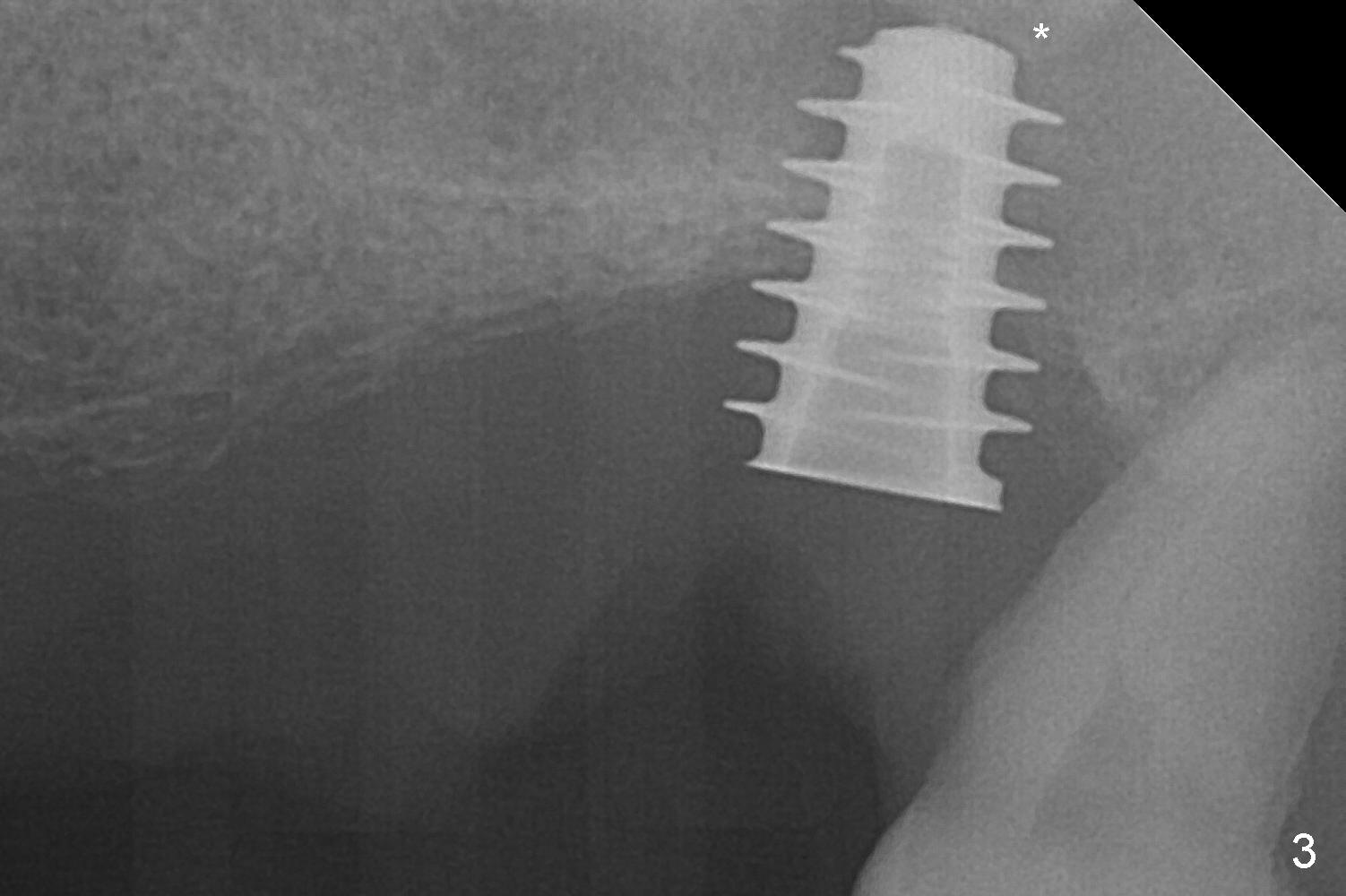
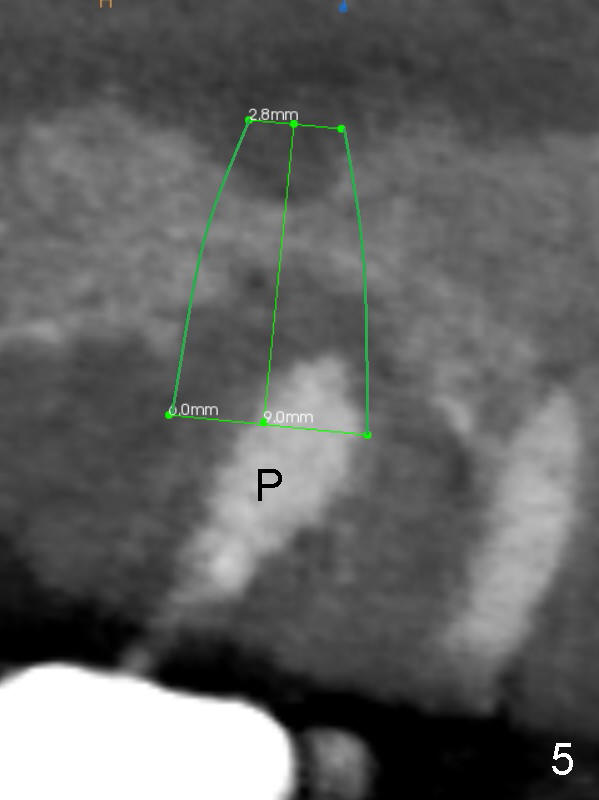
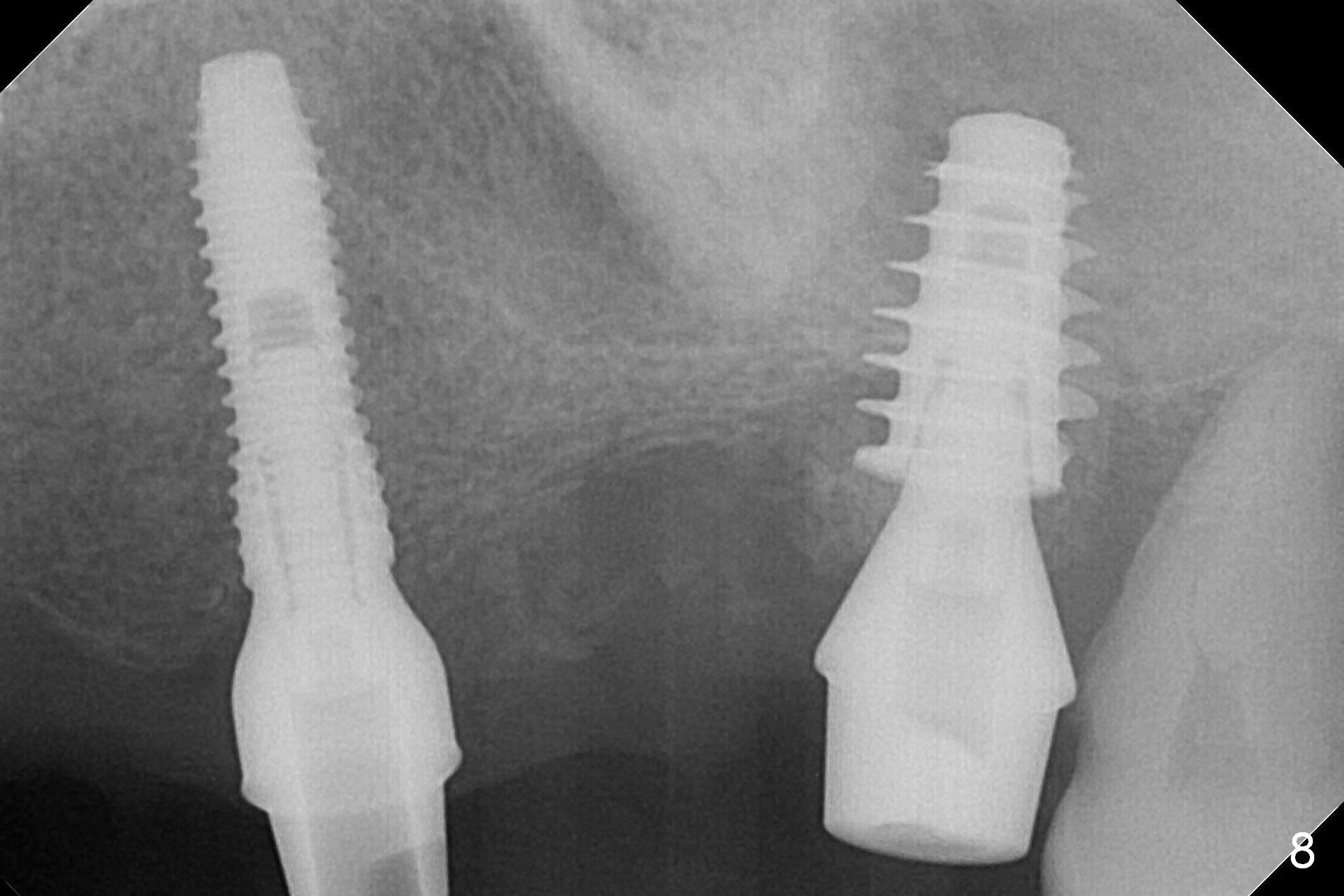
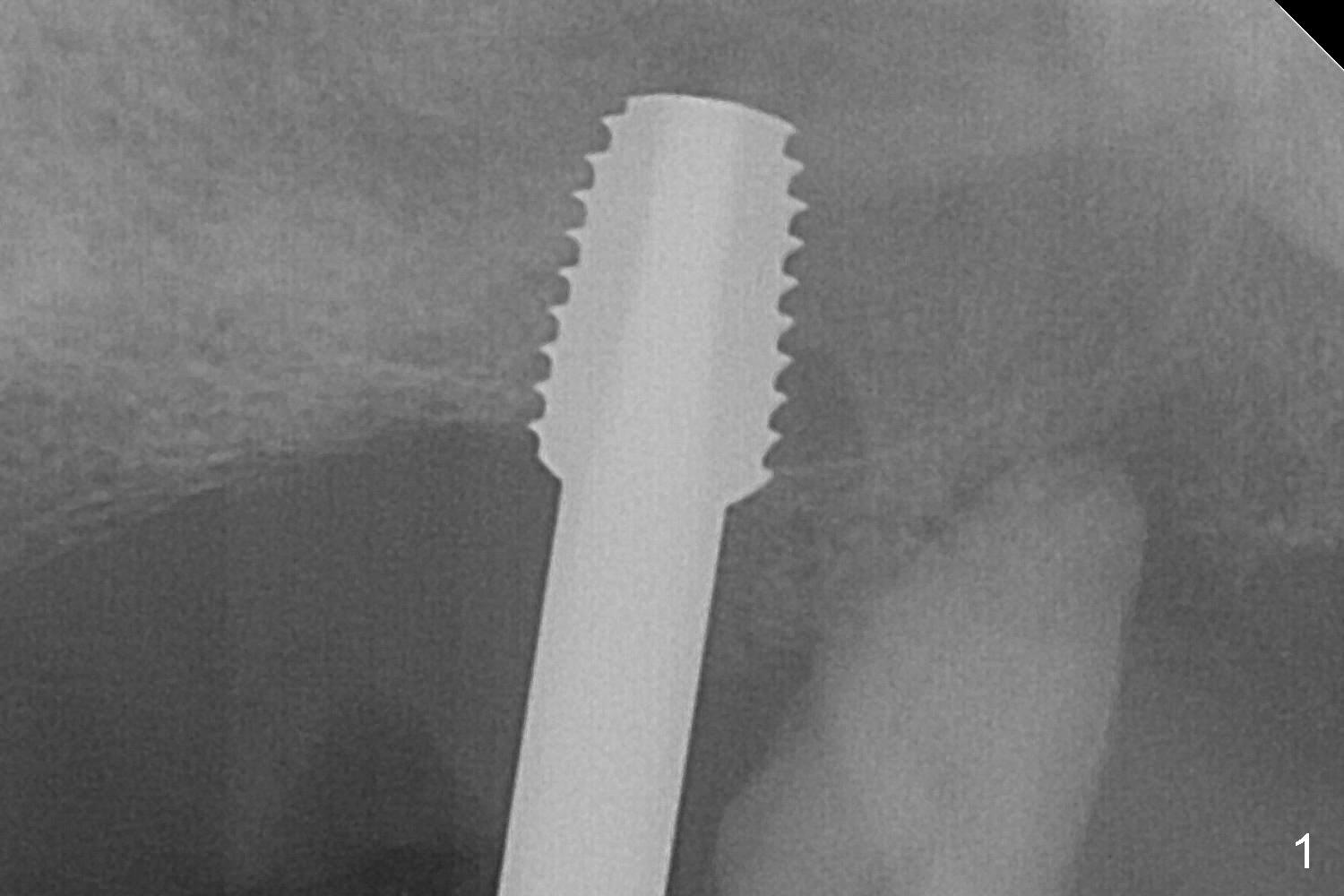
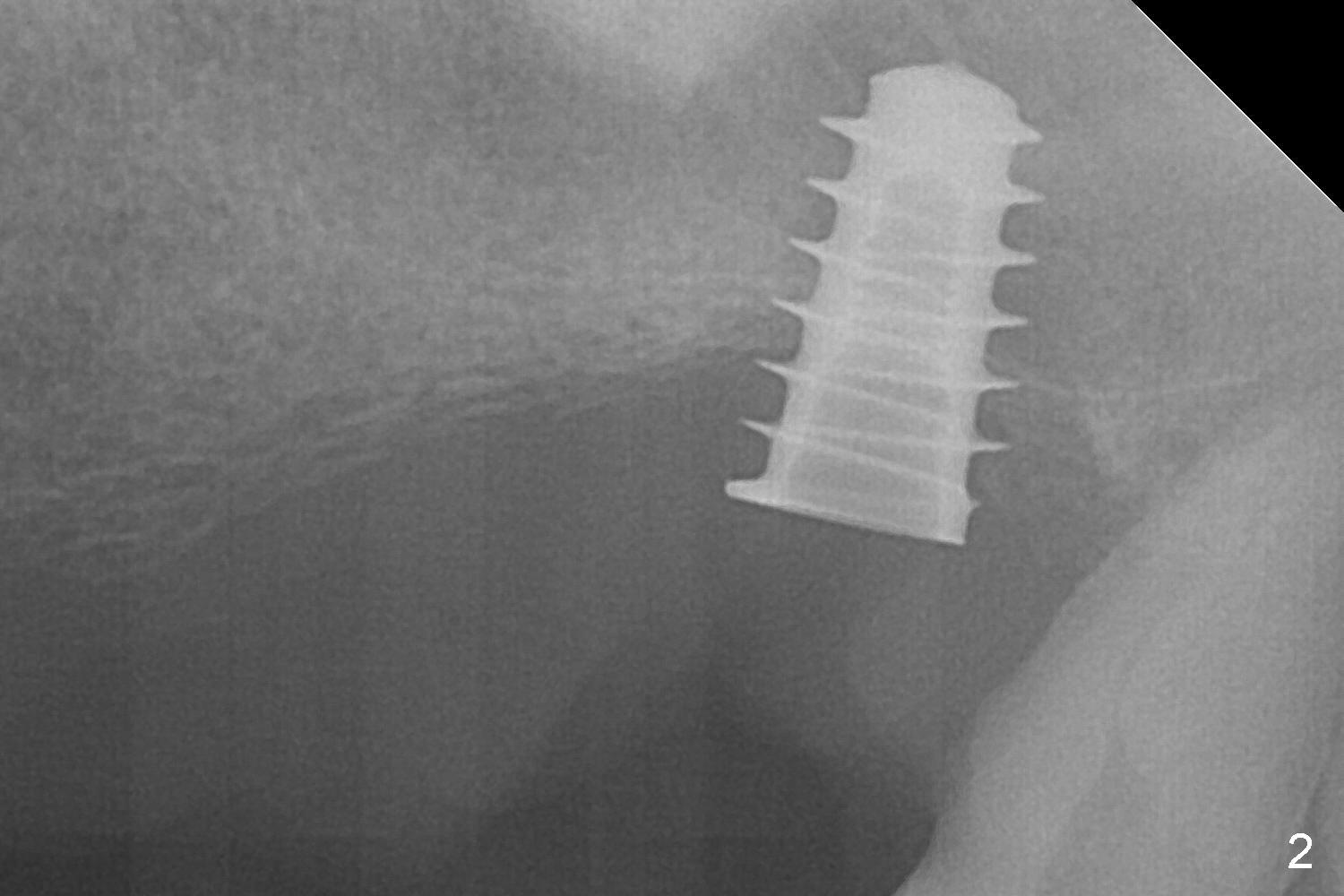
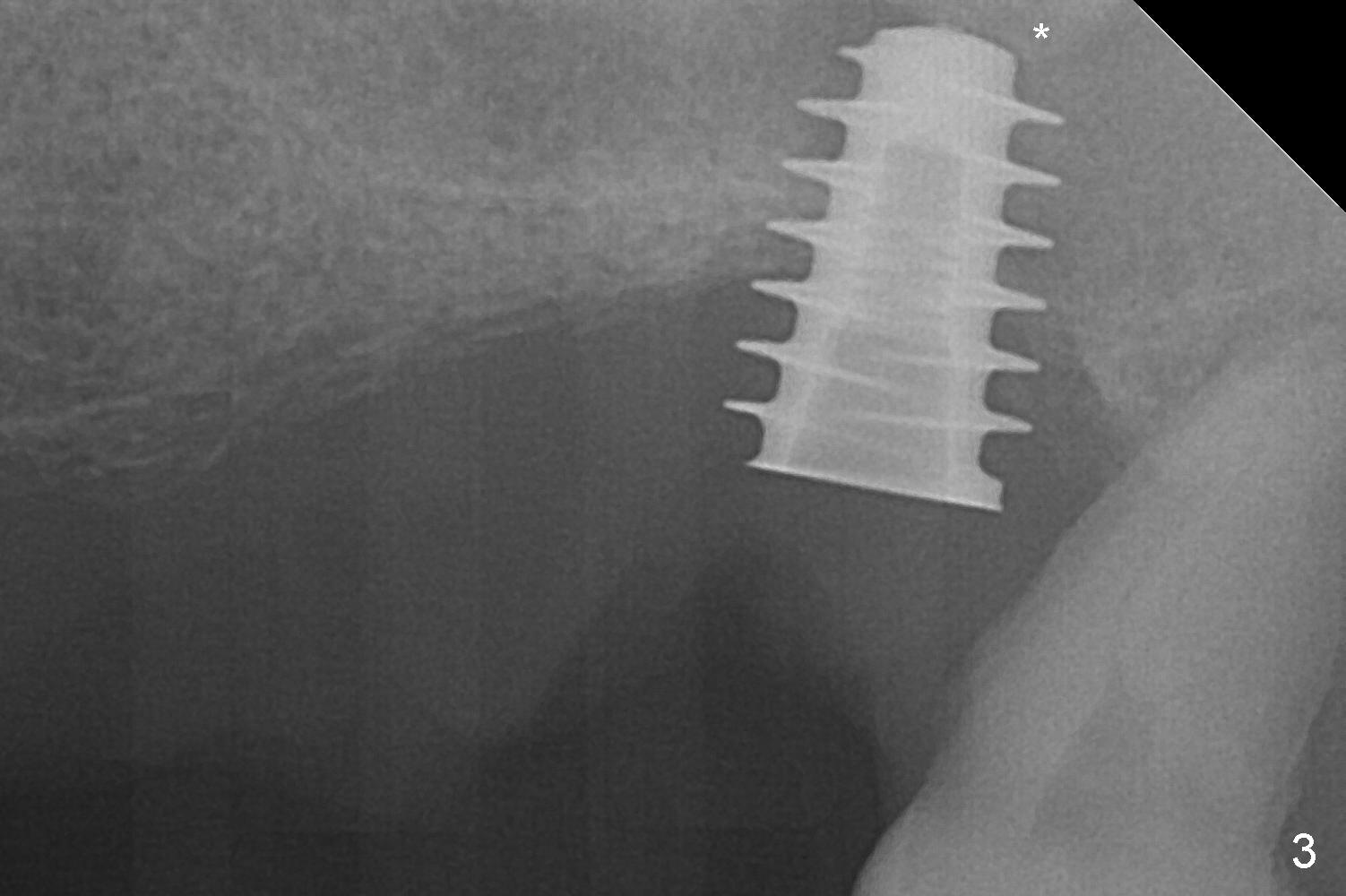
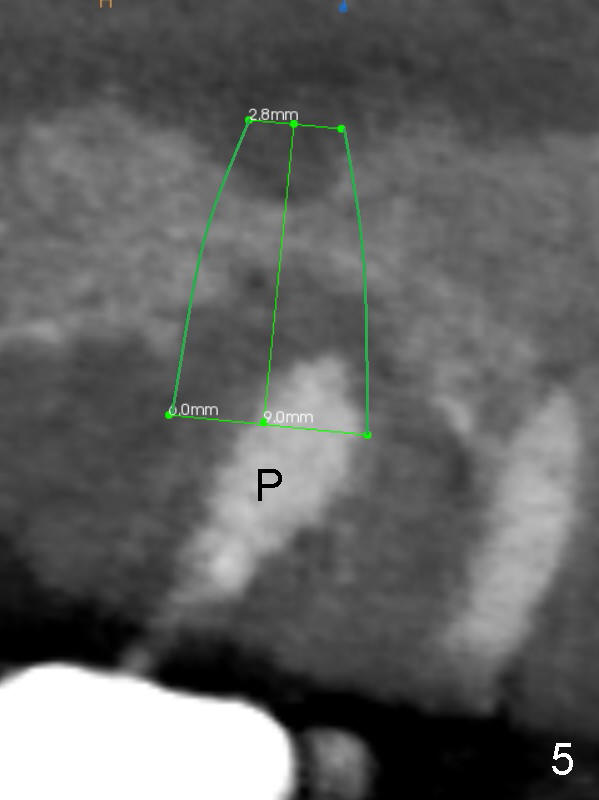
The posterior abutment of the 5-unit FPD, #15 is loose with the buccal roots extruded outside the sockets. The palatal socket is the appropriate site of immediate implant with the presence of the buccomesio-palatal walls, although short. The thinnest portion of the palatal socket is 1.6 mm (Fig.6 CBCT coronal section through the palatal root (P)). Magic Sinus Lifter cannot break through the sinus floor. UF drills are used to create osteotomy and sinus lift until 4.3 mm. A 5 mm tap drill is inserted without stability (Fig.1). A 5.5x9 mm IBS dummy implant achieves insertion torque of 10 Ncm, although it looks smaller (Fig.2) than the tap in Fig.1. After placement of PRF membrane and bone graft (allograft, autogenous bone and Osteogen, Fig.3 *), a 6x9 mm IBS implant is placed with insertion torque of 30 Ncm. It appears that the fins of the implant slice into the bone at high magnification for engagement. Following further placement of the implant, bone graft is packed into the distal portion of the socket (Fig.4 <). The thin fins extends into mesial and distal thicker bone (Fig.5 (CBCT sagittal view) *).
