














 |
 |
 |
|||
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
||
 |
 |
 |
|||
Find Problems and Solve Them While Implanting
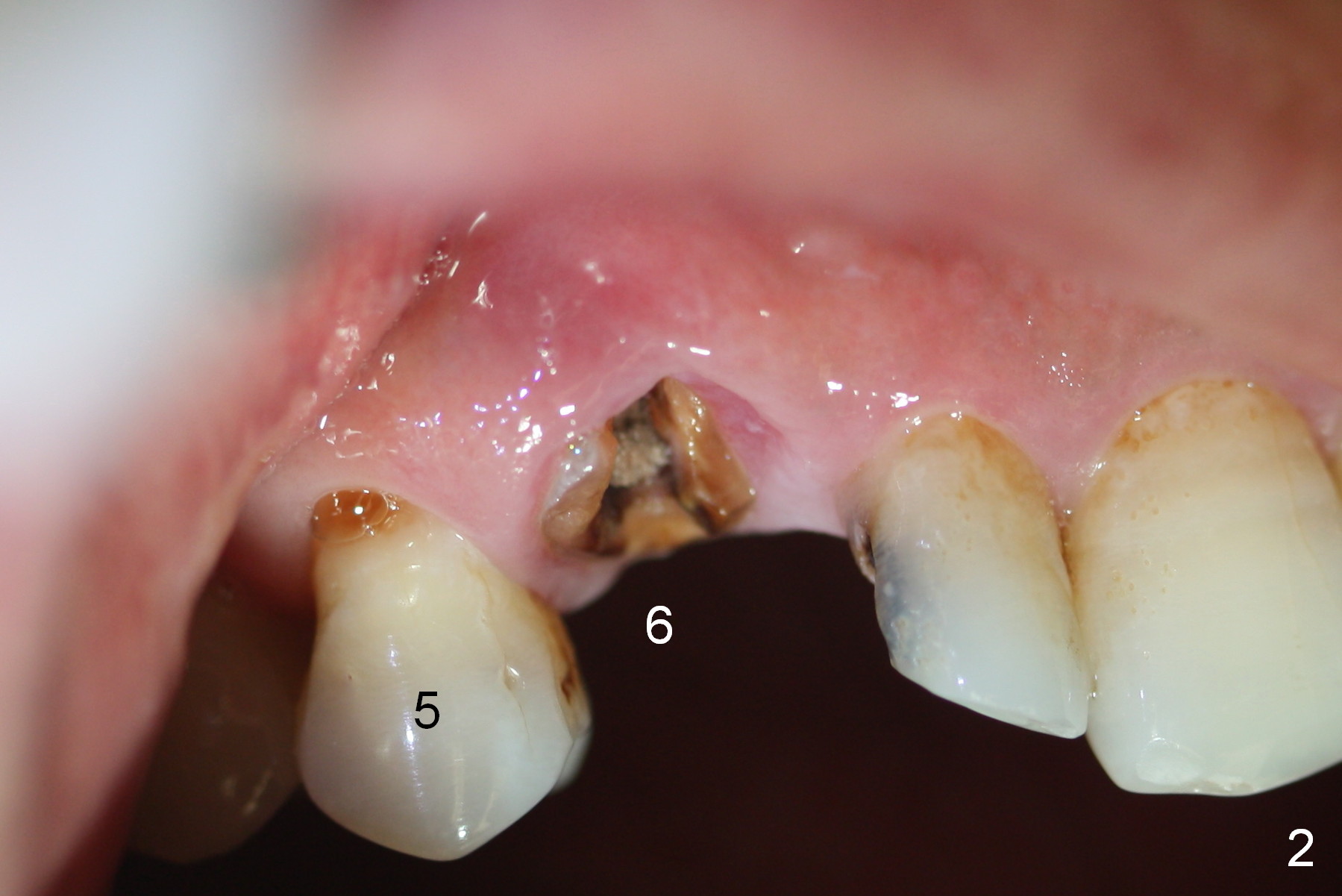
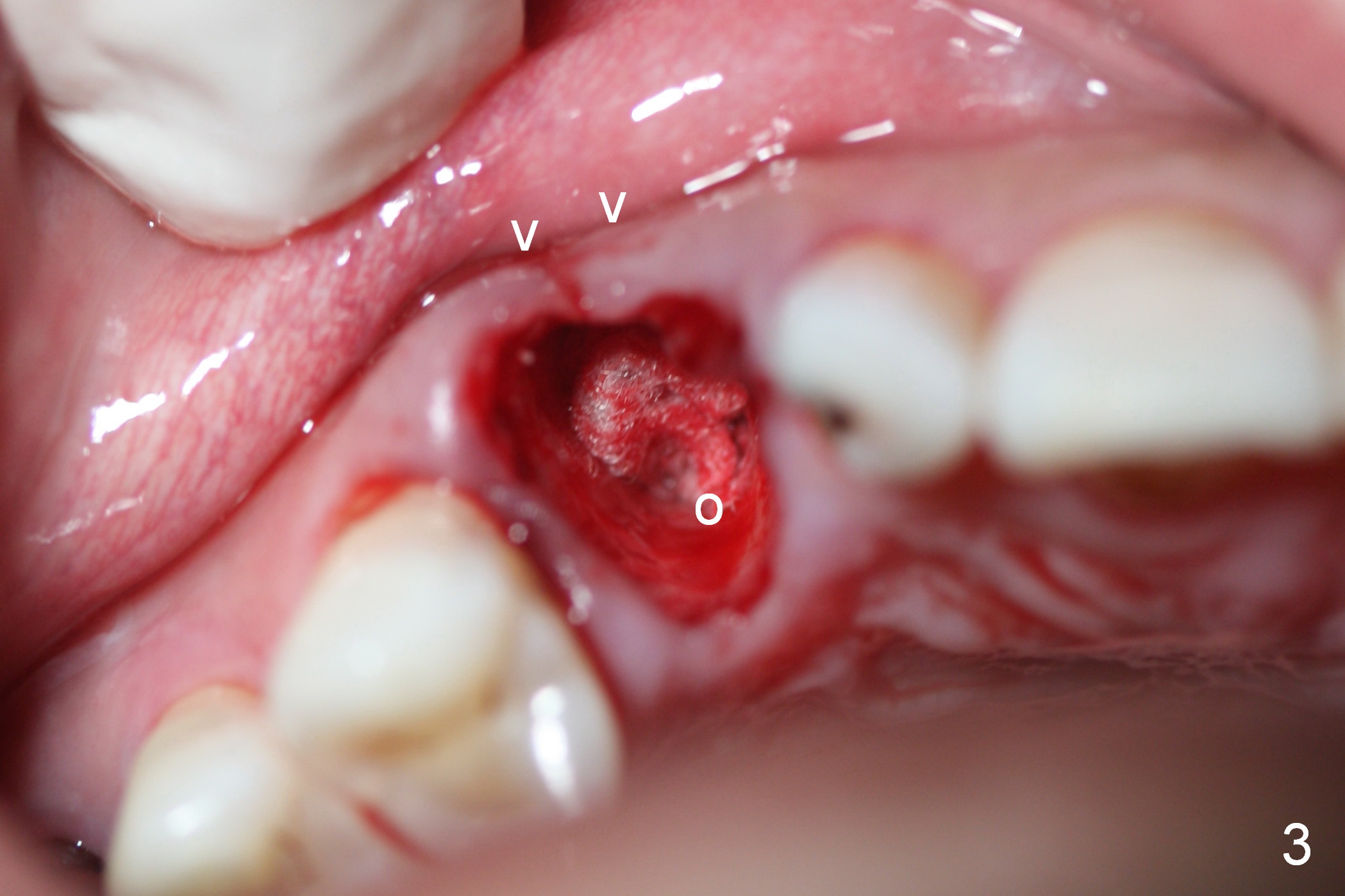
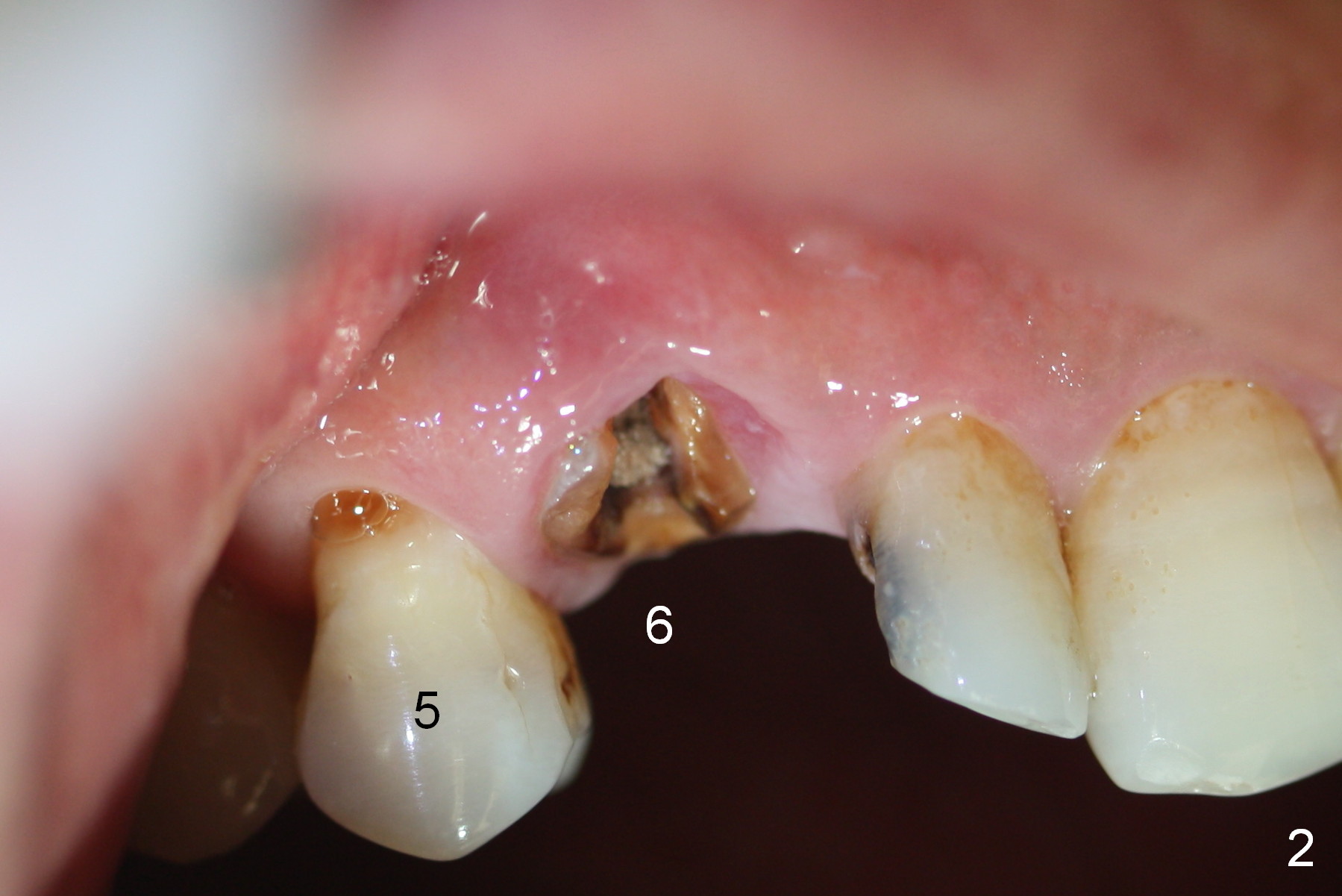
