







 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
Apical Buccal Plate Perforation
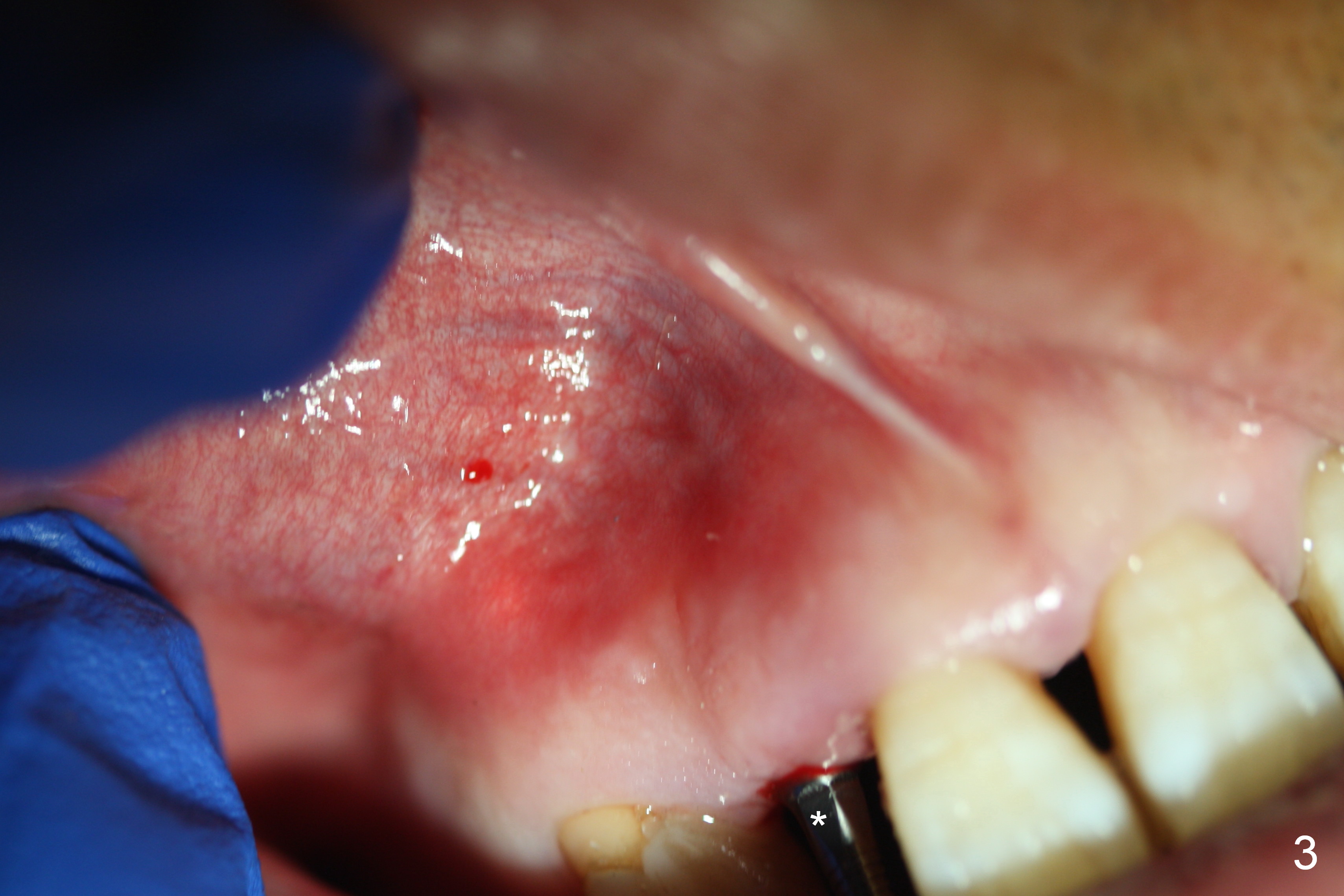
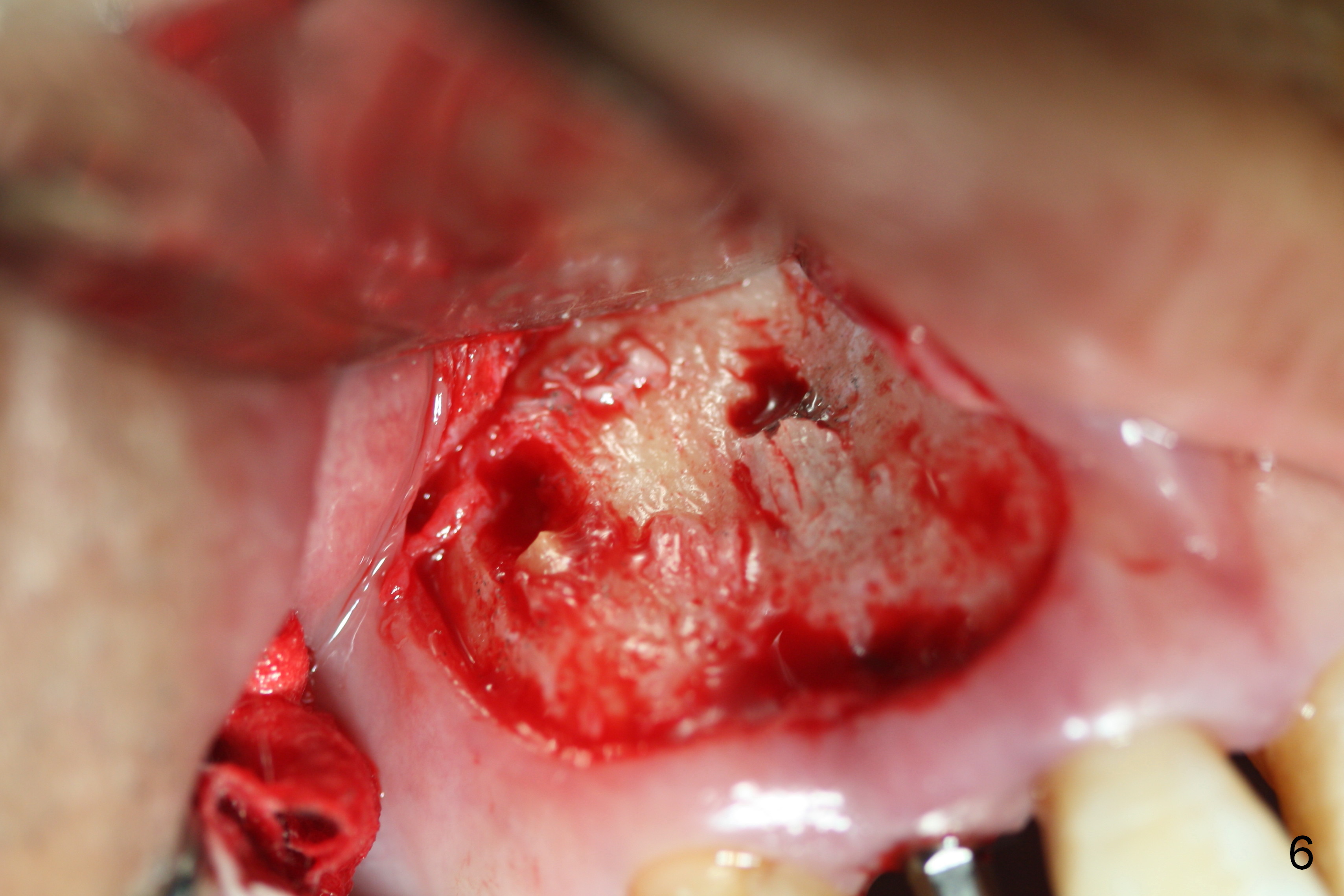
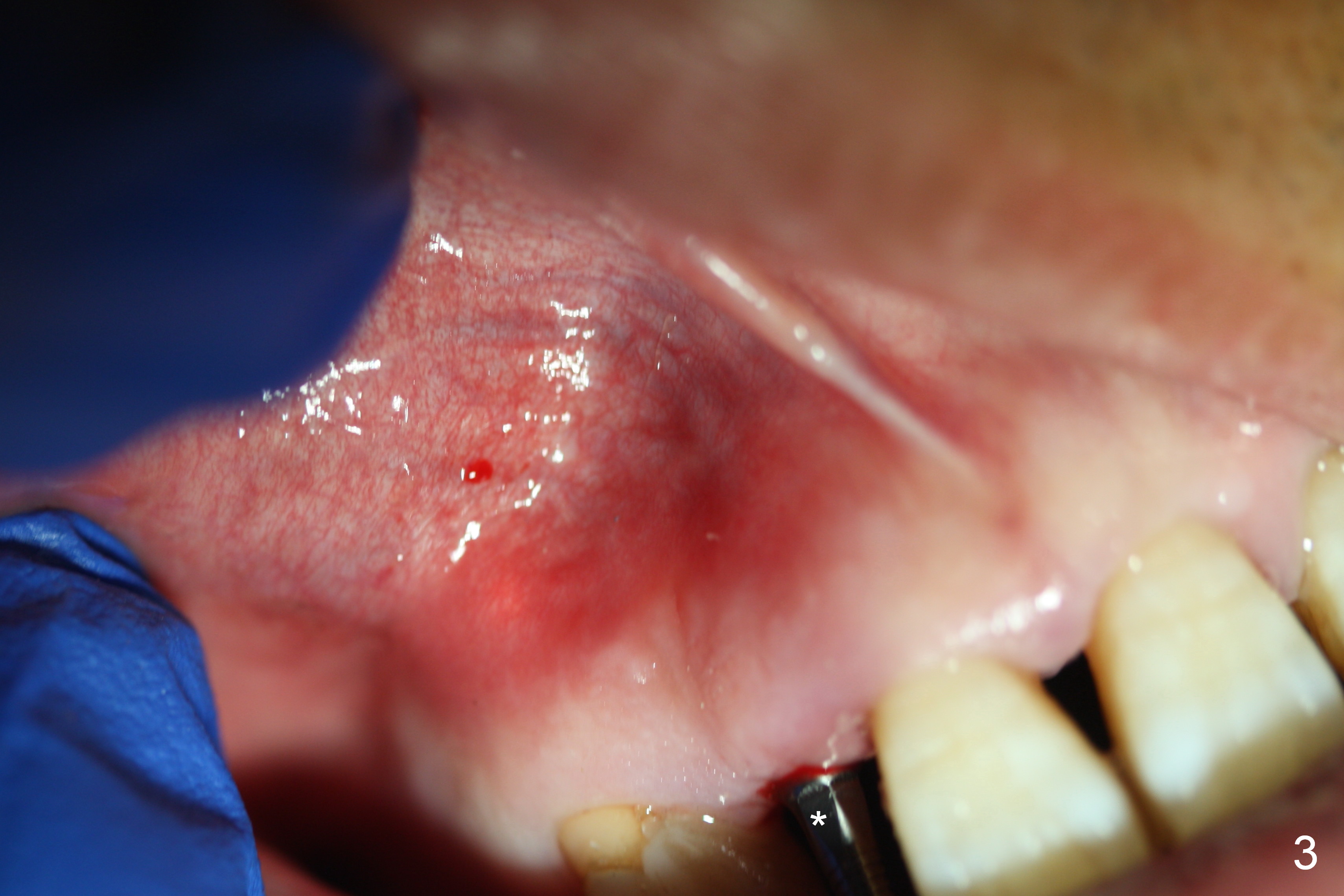
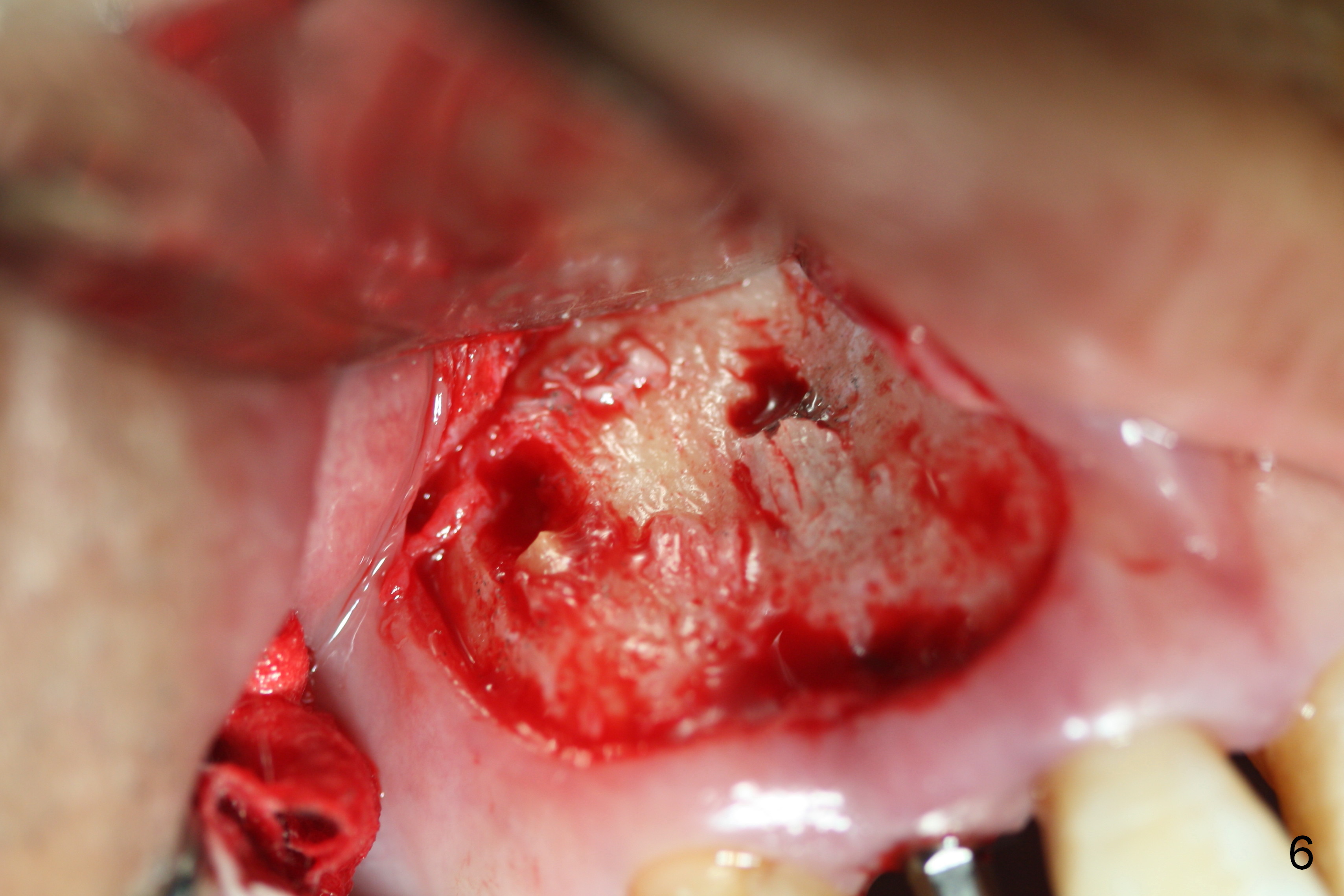
Preop exam shows the apparent wide ridge at #7 (Fig.1). What is ignored preop is the concavity in the apical buccal region (Fig.2 *). When a 3x16(4) mm 1-piece implant is being placed (Fig.3 *, flapless), the apical buccal plate vibration is felt. The biggest mistake is that initial osteotomy is ~ 6 mm shy of the implant length, partially because of 6 mm gingival height. Since the tooth #6 is symptomatic after RCT with paste overfill (Fig.4 >), apicoectomy is contemplated at #6 with exploration of the buccal plate at #7 (Fig.5). Since the implant appears to be long enough, implant apical resection is performed (Fig.6). Since there is coronal thread exposure due to previous periodontitis (Fig.7 <), bone graft is placed in these 3 defective areas after decortication.