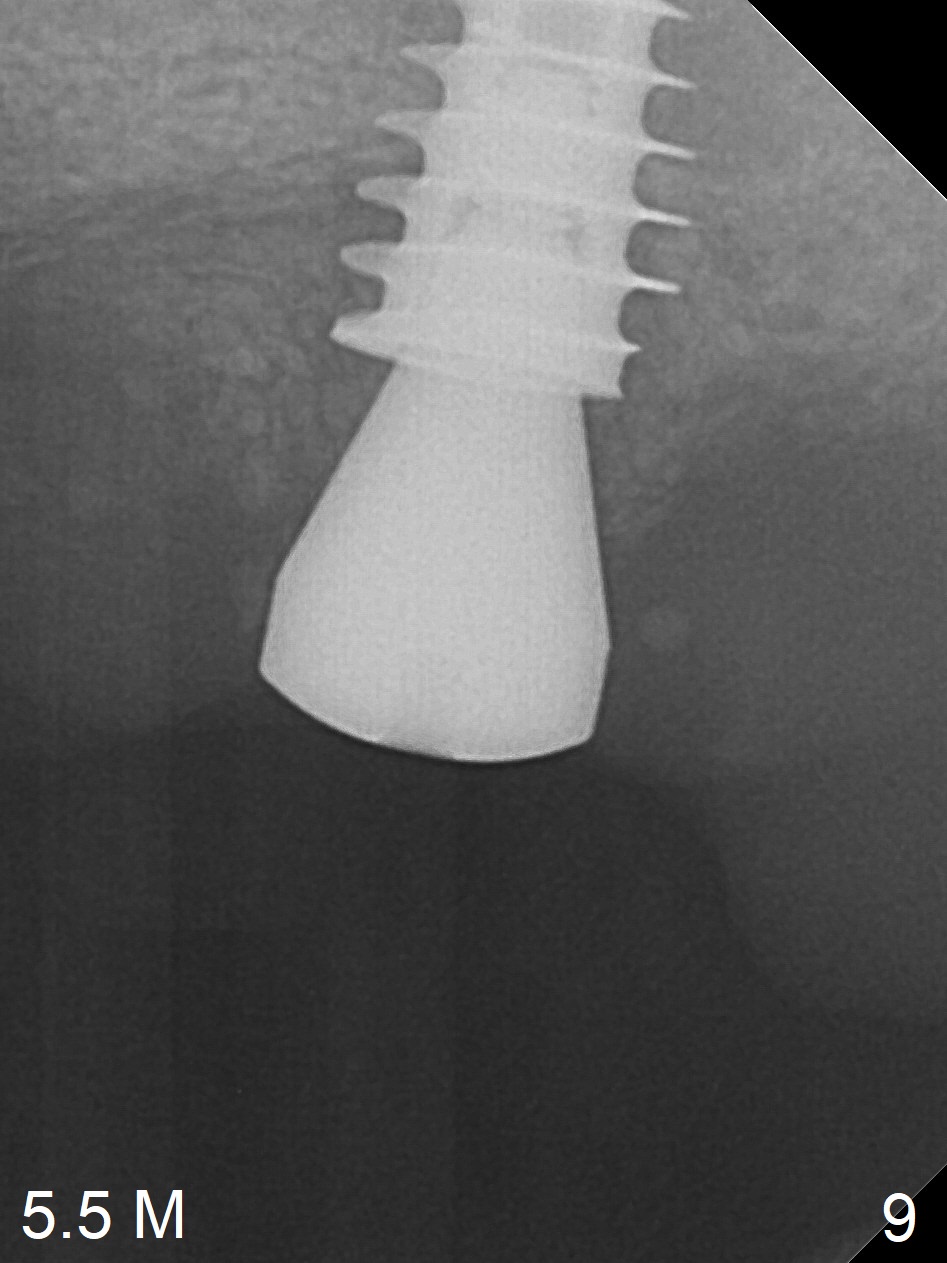
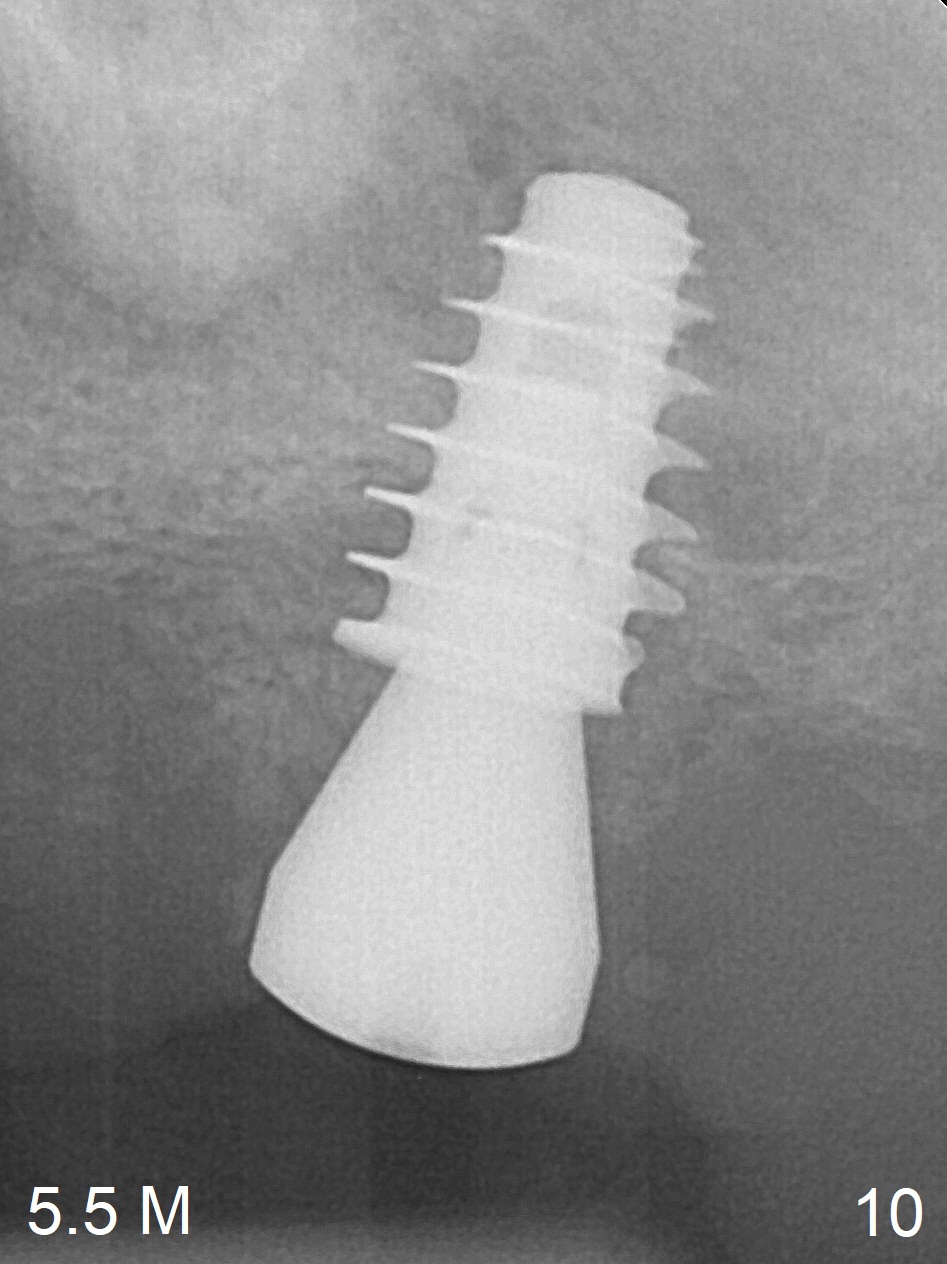
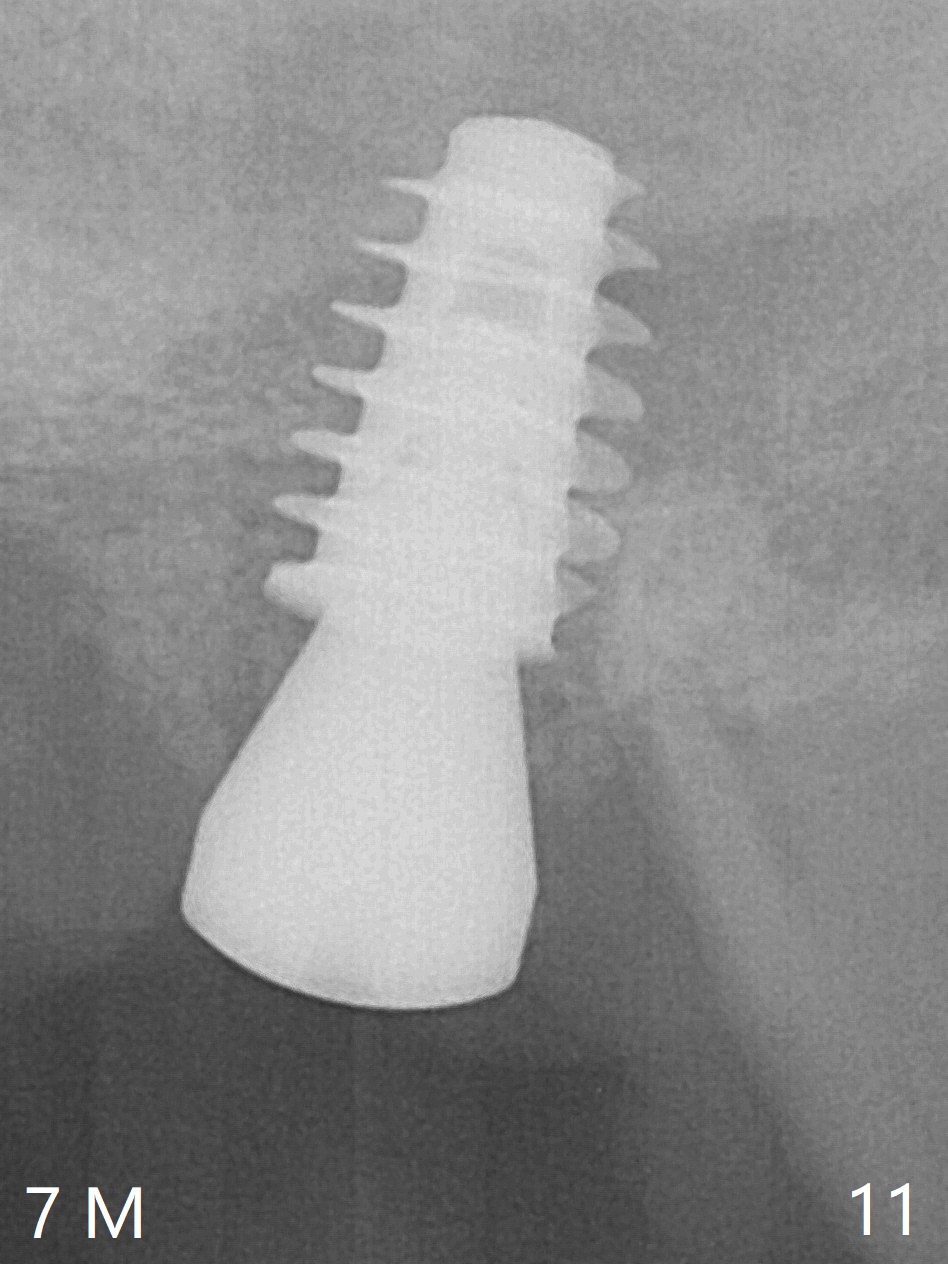
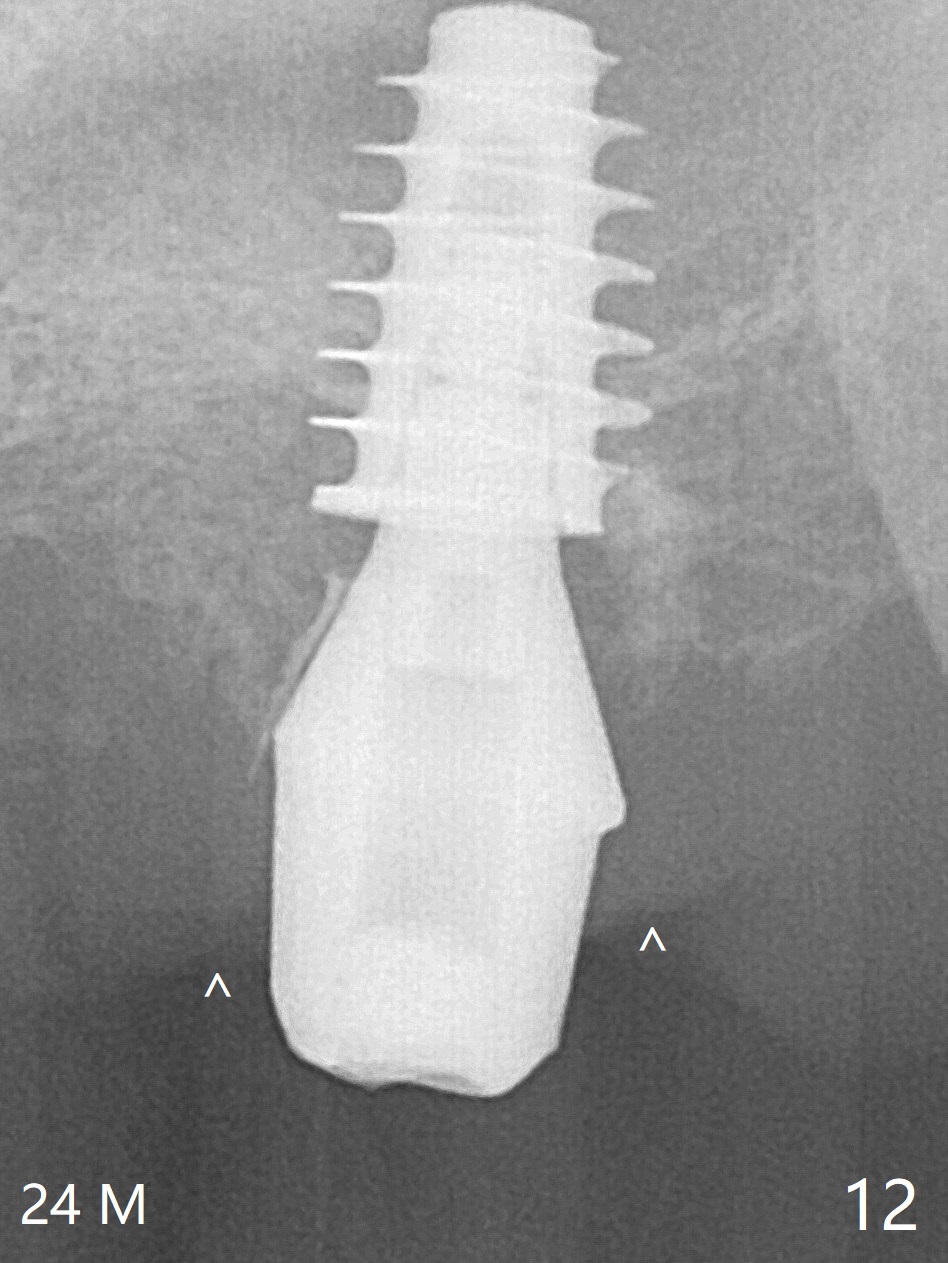
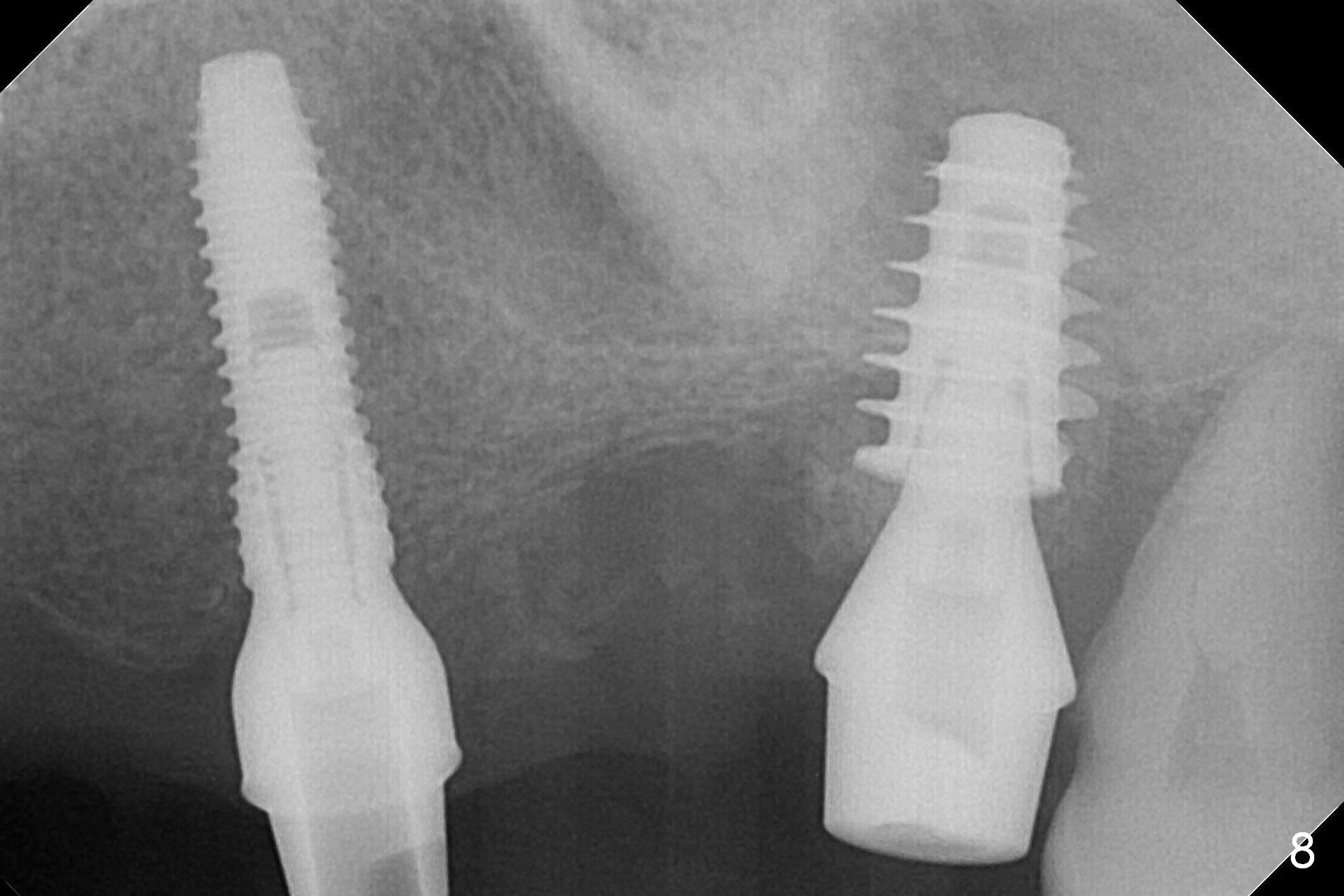
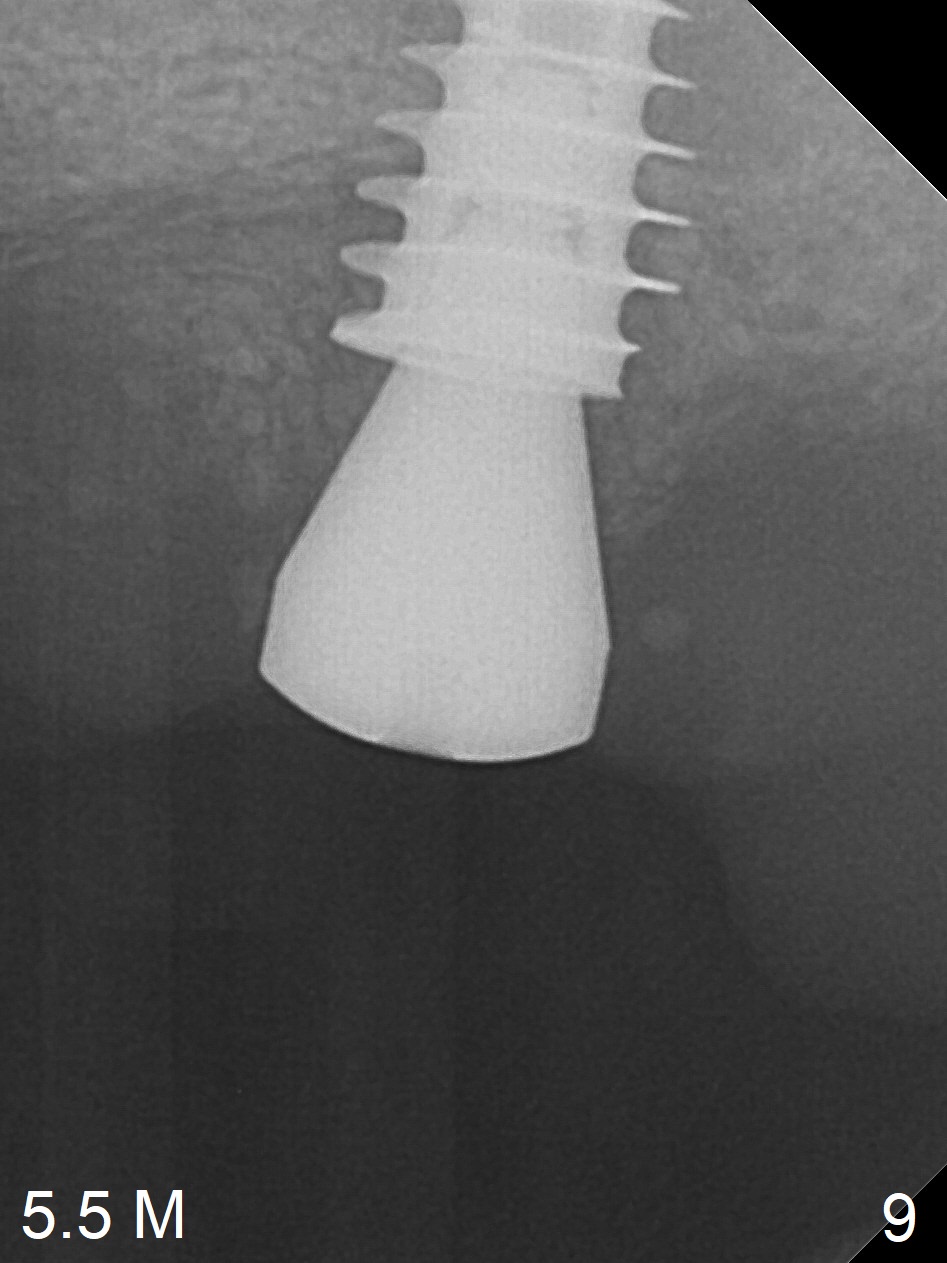
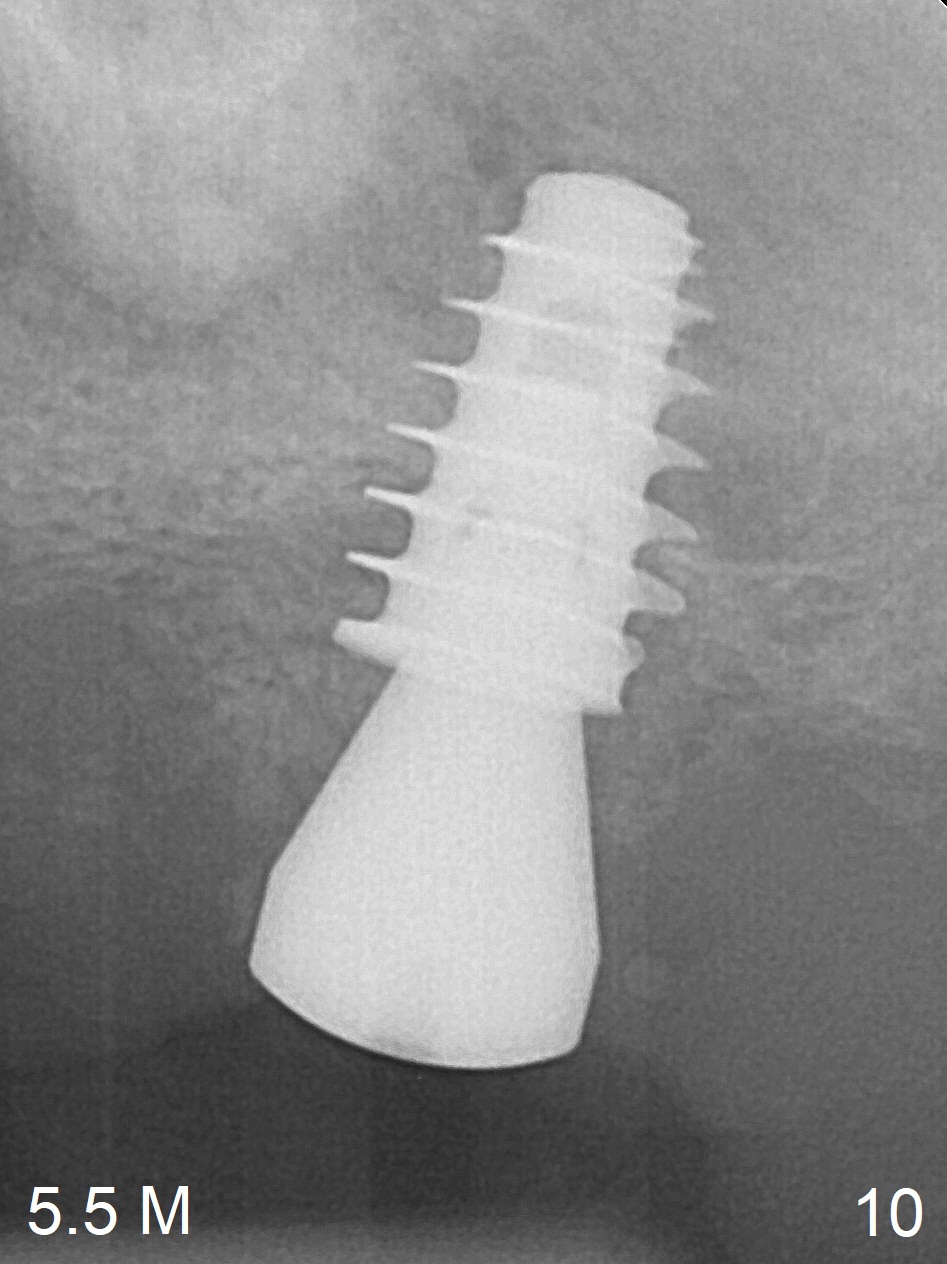