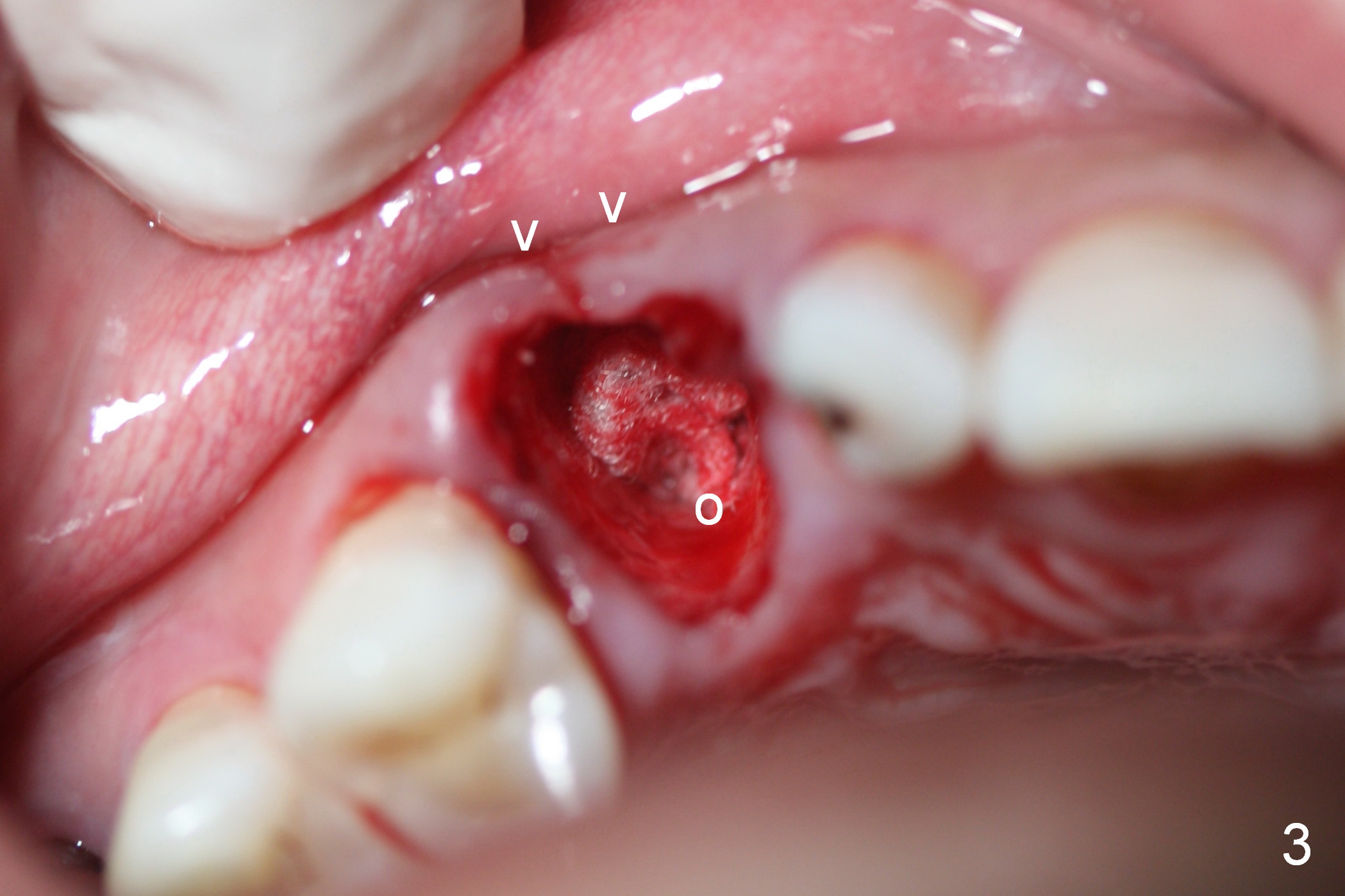
While the periodontal ligament is being severed with Proximators (periotomes), the tooth #6 is found closer to the tooth #5 (Fig.1,2). When the tooth is extracted, an osteotomy is initiated slightly mesially in the palatal wall of the socket (Fig.3 O).
