
%20bone%20graft%20buccally.jpg)



.jpg)


%20abutment,%20temp.jpg)



 |
 |
 |
 |
 |
%20bone%20graft%20buccally.jpg) |
 |
|
 |
 |
 |
|
 |
.jpg) |
 |
|
 |
%20abutment,%20temp.jpg) |
 |
|
 |
 |
 |
|
 |
 |
||
PRF Membranes
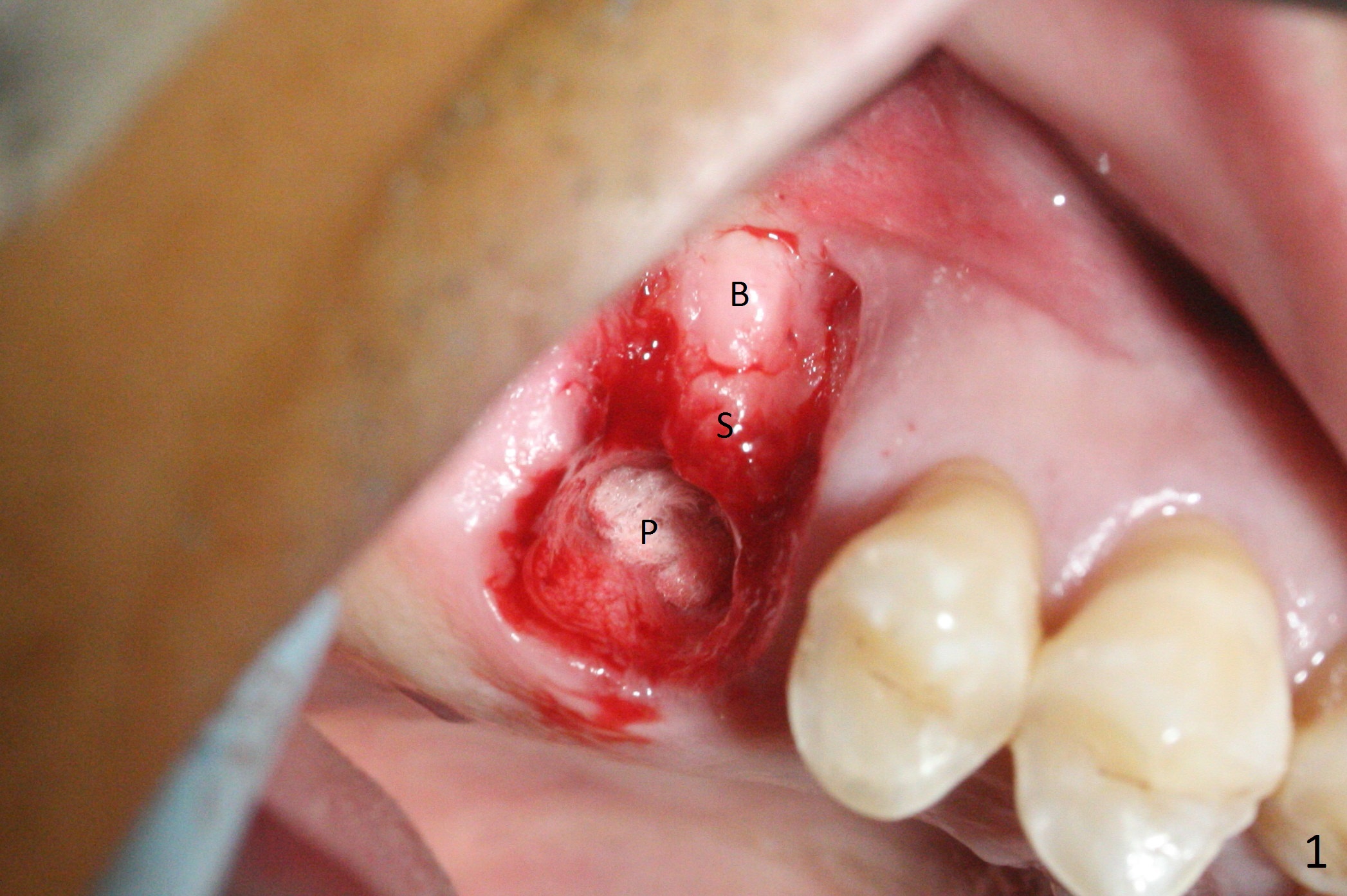
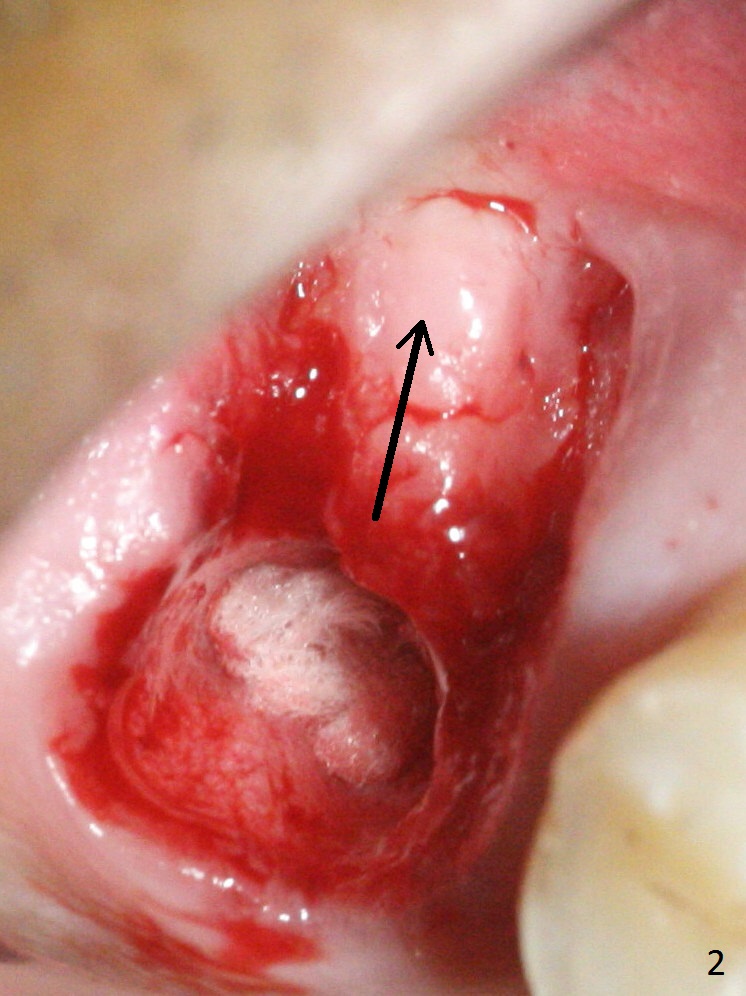
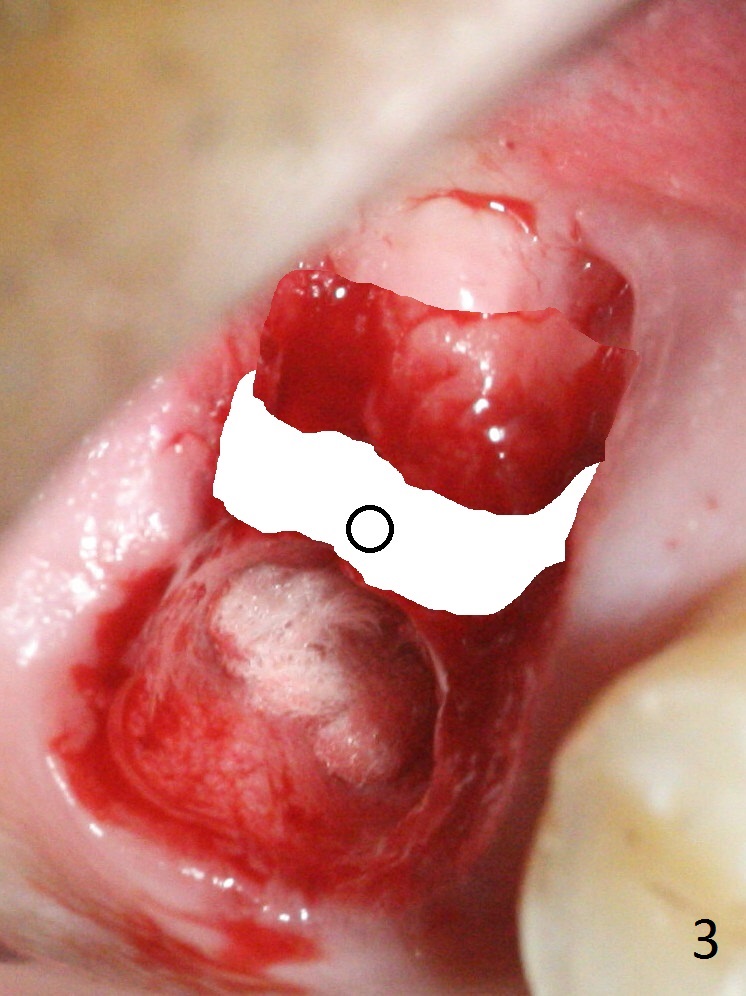
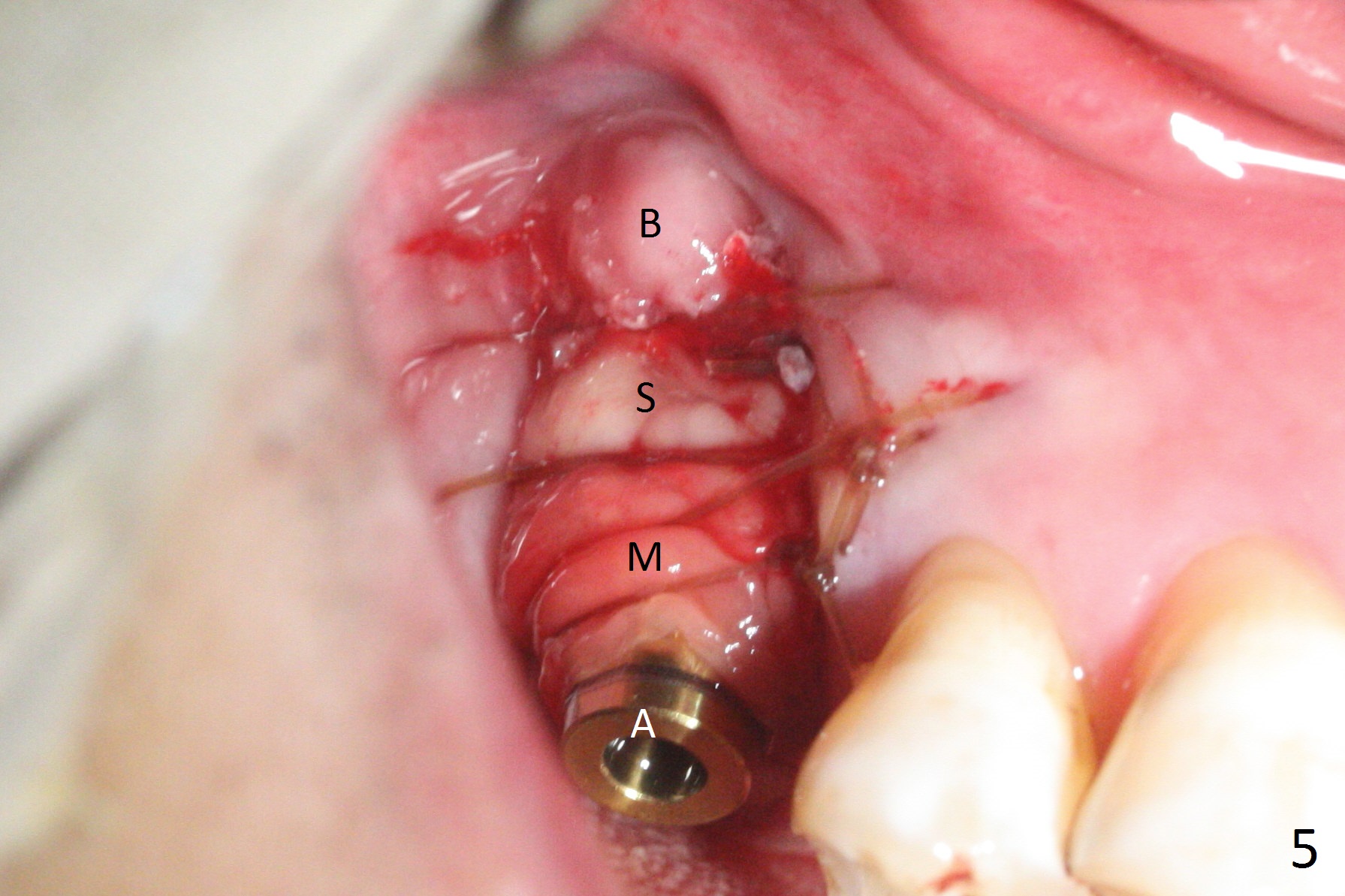
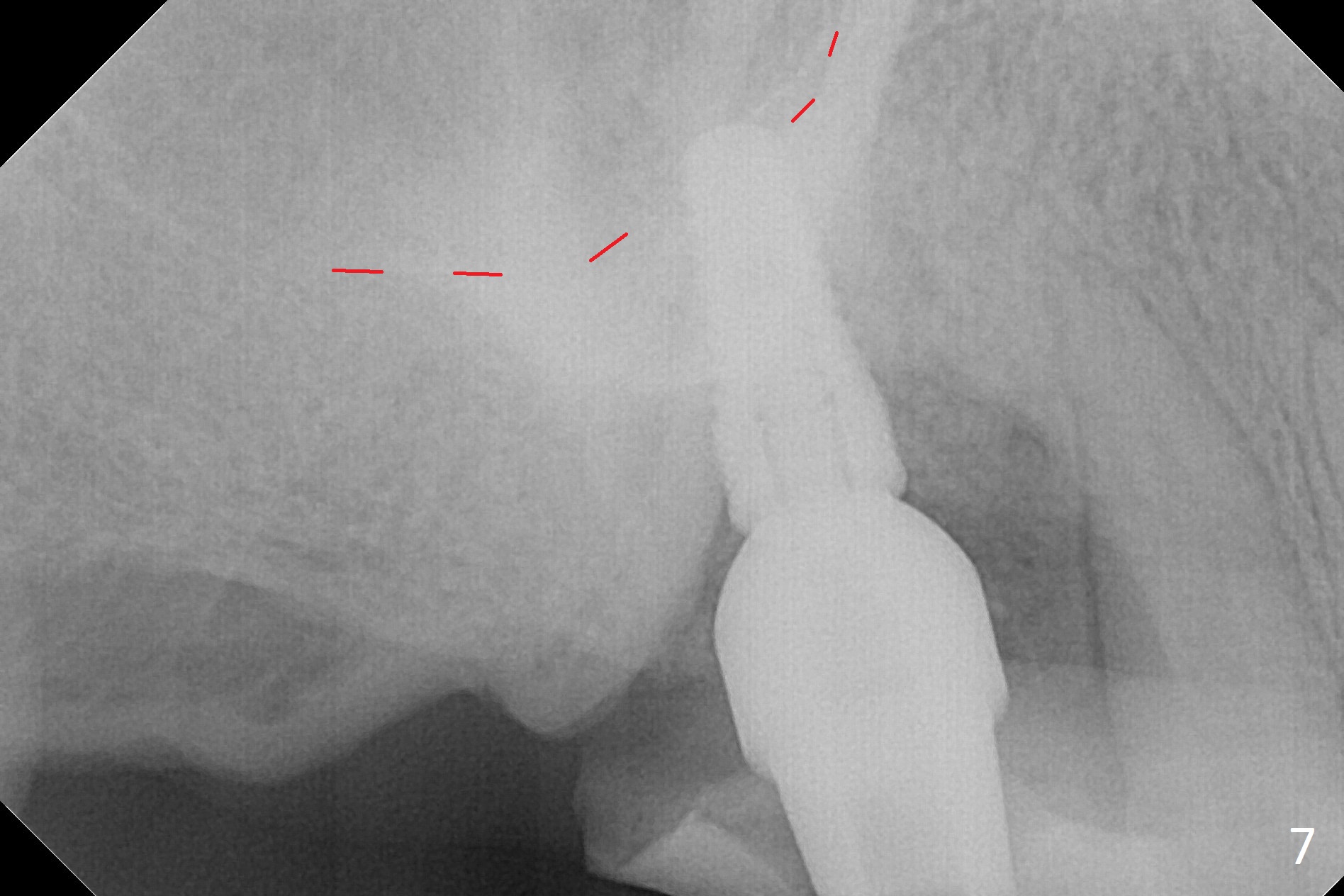