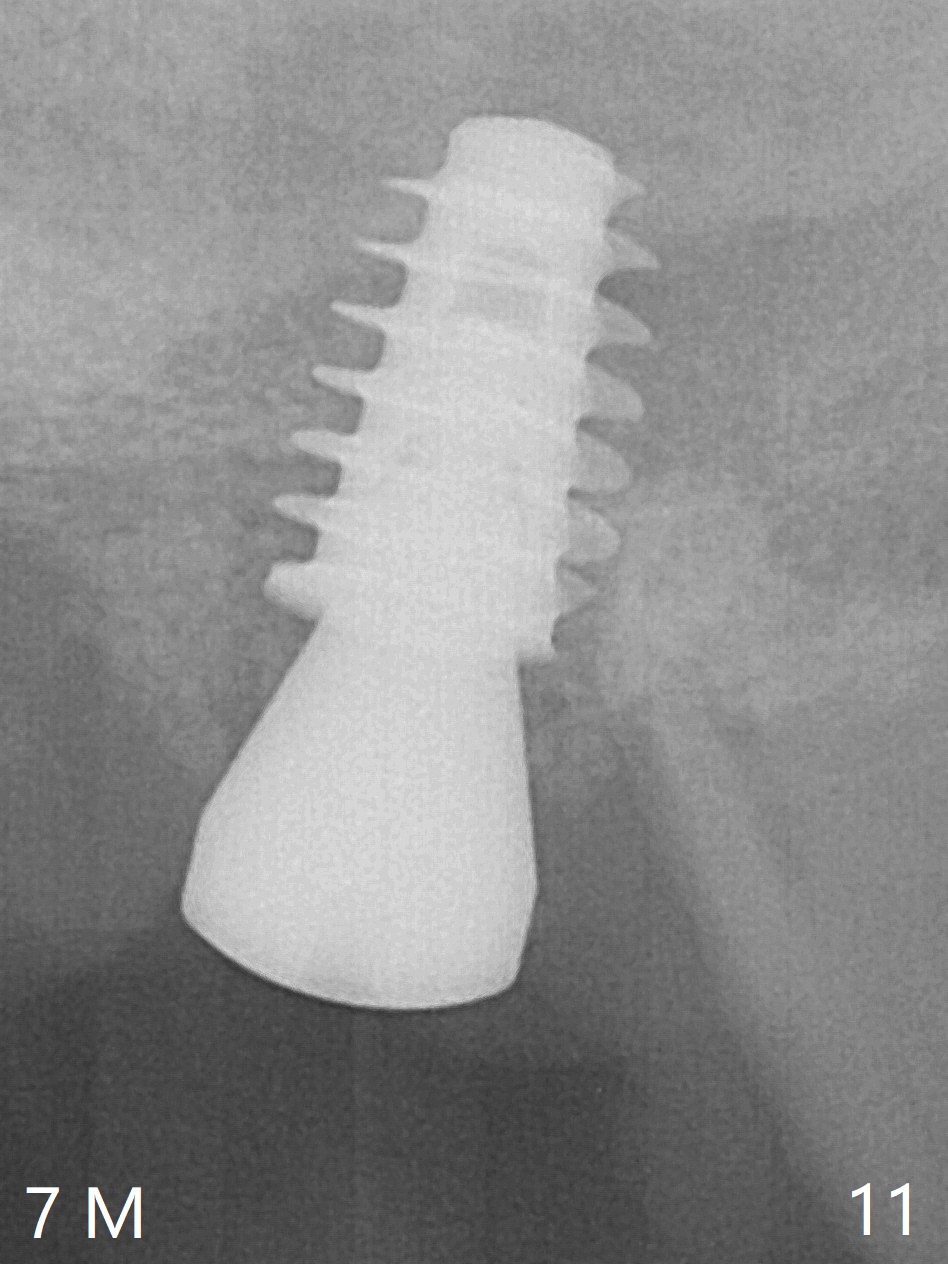
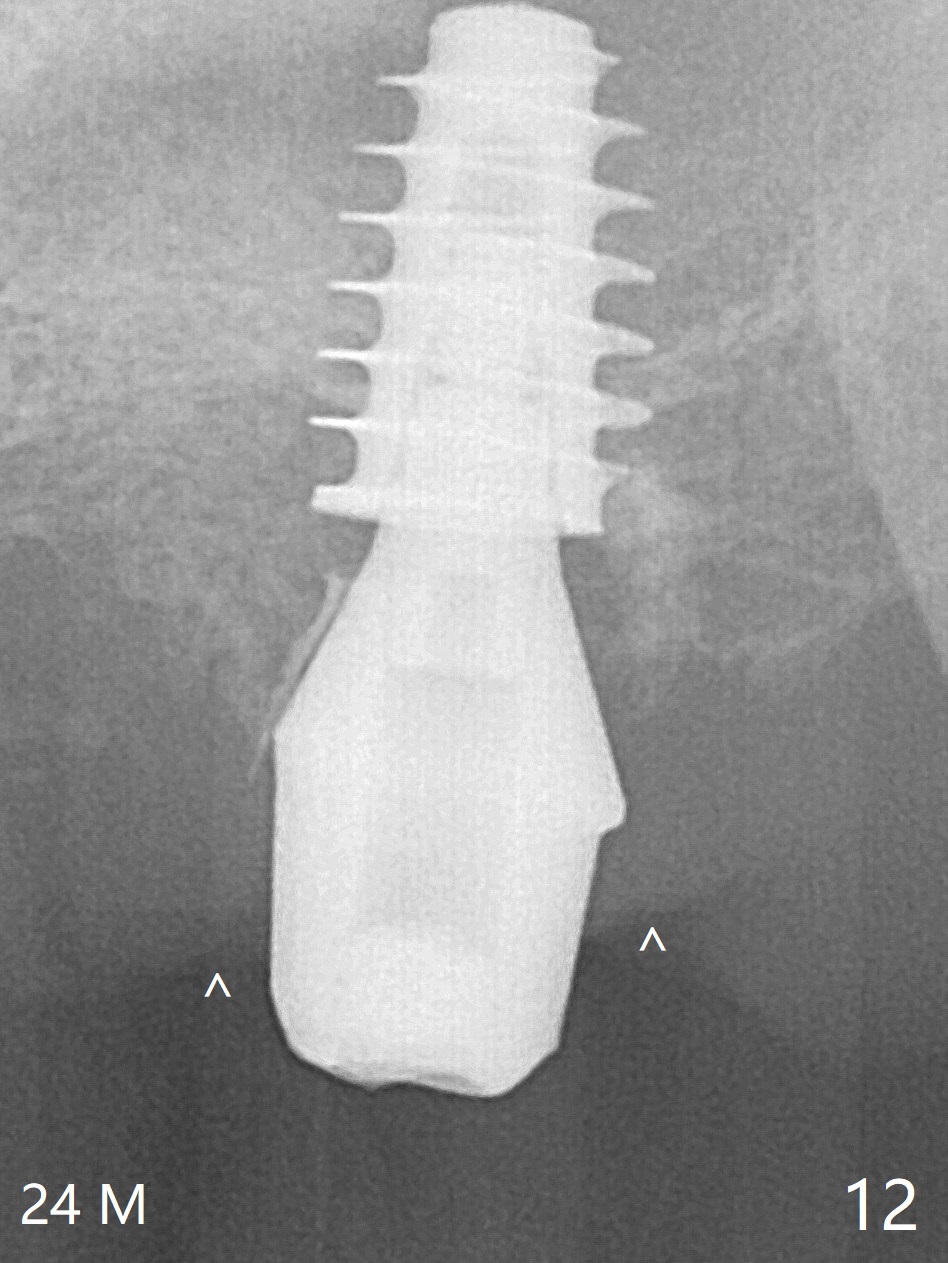
One month later, bone graft is placed mesiopalatal to the implant at #15 (Fig.7 *,8) while a 3.8x13 mm implant is placed at #13 following bone expansion (using Magic Split and Magic Expander 3.0 mm (abutment 5.5x4(5) mm). Another month later, the tooth #16 is extracted to create space for #15 restoration. Two weeks later the abutment at #15 is found to be unstable (2.5 months postop). Local oral hygiene is poor. The abutment is removed and a 6x4 mm healing abutment is placed with mild tenderness. It appears that the limited bone height is associated with low stability with CMC. Three months later (5.5 months postop), the implant seems to be stable (Fig.9,10). The implant remains stable clinically 7 months postop (Fig.11). The bone graft appears to mature and covers the abutment with provisional 24 months postop, the bony changes is related to the thick gingiva (Fig.12 ^).
Return to Full Mouth Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table) Next #2,3,5 Course 2 3 4 CMC Xin Wei, DDS, PhD, MS 1st edition 02/24/2017, last revision 03/01/2019