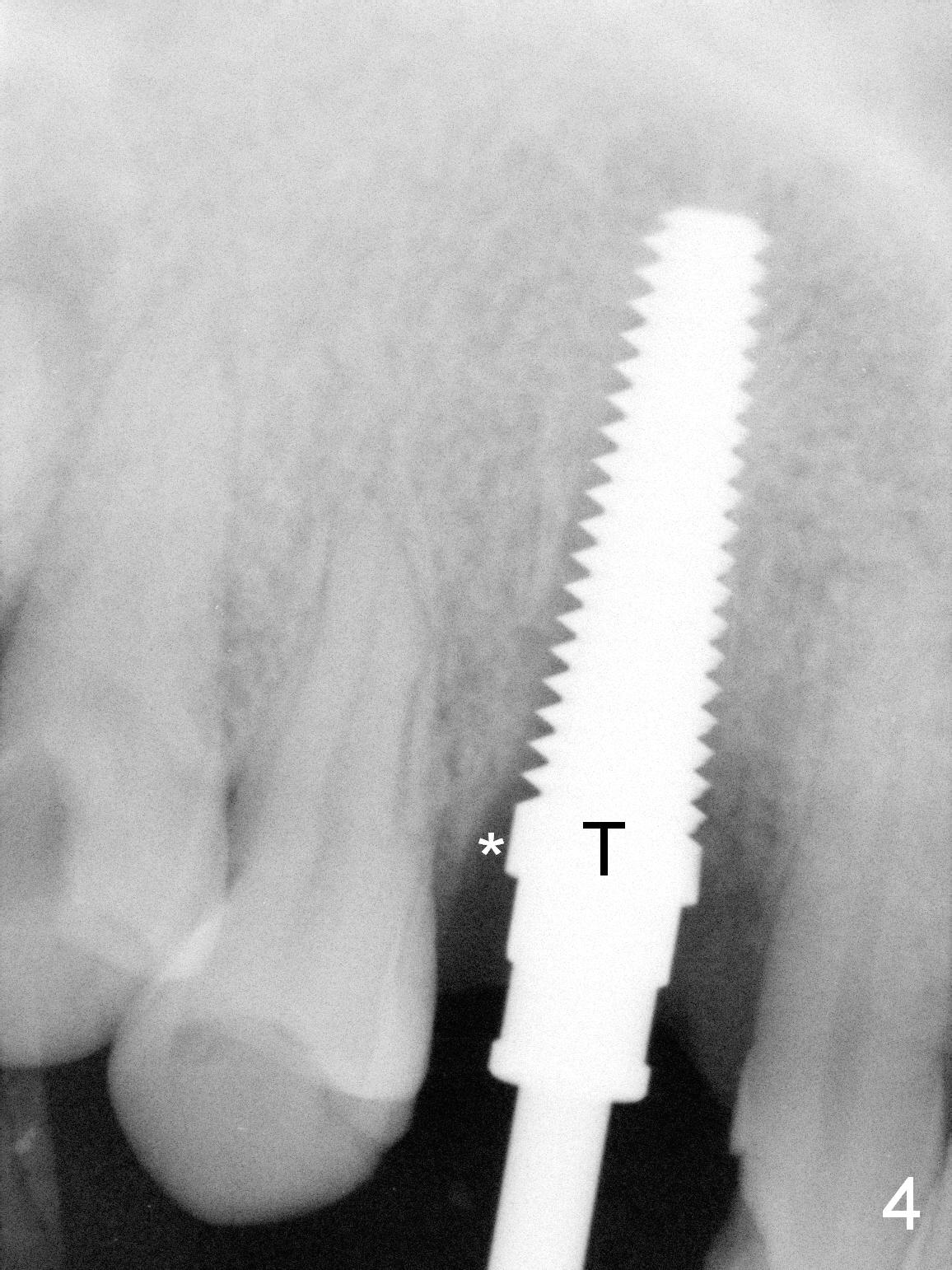
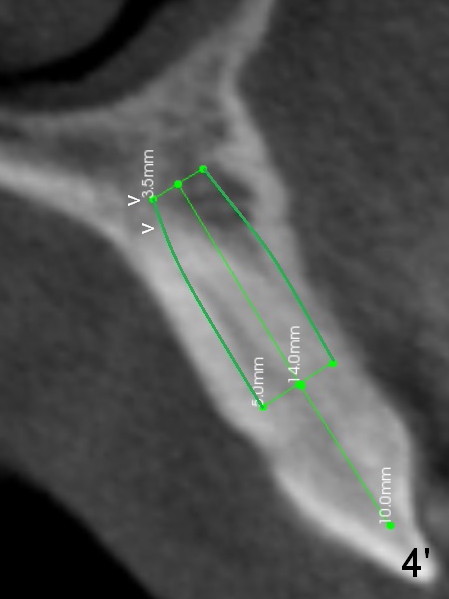
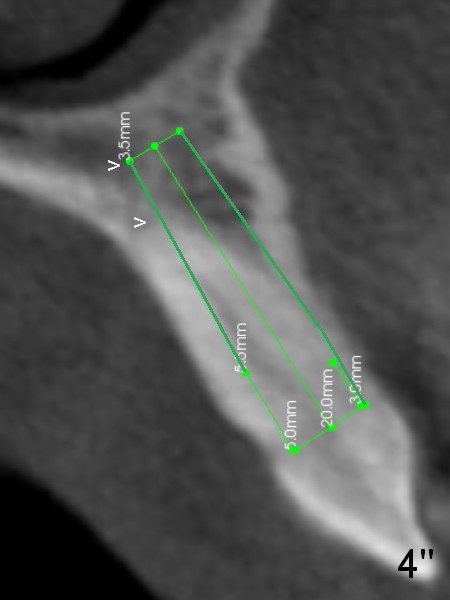
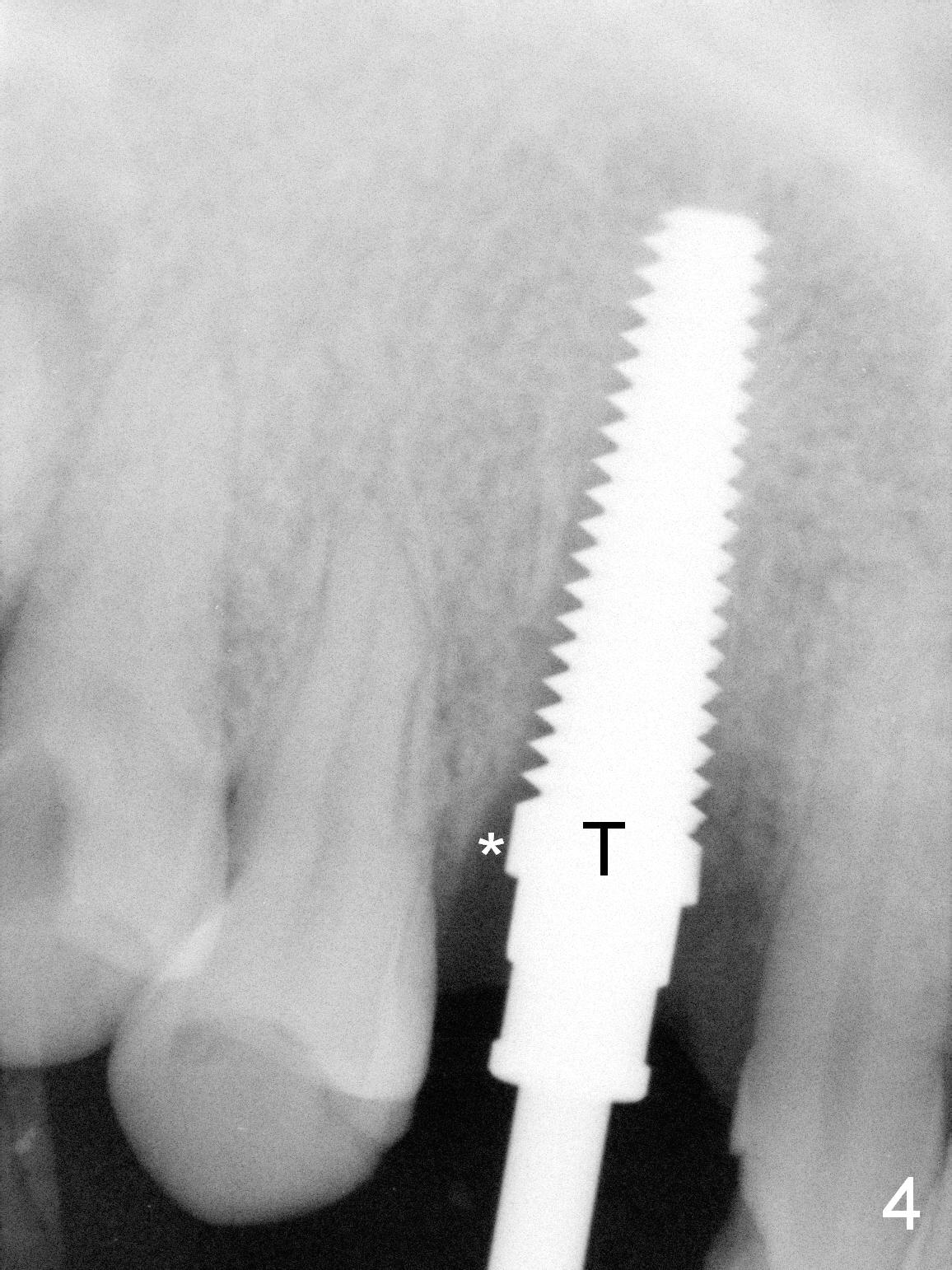
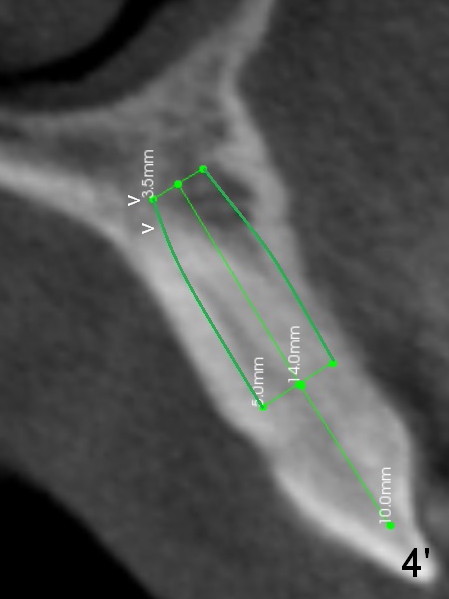
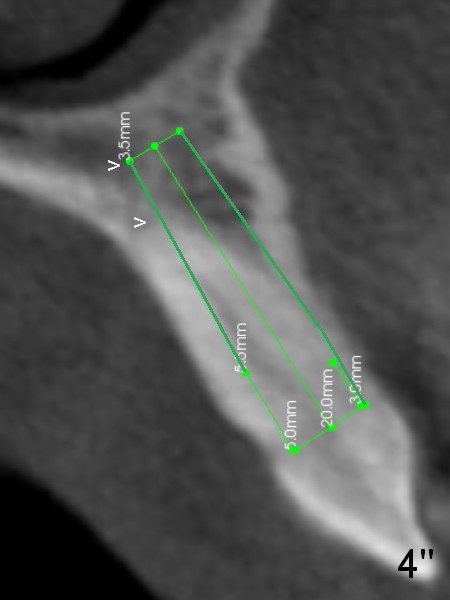
Lengthwise, a longer osteotomy is needed (Fig.4): 20 mm at the gingival level, 17 mm at the bone level. Distal to the 5 mm tap is a gap (*). Initially a shorter osteotomy (by 3 mm) is made: there is minimal engagement with the labial bone (Fig.4' between arrowheads (CT coronal section from not the same patient)). The osteotomy is extended (Fig.4''). This is the second problem to be solved.