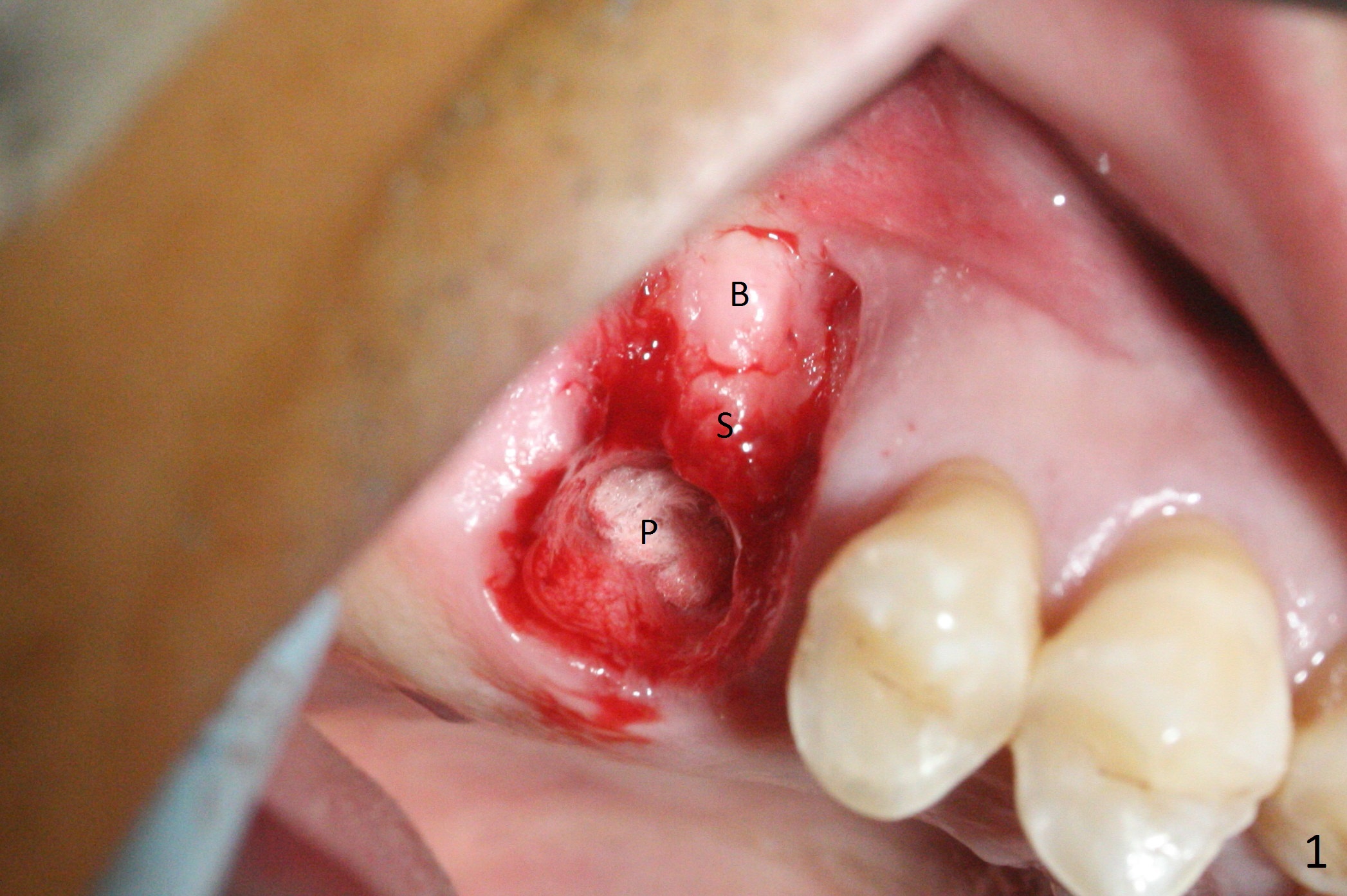
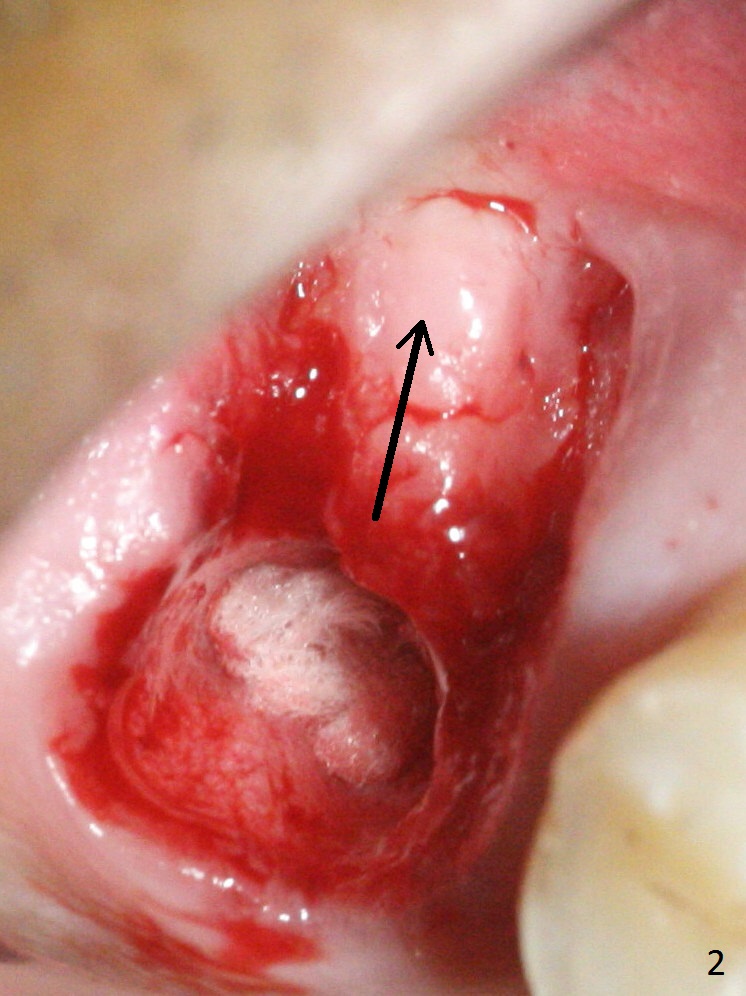
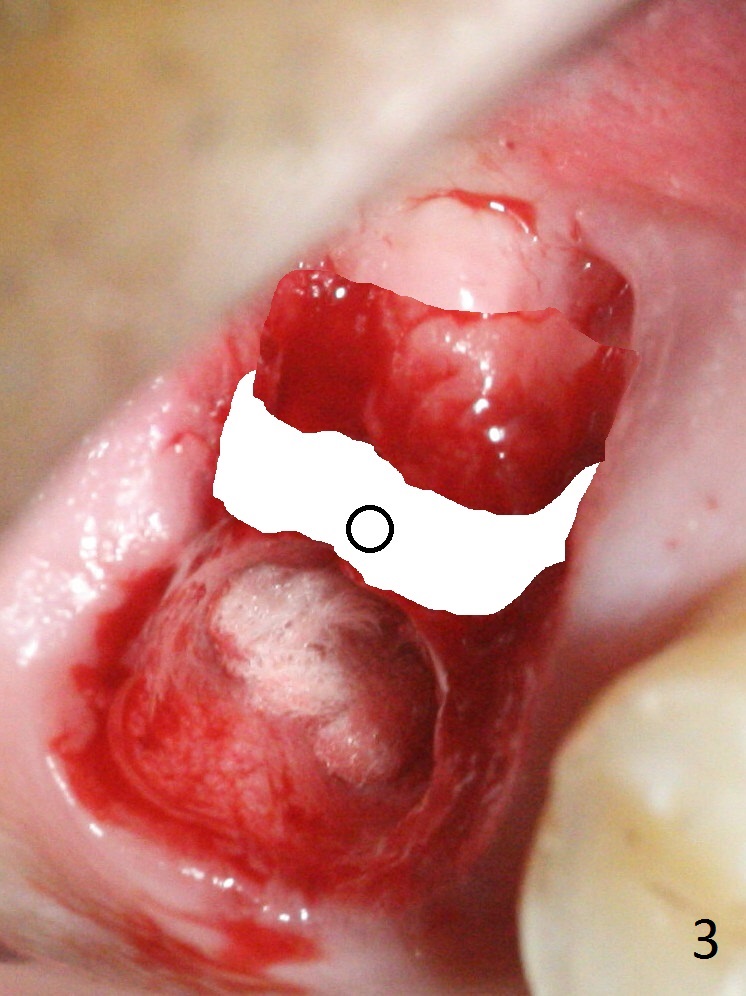
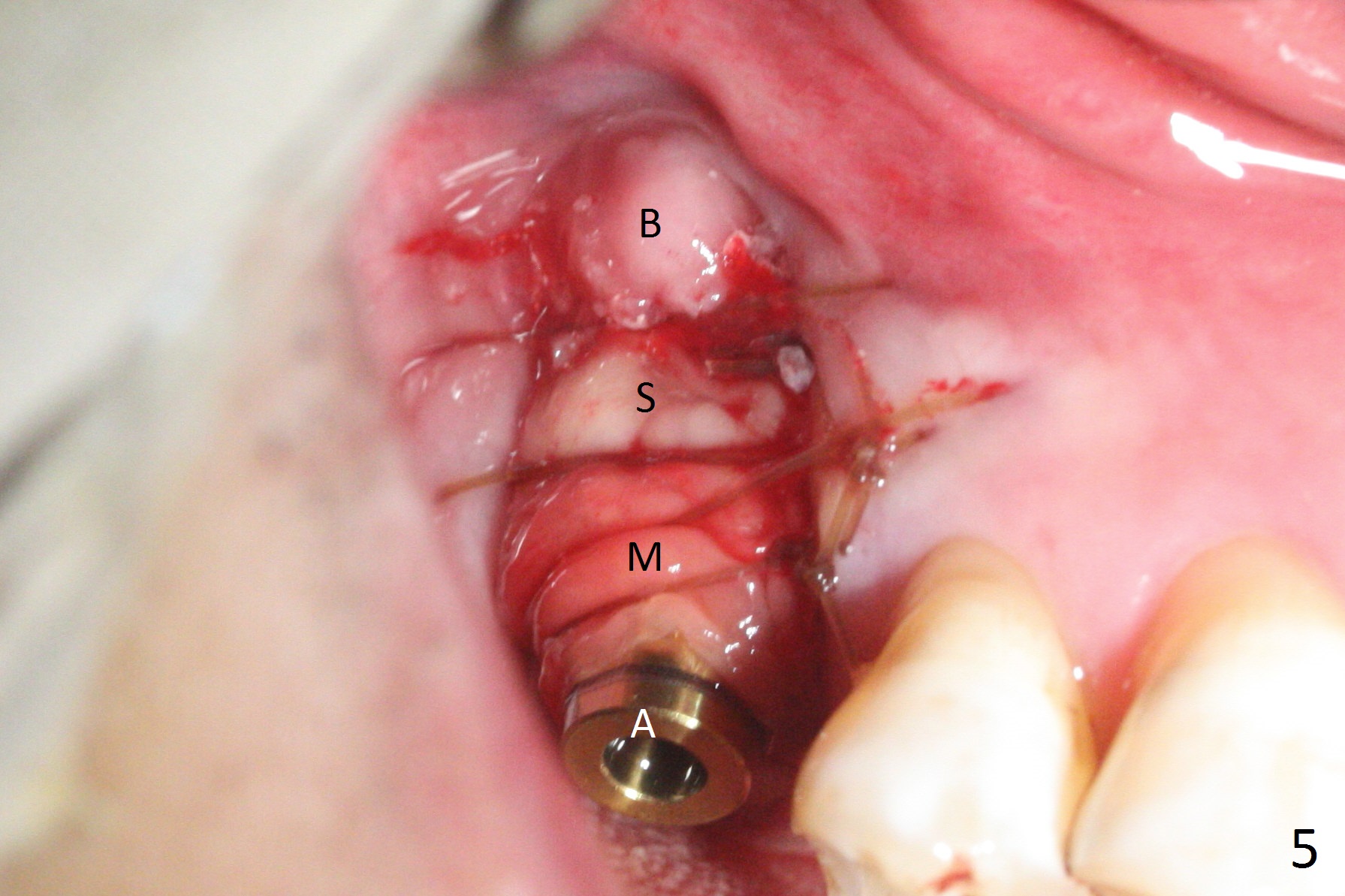
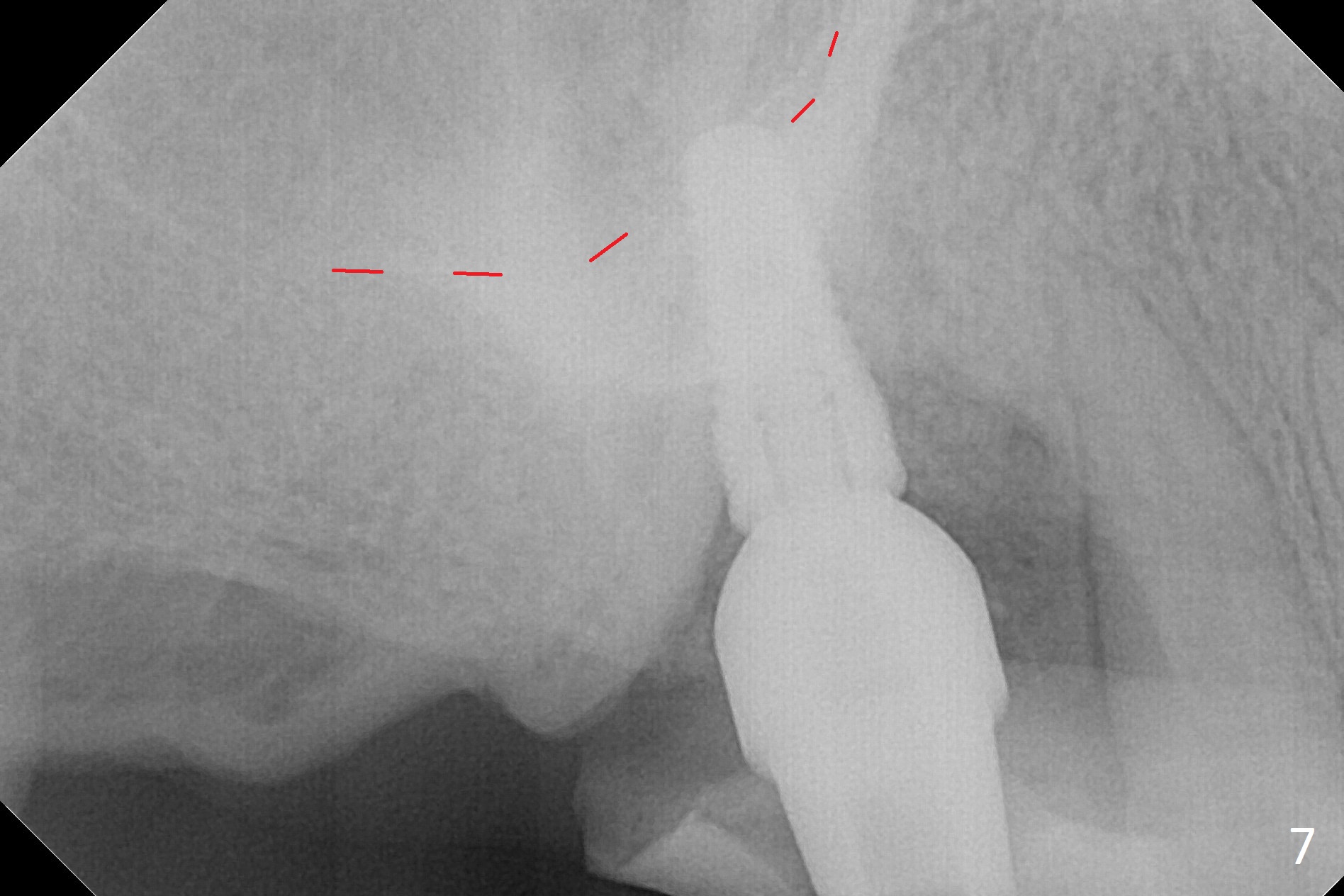
The palatal socket (Fig.1 P, packed with gauze) is intact, but implant trajectory may not be ideal. Buccal to the palatal socket are 2 pieces of the gingiva, buccal (B) and Septal (S). After the septal gingiva is pushed buccally (Fig.2 arrow), the underlying sloped septal bone is exposed (Fig.3 white area). Osteotomy is established as palatal as possible (Fig3 black circle) using DIO Sinus Master Kit, supplemented by Tatum osteotomes and DIO SM 3.8 mm tap drill for final sinus lift (Fig.4). Following further osteotomy using 4.1 and 4.5 mm taps, a 4.5x10 mm implant (Fig.6,7) with insertion torque >65 Ncm. Due to buccal bone loss, the coronal buccal threads are exposed 1-2 mm, which is covered by combination of allograft, autogenous bone and Osteogen. Prior to implantation, PRF plug and bone graft are used for sinus lift. The septal gingiva now is approximately 1-2 mm coronal to the implant plateau (Fig.5 S). The most coronal buccal gingival defect is covered by 3 pieces of PRF membrane (Fig.5 M) against a 6.8x5.5(6) mm abutment (A). Finally the socket is protected by periodontal dressing (Fig.8).