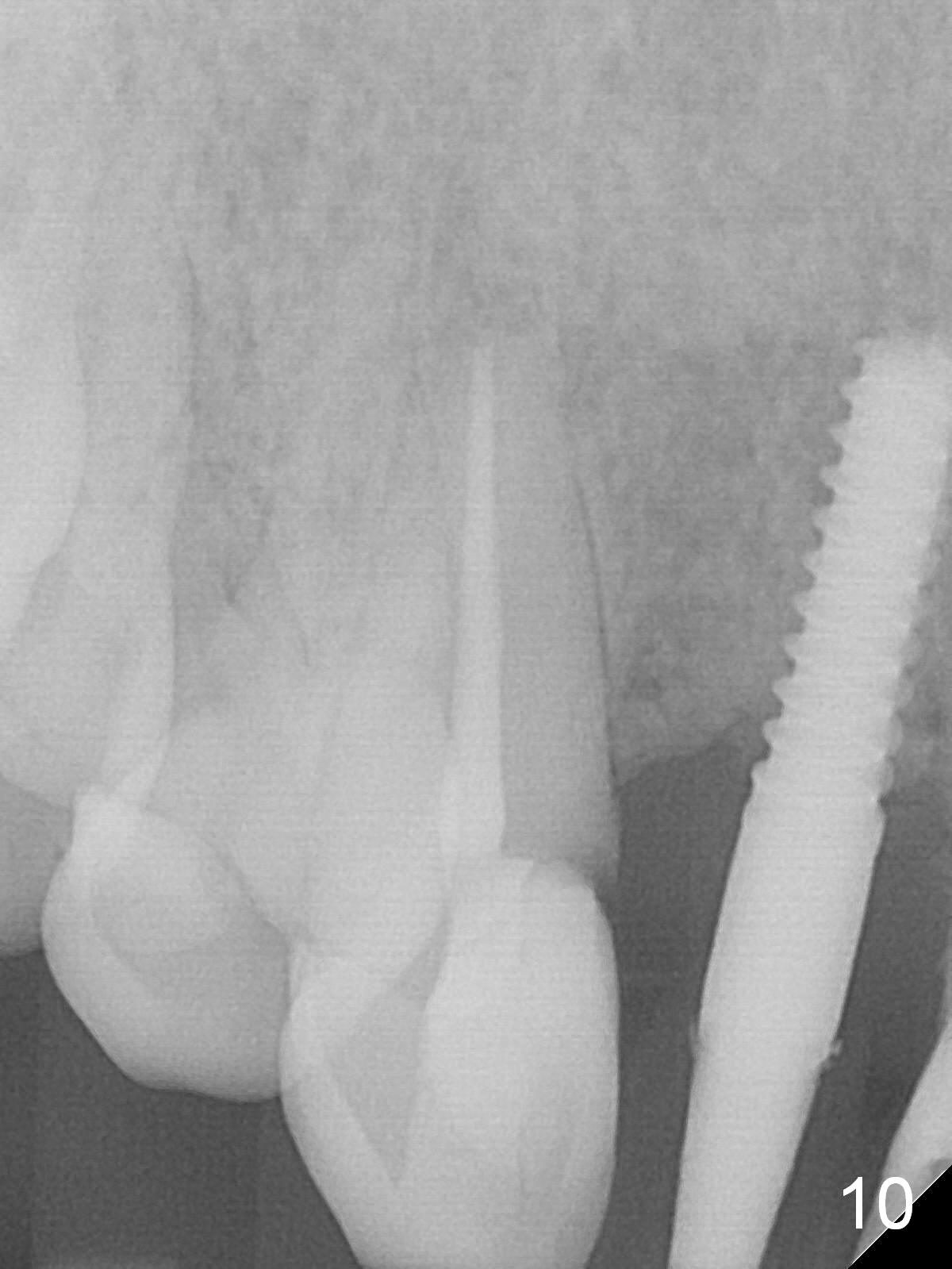
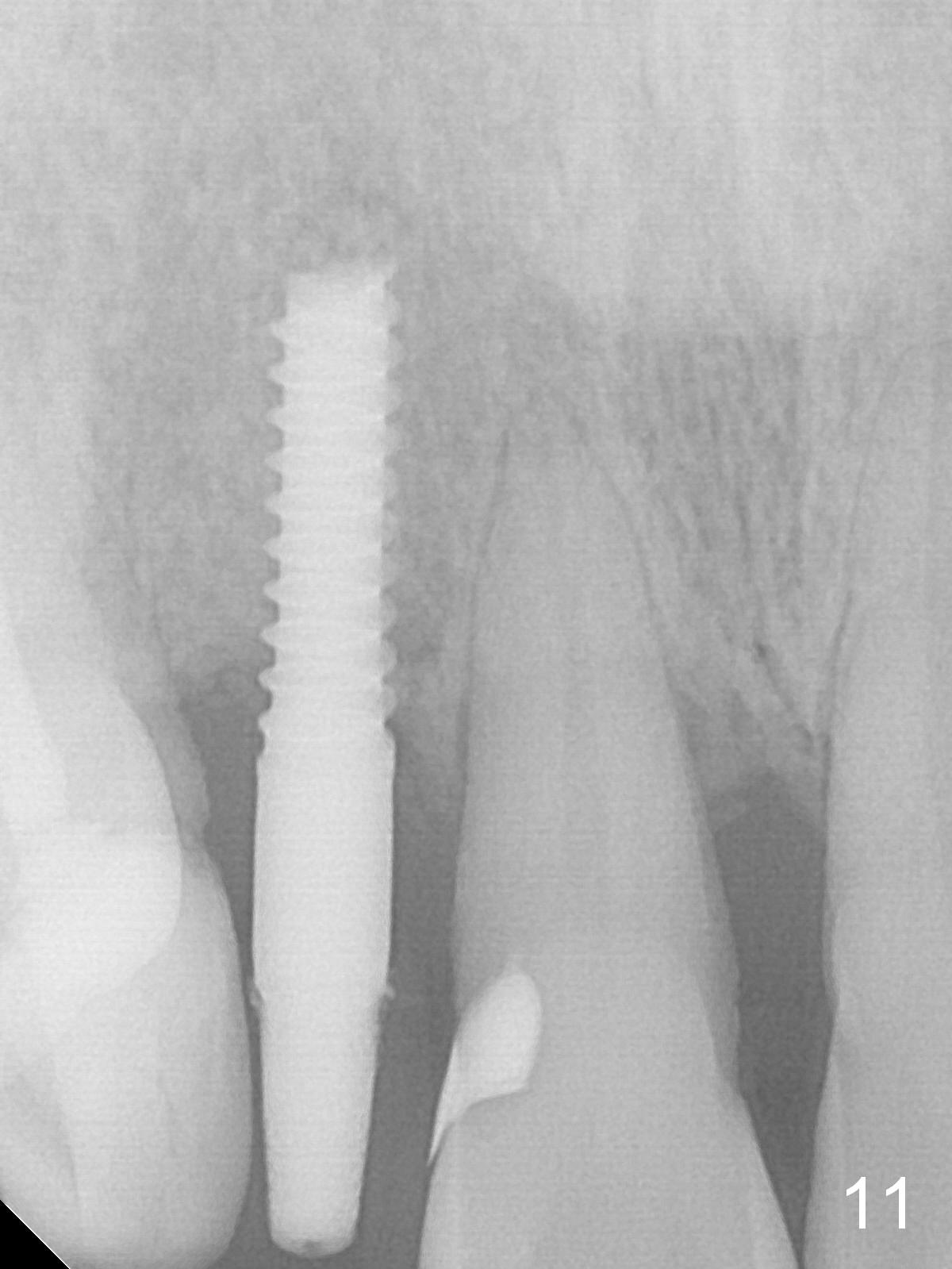
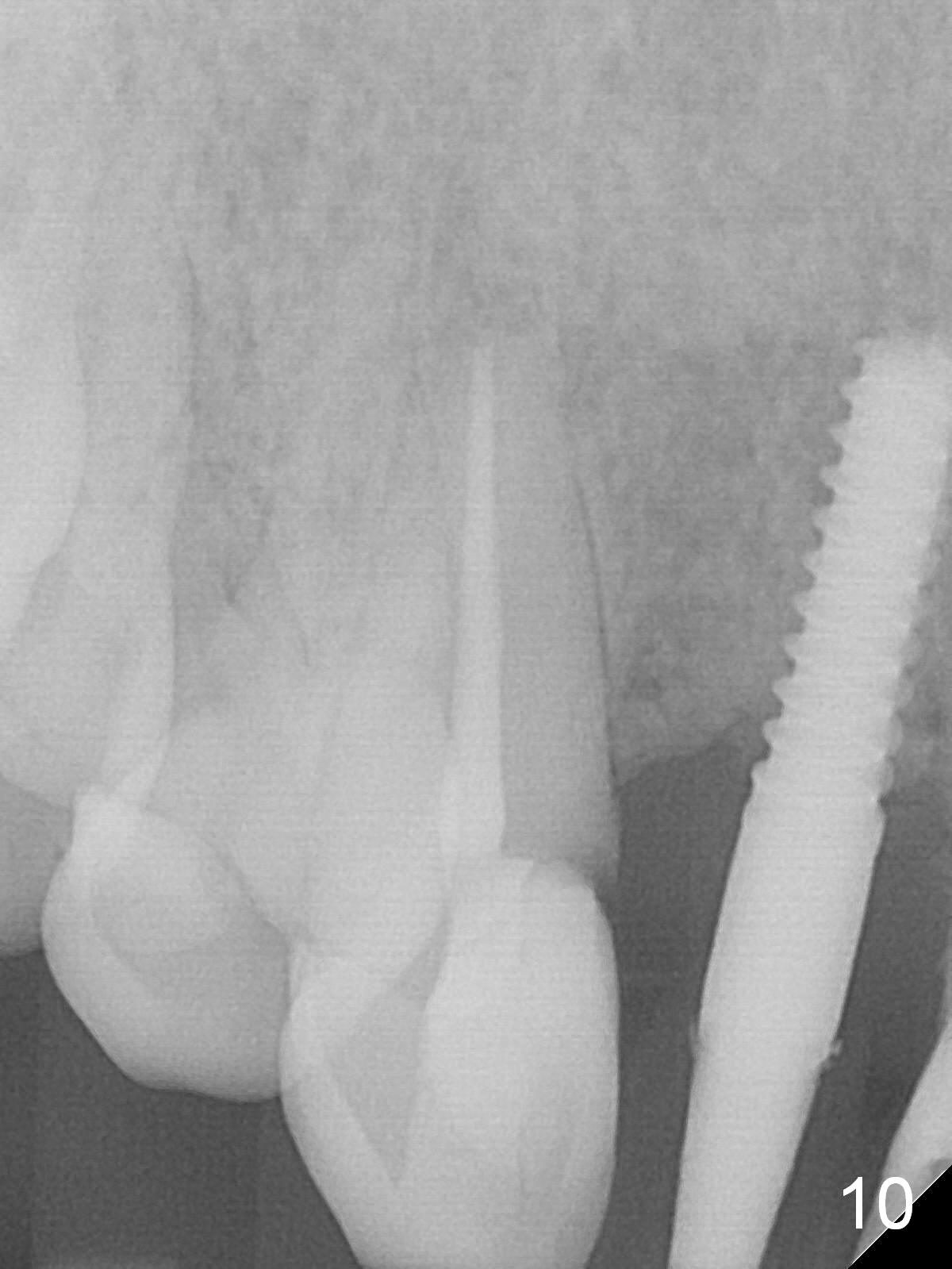
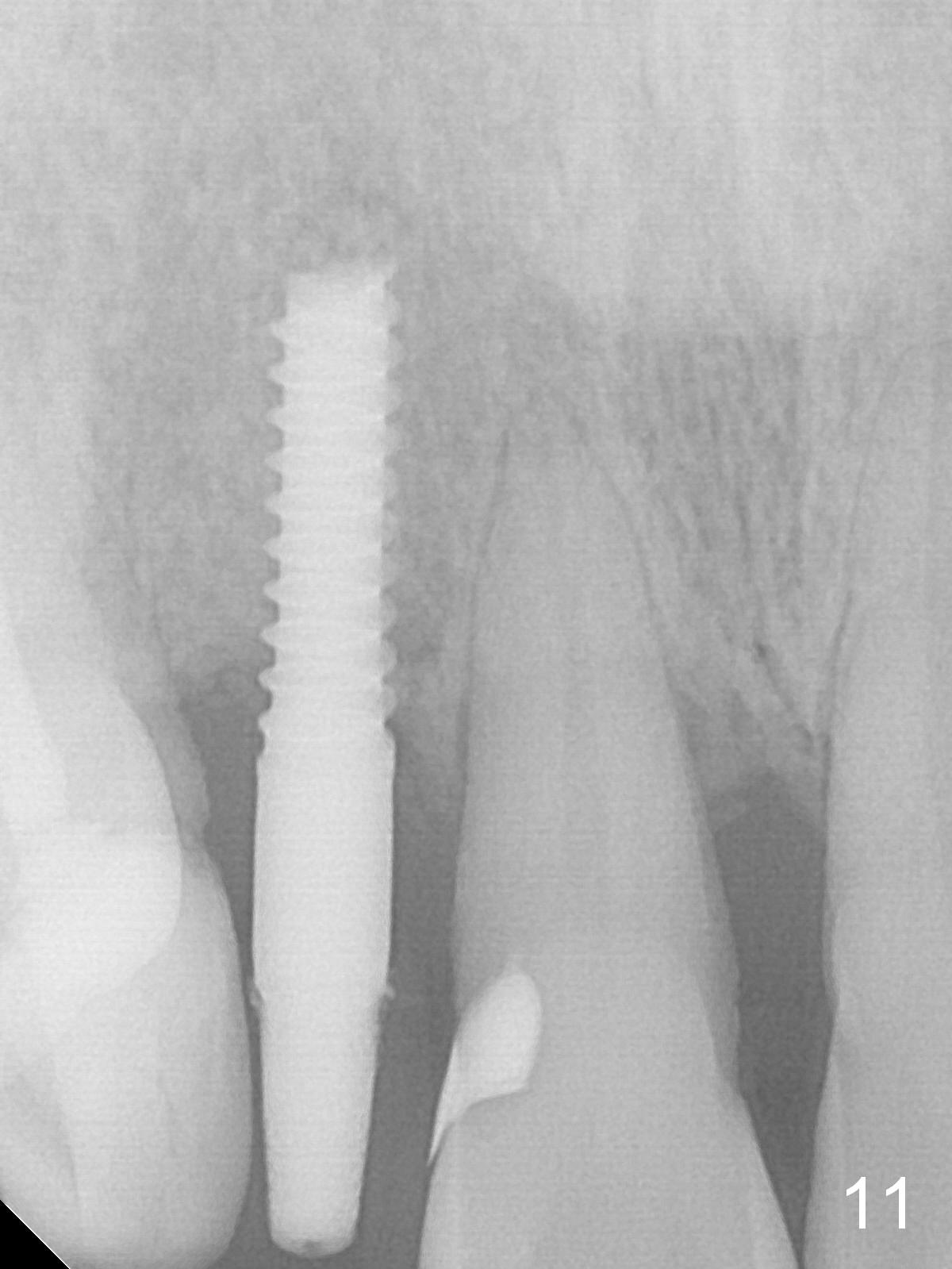
Extending the initial osteotomy to the full length of the implant is critical. If perforation is detected early, the trajectory can be changed. Incision should be made if there is no CBCT study. The incision heals 1 and 4 weeks postop (Fig.8,9). The patient returns for final restoration 6 months postop. Apical defects appear to have healed at #6 and 7 (Fig.10,11). Fig.12 is taken 11 months postop and 5 months post cementation. The patient has an accident 9 months post cementation. In fact the implant is alright, while the tooth #6 fractures and #8 subluxates.
Return to
Upper
Incisor, Full Arch Immediate
Implant, IBS,
#14,18,
19, 30,
1-Piece,
Atrophic Ridge
Xin Wei, DDS, PhD, MS 1st edition 09/15/2016, last revision 10/24/2018