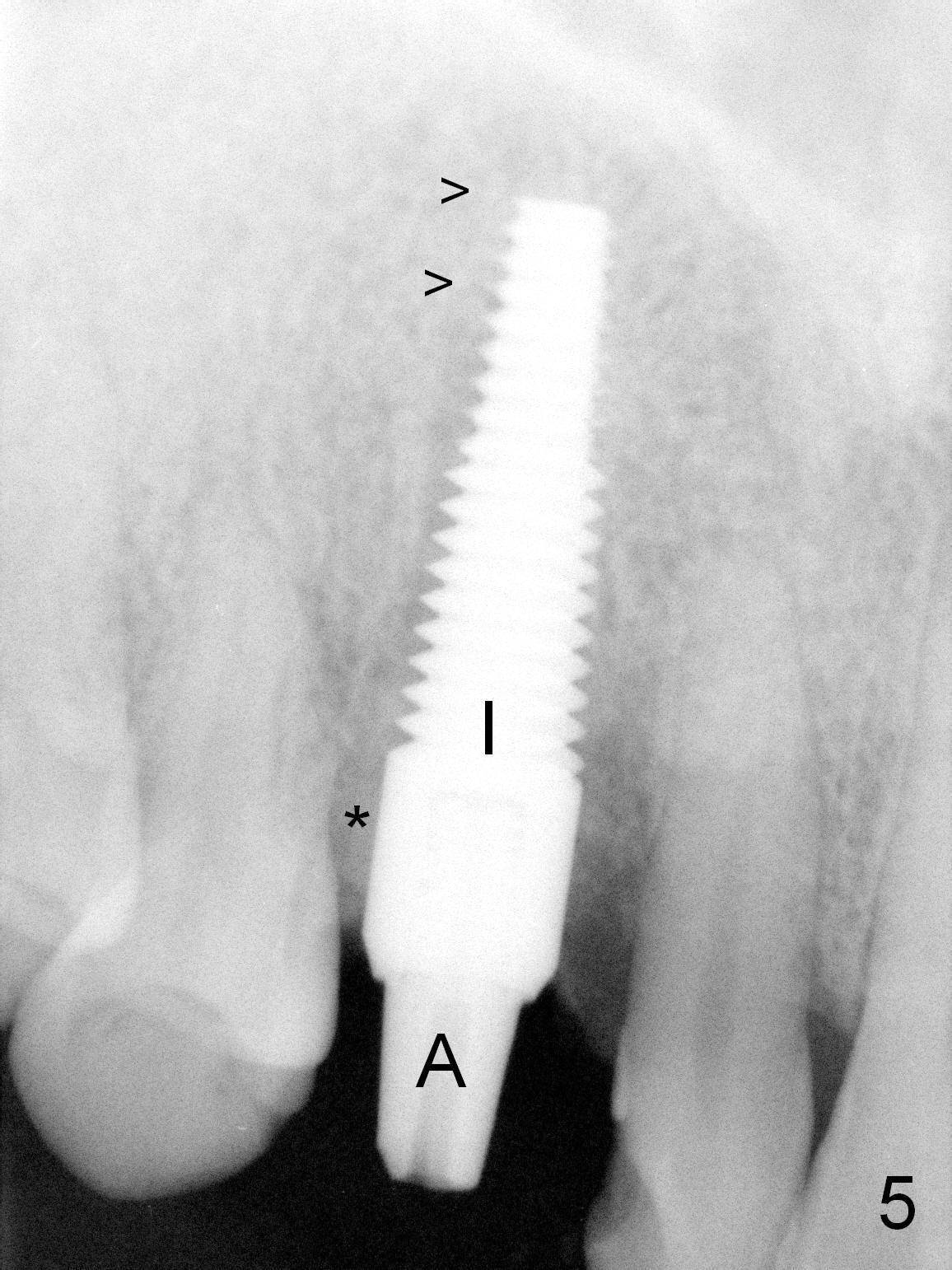
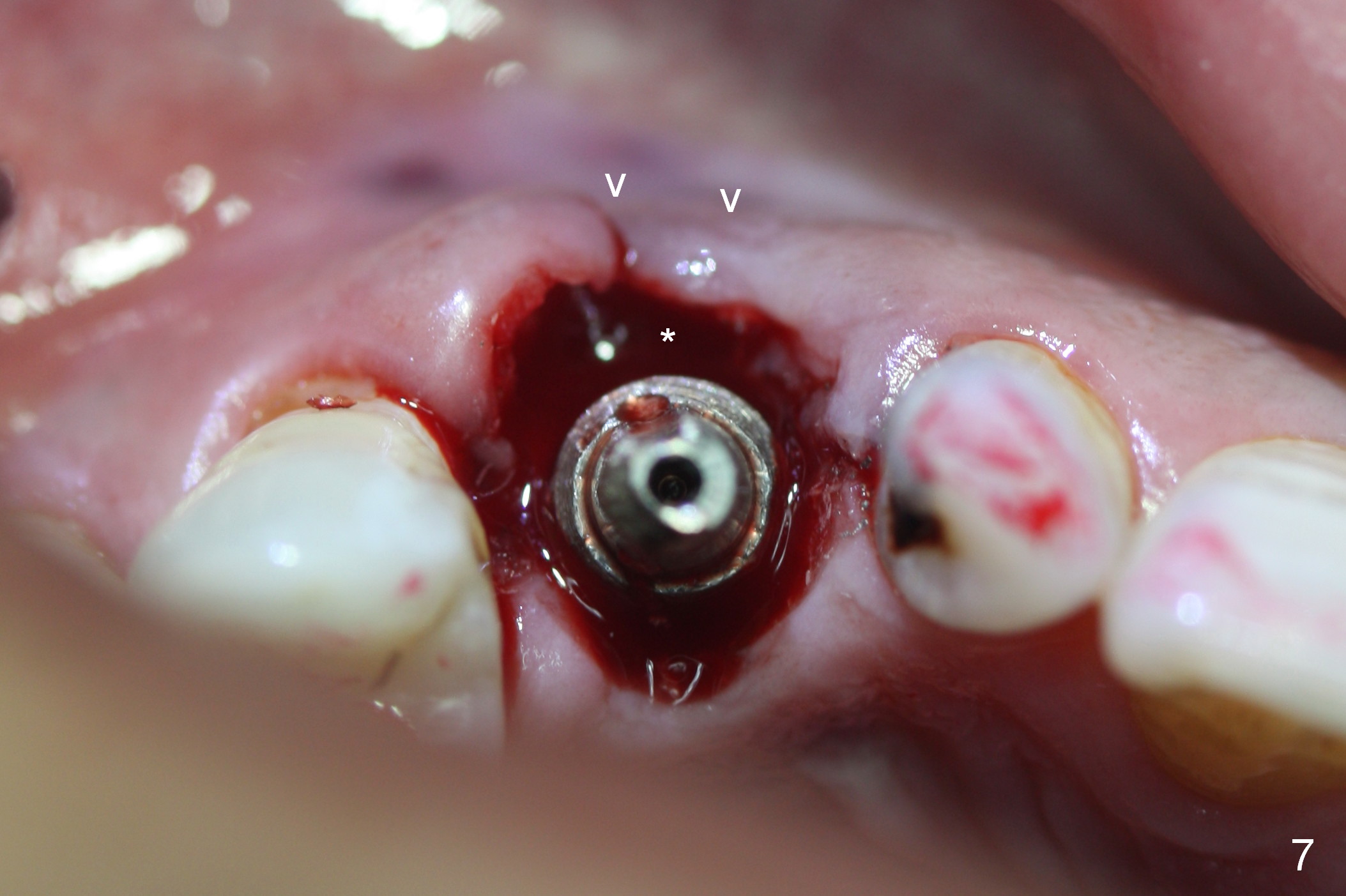
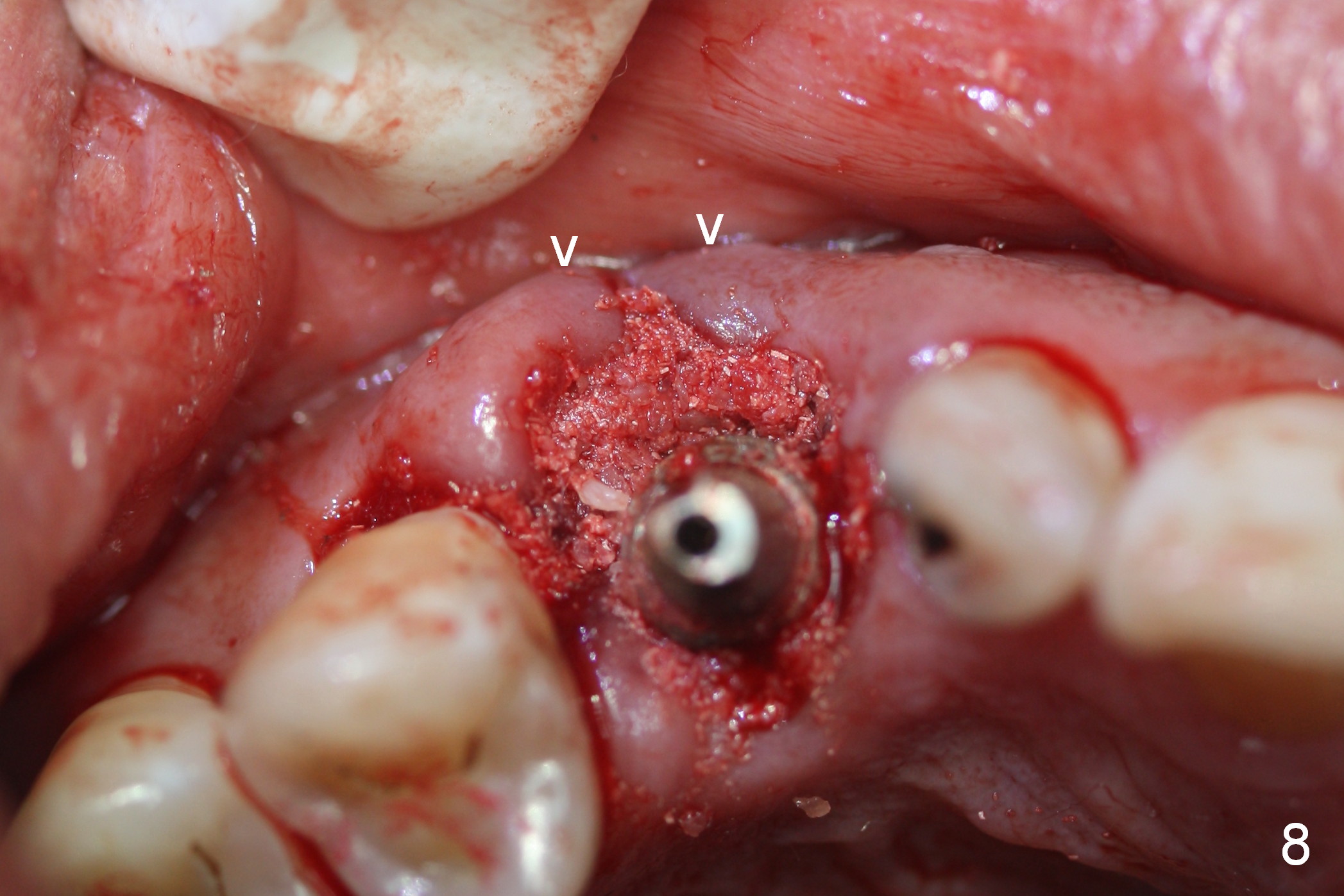
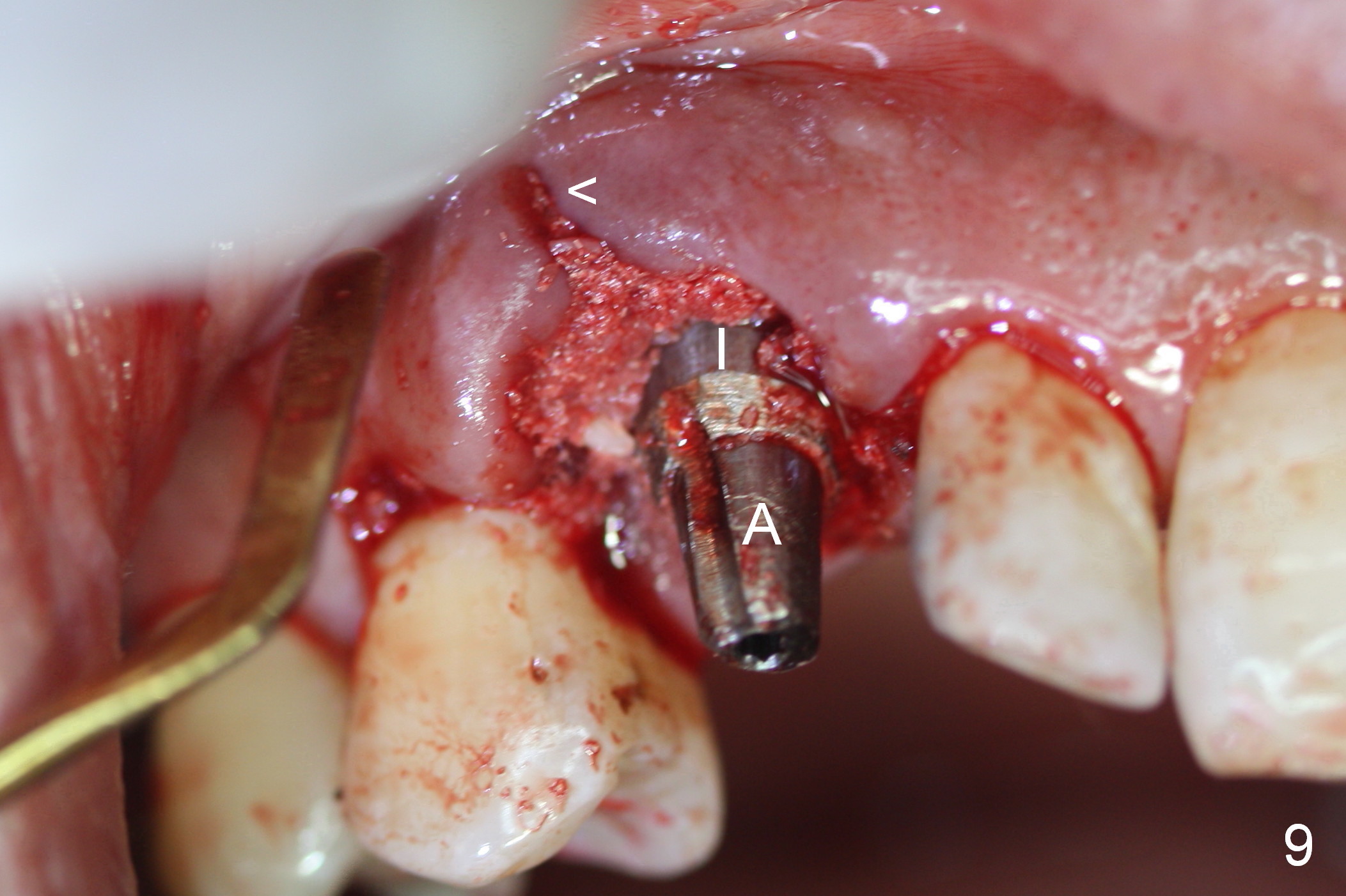
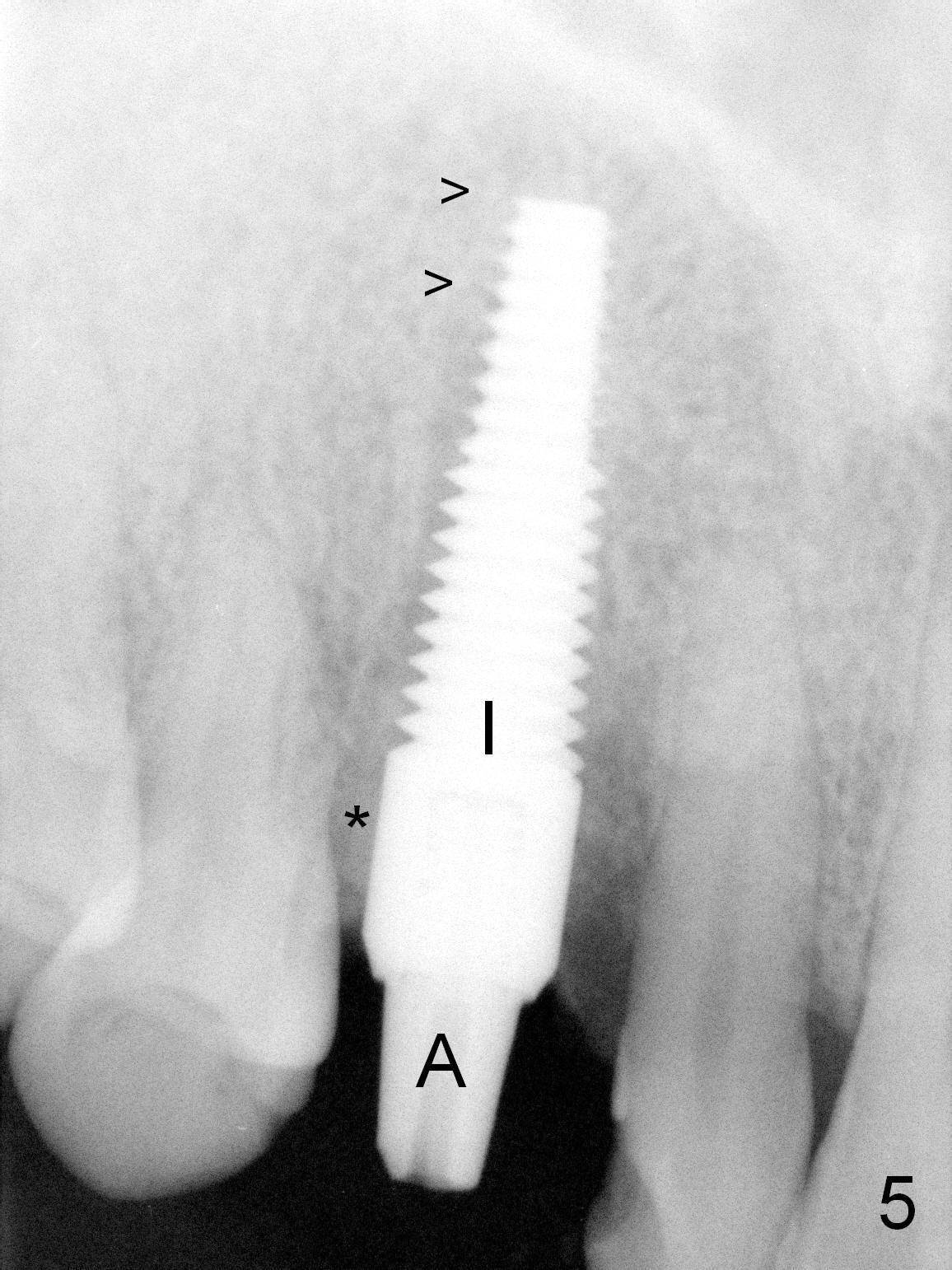
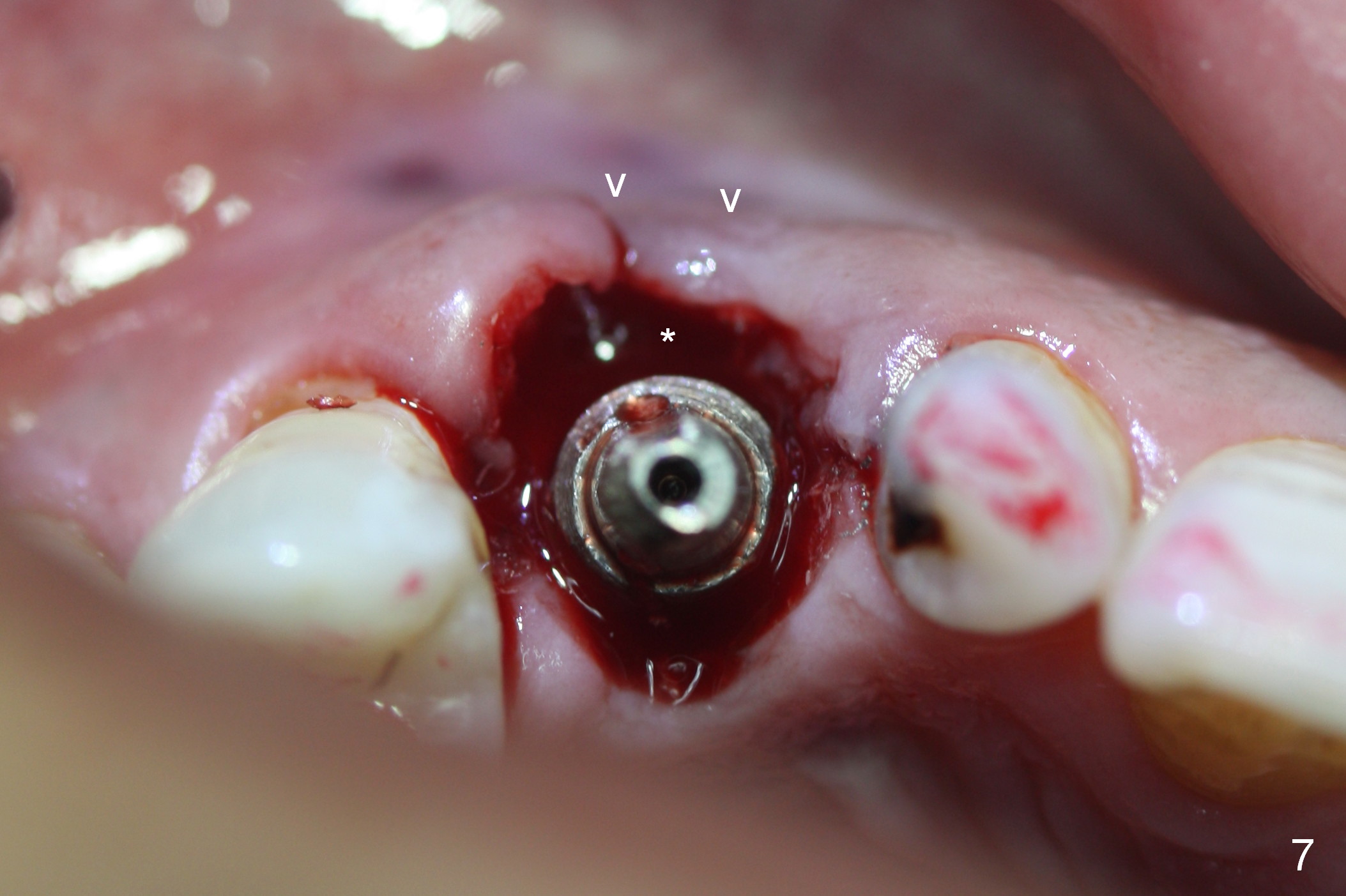
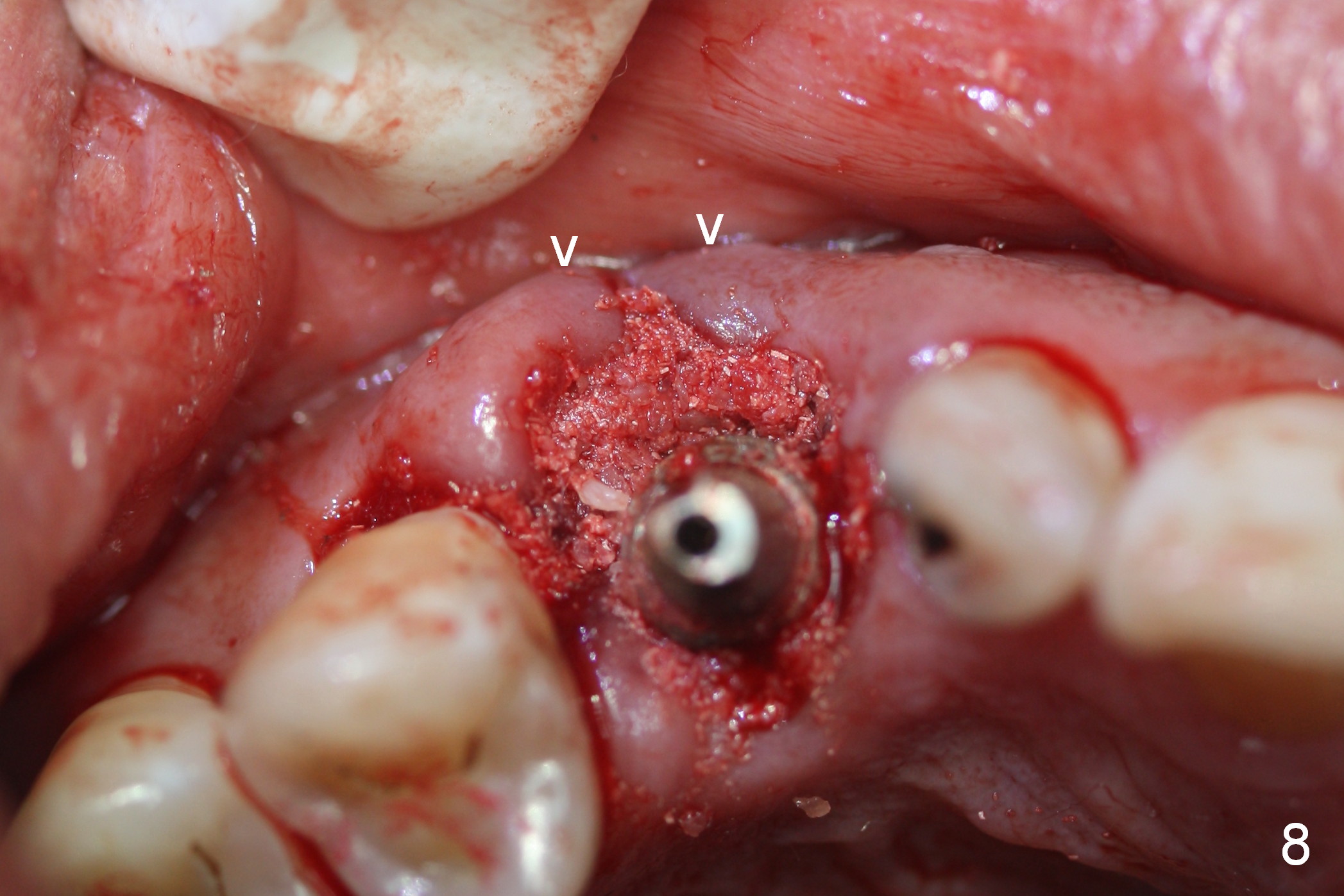
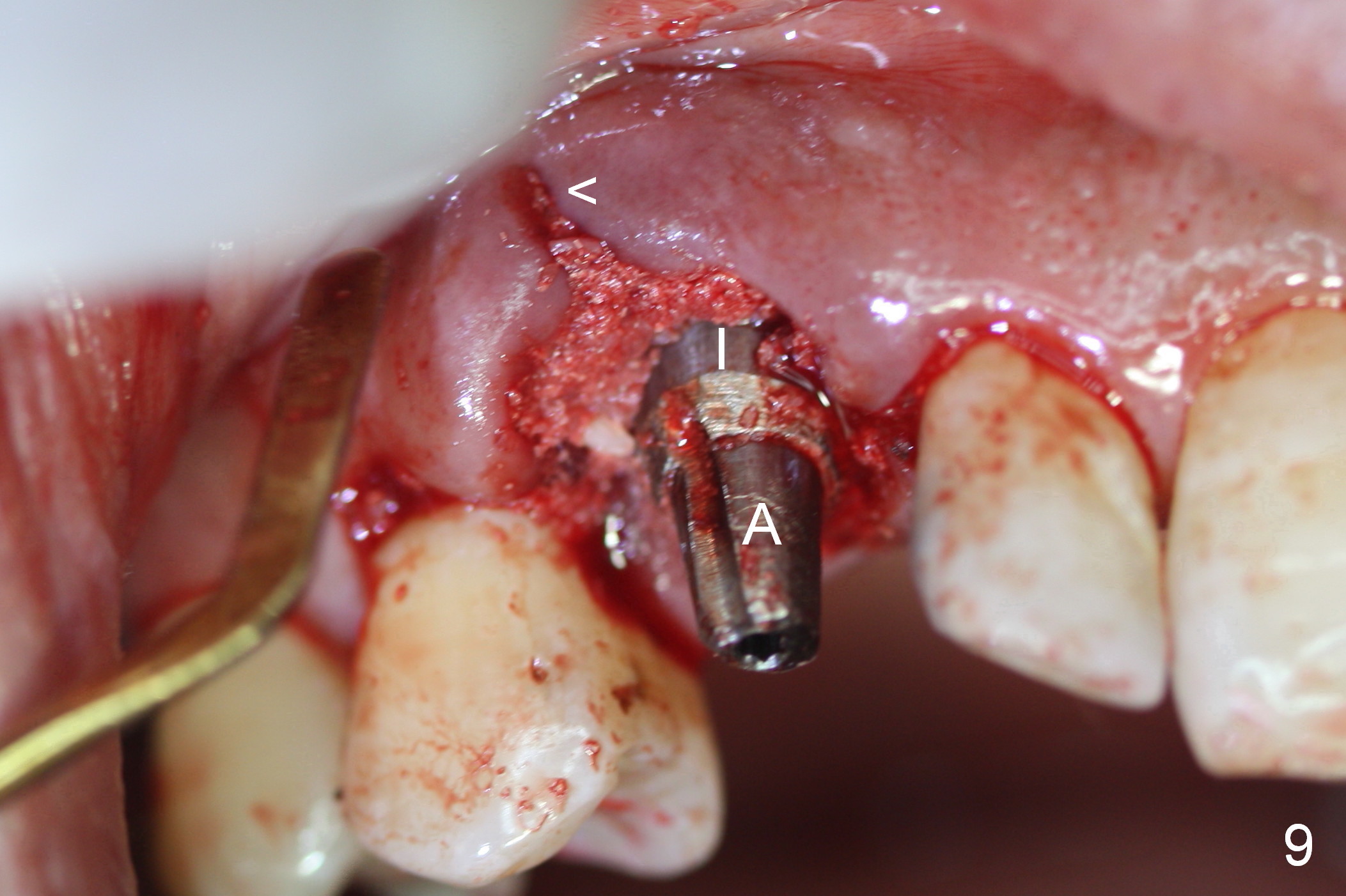
After 5x20 mm implant is placed, the distal gap is filled with bone graft (Fig.5 *). An abutment is placed (A) for fabrication of an immediate provisional (Fig.6 P). The latter hold the labial gingiva bulging (Fig.6 >). When the provisional is removed for bone grafting, the labial gingiva collapses (Fig.7 arrowheads). In fact a