The distopalatal portion of the periodontal dressing dislodges 10 days postop. It appears after removal of the remaining dressing that PRF membranes has dissolved, while the remaining buccal and septal gingiva is healing (Fig.9). The wound leaves open for secondary healing.
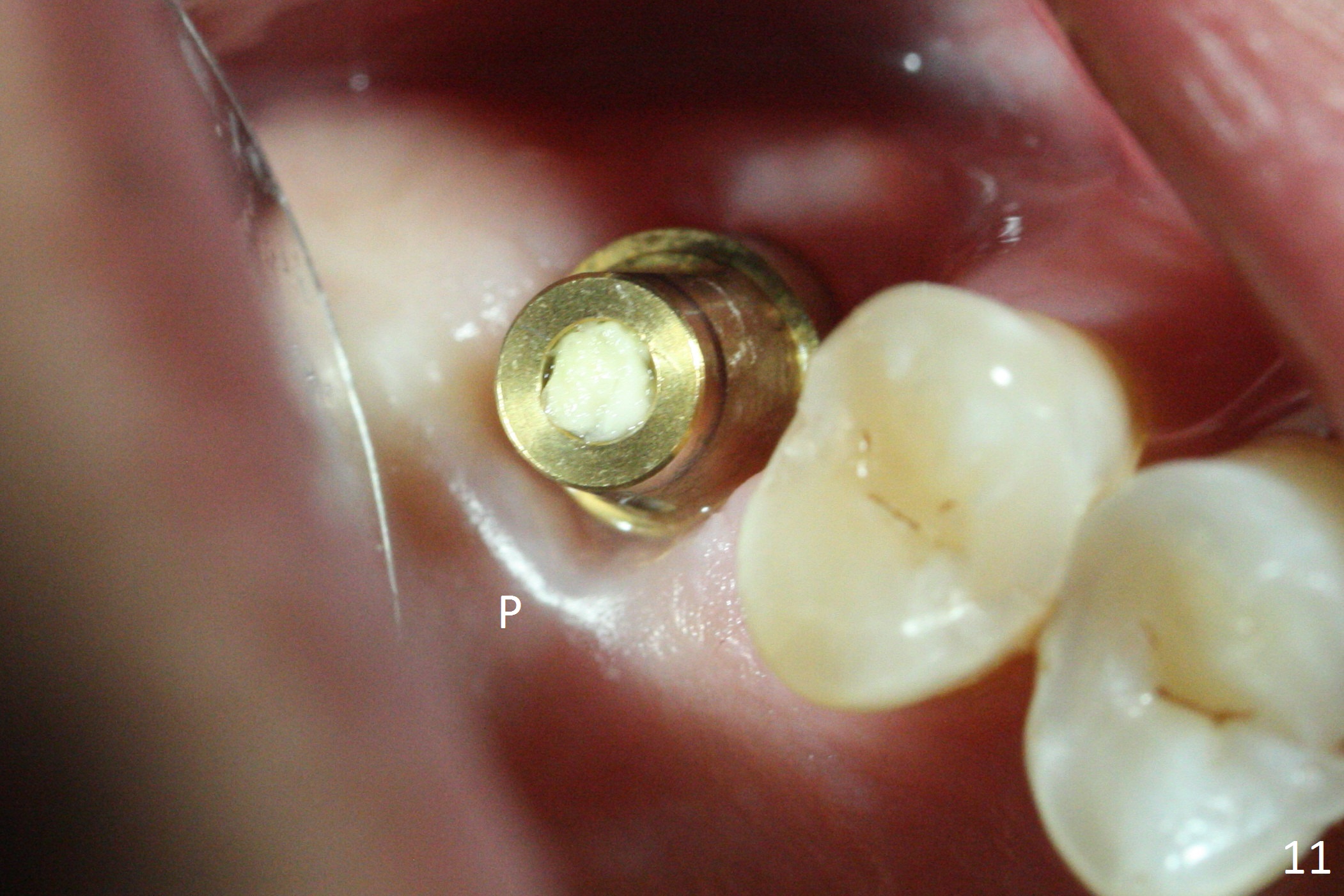
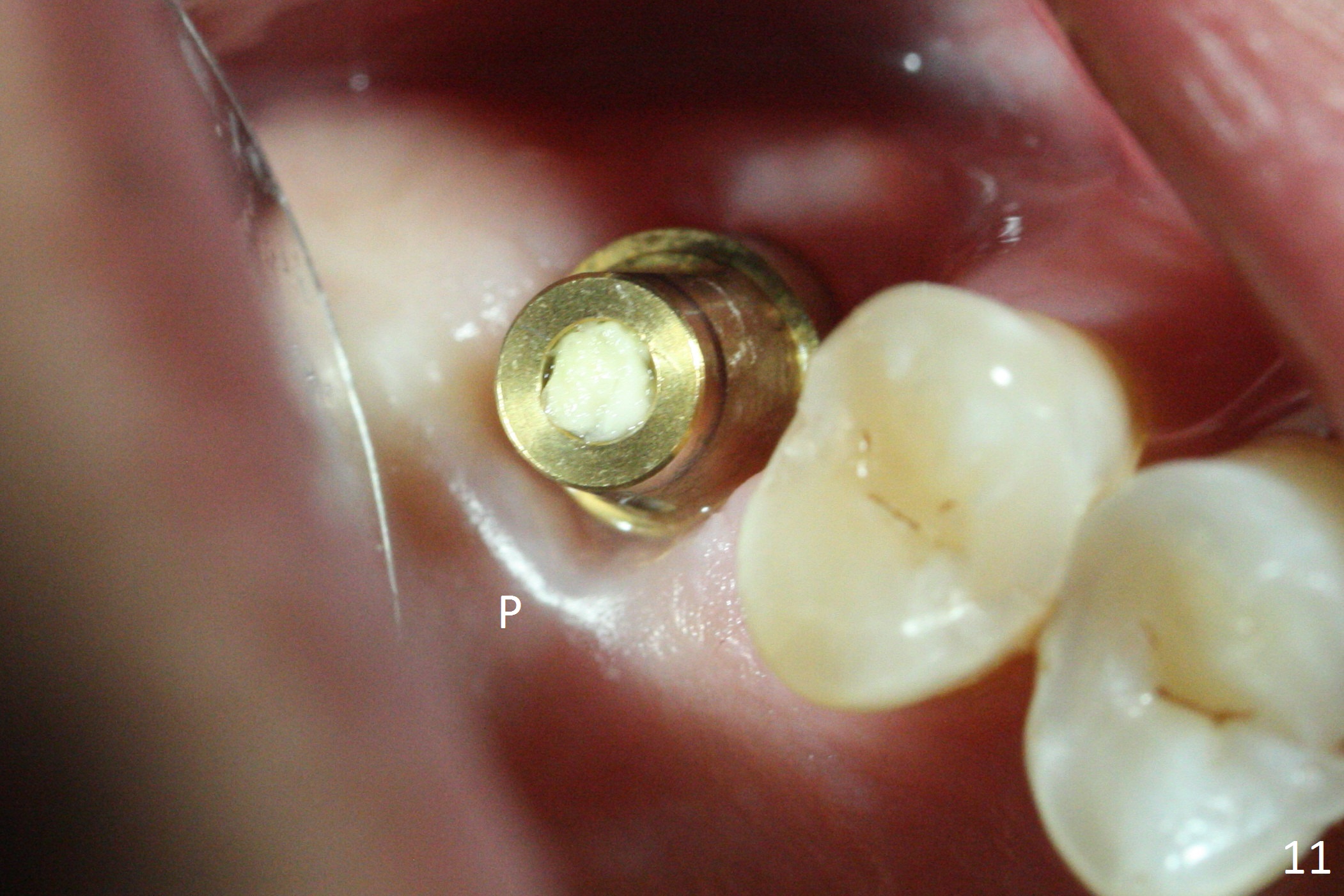
The buccal margin remains supragingival (Fig.10), while the palatal one subgingival 1.5 months postop (Fig.11 P). The abutment is changed to 4.8x7(3) mm (Fig.12). A provisional is fabricated to keep the palatal space for easy impression later on. With the smaller abutment and less tension, the buccal gingiva is expected to grow more coronal to reduce recession.
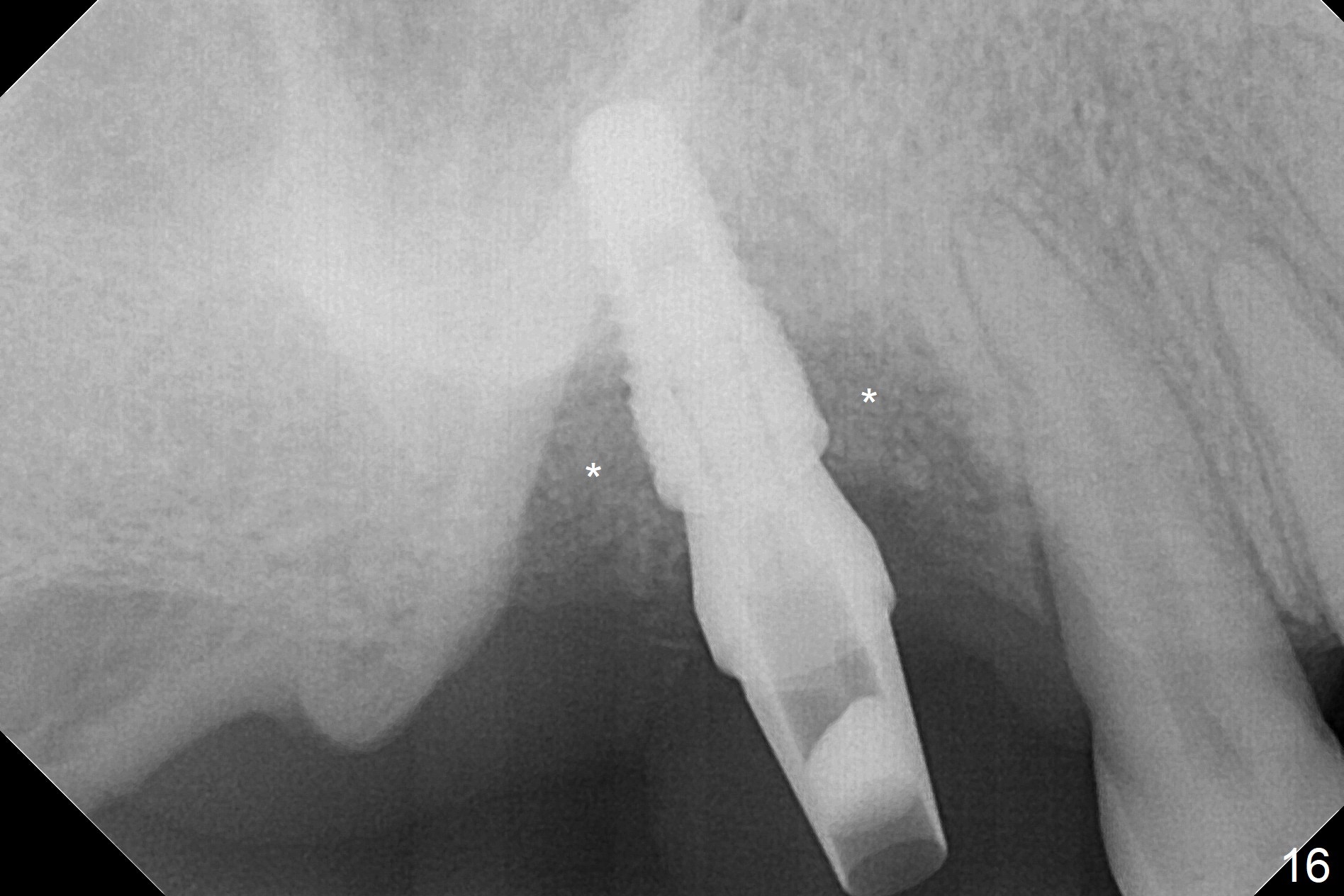
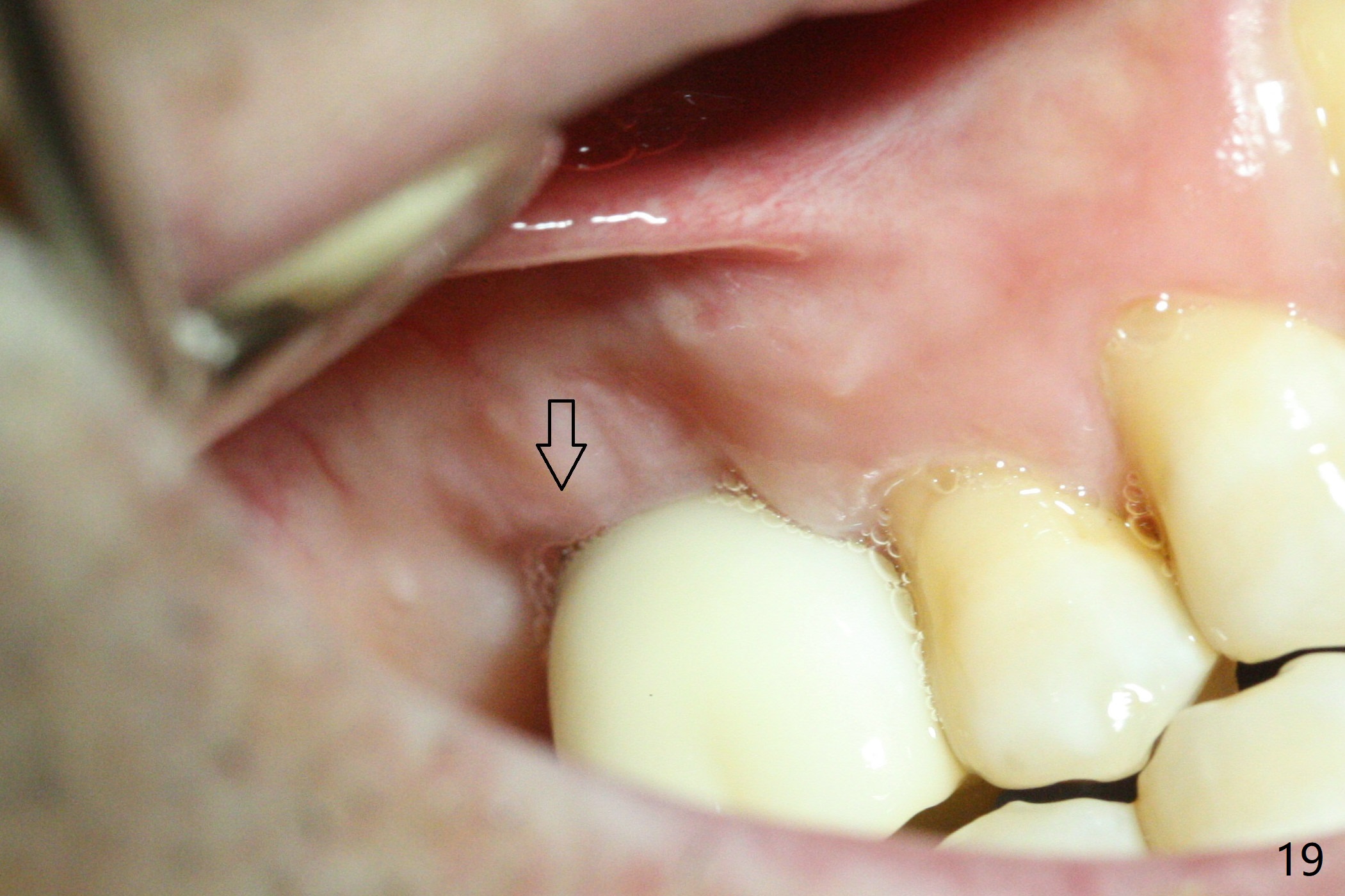
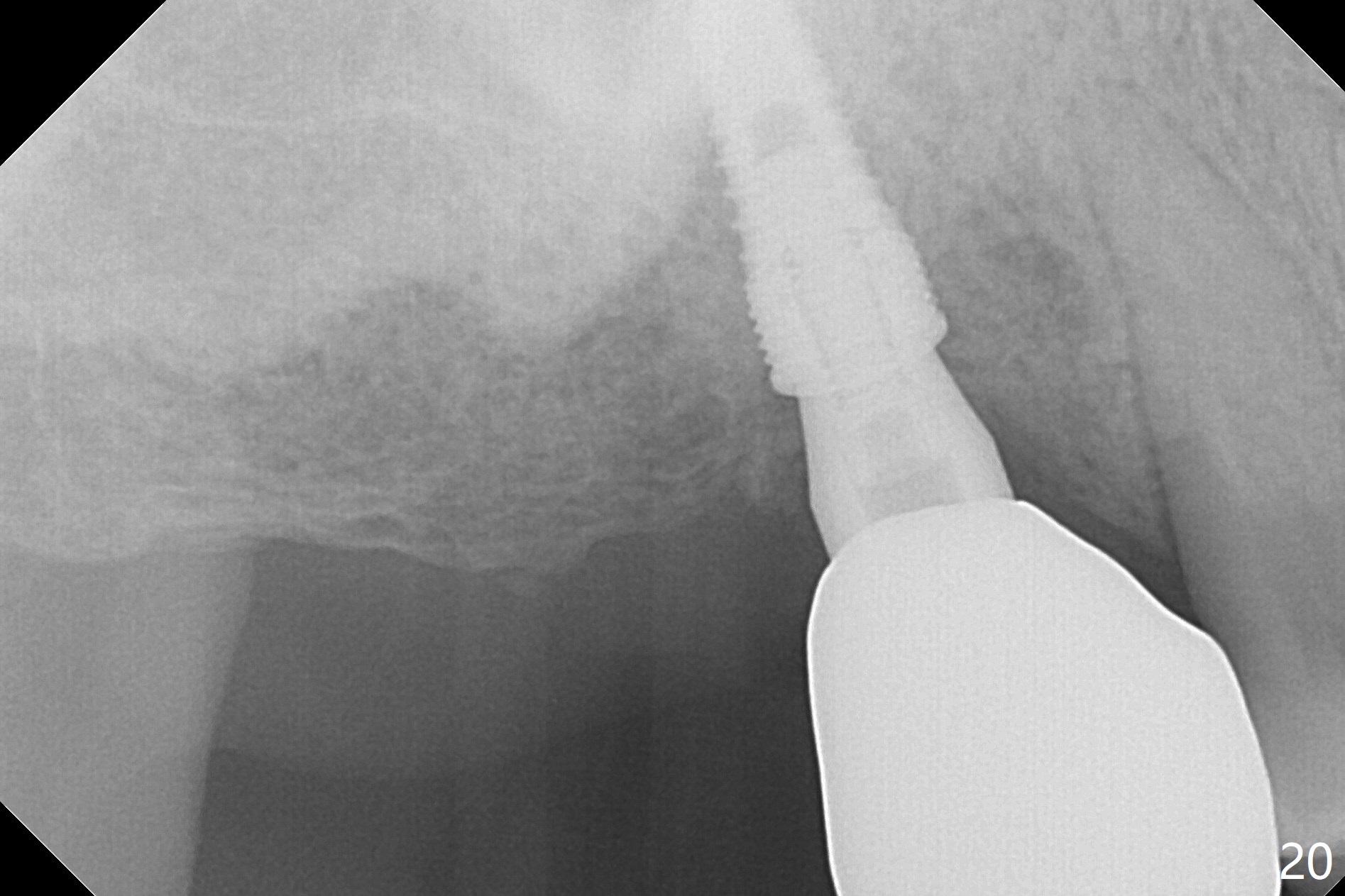
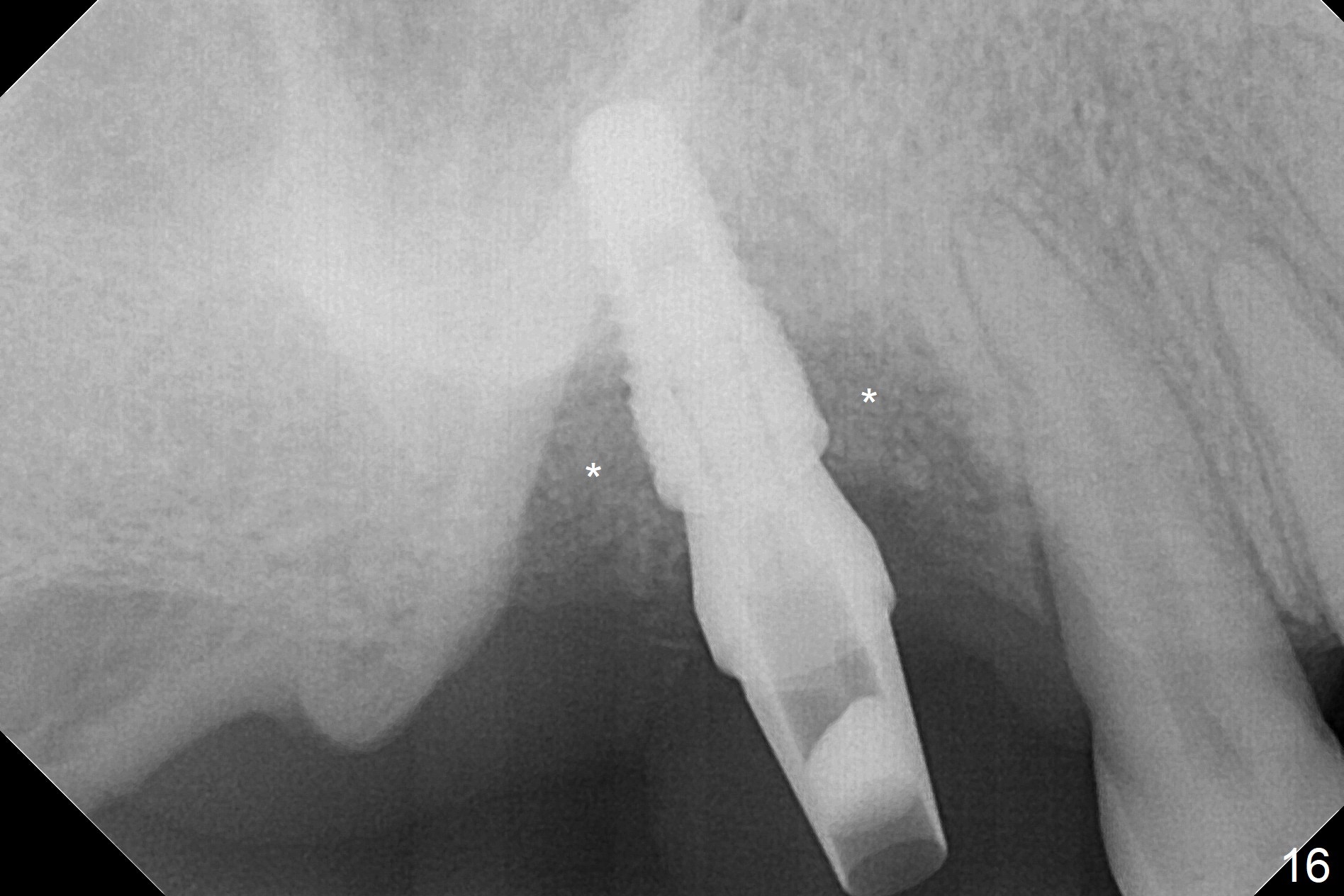
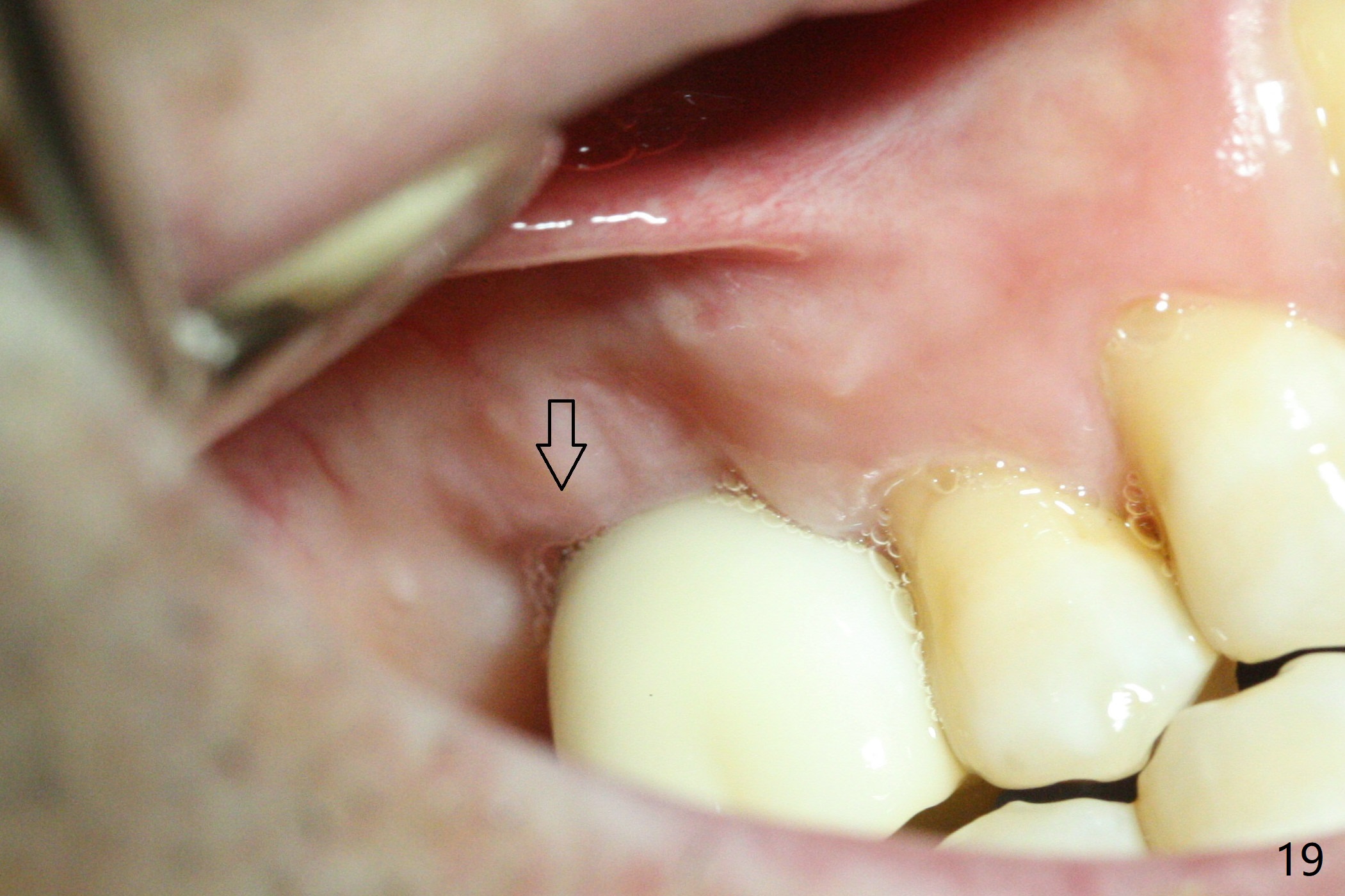
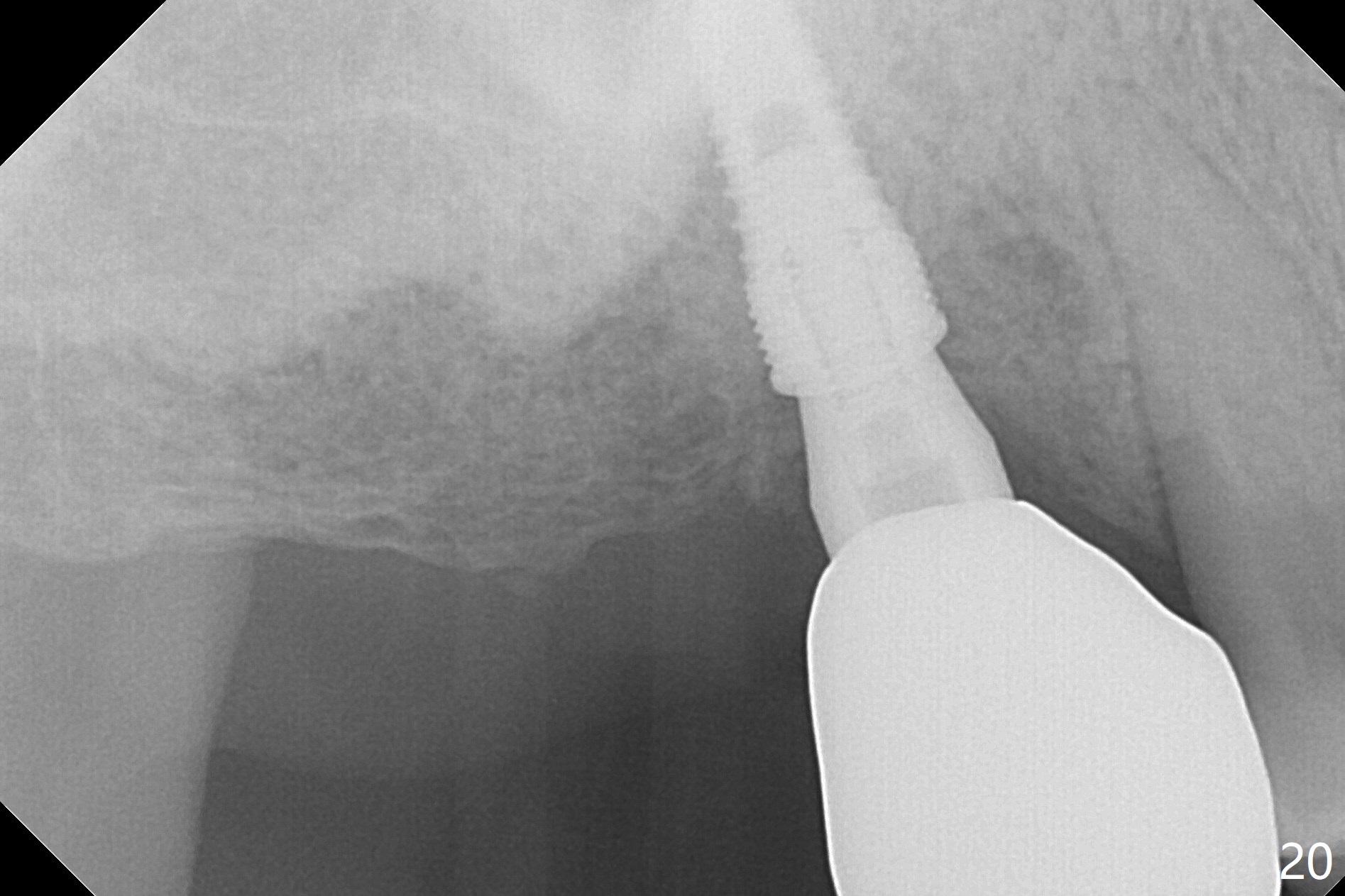
Two weeks later, the buccal gingiva appears to have grown downward (Fig.13). Fig.14 is taken when the provisional is removed. To facilitate this process, change abutment from 4.8x7(3) to (4.5) mm and a new provisional is fabricated (Fig.15): note the metal exposure distobuccally. When the patient returns in another two week, the gap should be able to disappear. There is no loss of bone graft 3 months postop (Fig.16). Two weeks later (3.5 months postop), the margin of the abutment is supragingival buccally and subgingival palatally (Fig.17,18). The gingiva seems to have migrated downward (Fig.19 arrow), while the bone density around the coronal implant appears to increase 5.5 months post cementation (Fig.20). There is buccal swelling with purulent discharge 1.5 years post cementation (Fig.21). Perimplantitis develops. Tuberosis bone graft will be performed when the limited ortho is finished.
Return to
Upper
Molar Multiple Tooth Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table), IBS, #9, 19,
23
Buccal Root Exposure
Xin Wei, DDS, PhD, MS 1st edition 04/24/2017, last revision 02/28/2019