piece of cone-shaped Osteotape (Impladent) is placed palatal to the labial gingiva/thin labial plate and a small amount of graft is placed in the deepest area of the socket (labial to the osteotomy) prior to placement of the implant. More graft is placed in the peri-implant gap, particularly labially to keep the labial gingiva convex (Fig.8 arrowheads). The lacerated gingiva is to be approximated with perio glue (Fig.9 <). Collagen dressing is placed over the exposed graft before cementation of the provisional. Perio dressing is applied for further protection and seal.
The perio dressing has been dislodged with exposure of the collagen dressing (Fig.10 *) 13 days postop. The graft appears to have consolidated or dislodged since the buccal plate collapses (Fig.11 arrowheads) to the status prior to grafting (as compared to Fig.7).
The patient returns 1.5 months postop. The provisional margin is much higher than that of the neighboring teeth (Fig.12,13: #6), unlike the opposite side (Fig.12: #11). When the provisional is removed, the implant margin is at the same level as that of the neighboring teeth (Fig.14 arrowheads). The implant margin is slightly extended apically (Fig.15 ^) prior to seating of the modified provisional. When the provisional is seated, its margin (Fig.16 ^) is at the implant margin; the gingival margin (*) is free and expected to move coronally by itself.
One and a half months later (3 months postop), the patient returns for final crown impression. The buccal gingiva has grown coronally (Fig.17 arrow). The implant appears to have osteointegrated (Fig.18). The buccal plate has become concave (Fig.19 arrowheads). To maintain the gingival level, the buccal portion of the implant/abutment (Fig.19 *) is going to be reduced (Fig.20 *). The margin of the definitive restoration will be at the prep margin and thin so that the gingiva is expected to continue to be growing coronally after cementation.
To be improved: 1. Implant could be placed more palatal; 2. Gingival laceration should have been sutured prior to bone grafting; 3. The buccal margin of the provisional should have been extended more buccally to prevent bone graft from dislodgement; the provisional should be relined and recemented securely; 4. More rigid membrane should have been used to keep convexity of the buccal plate. The crestal bone is stable 3 Years 7 Months Post Cementation (Fig.21). The buccal plate is slightly atrophic 3 Years 7 Months Post Cementation (Fig.22).
Return to Upper
Canine Immediate Implant
30
Xin Wei, DDS, PhD, MS 1st edition 05/17/2015, last revision 02/16/2020