






 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
|
 |
 |
||
Immediate Provisional May be a Must for a Posterior Tooth
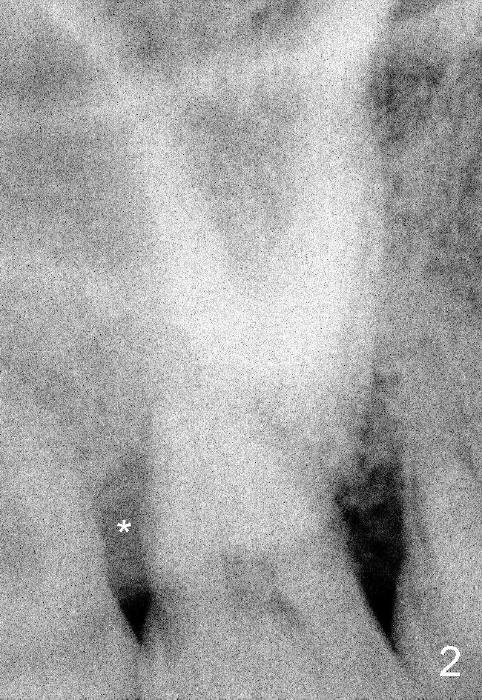
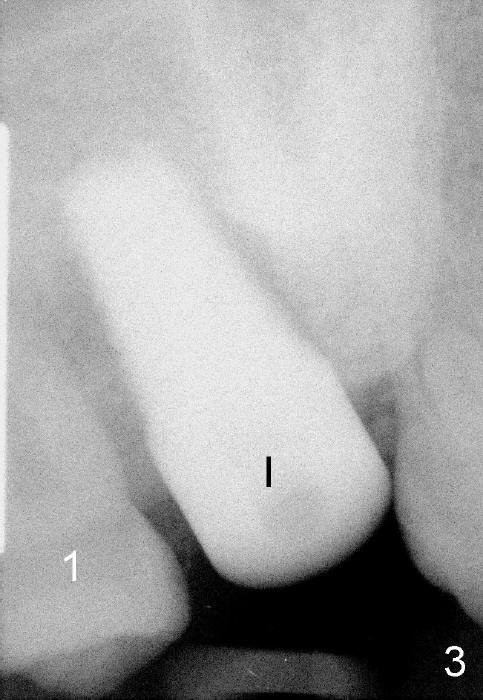
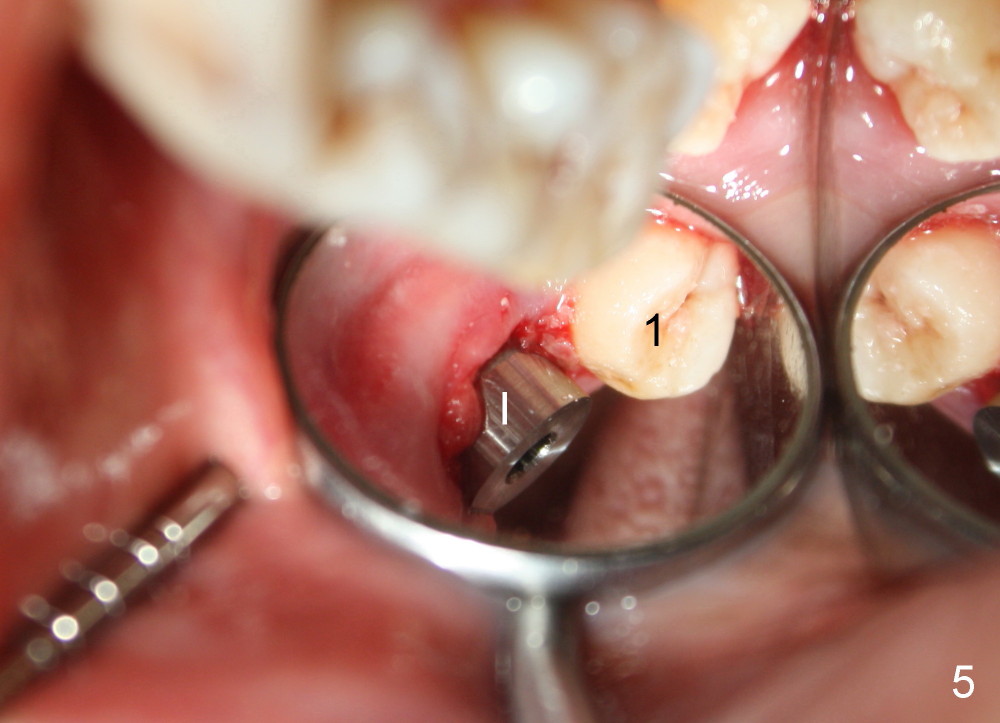
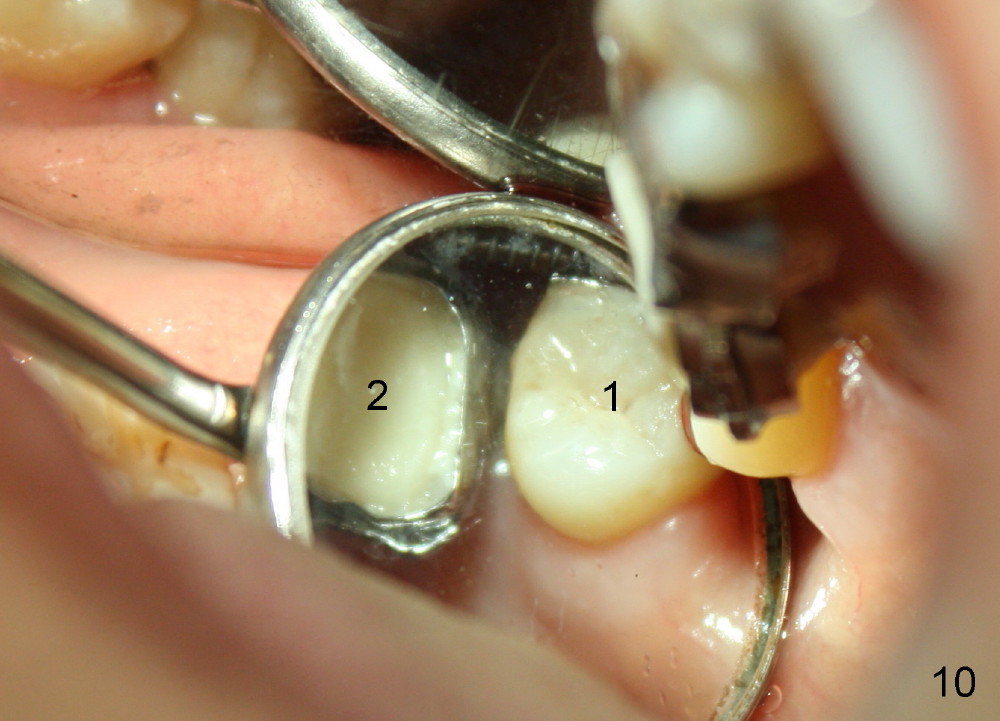
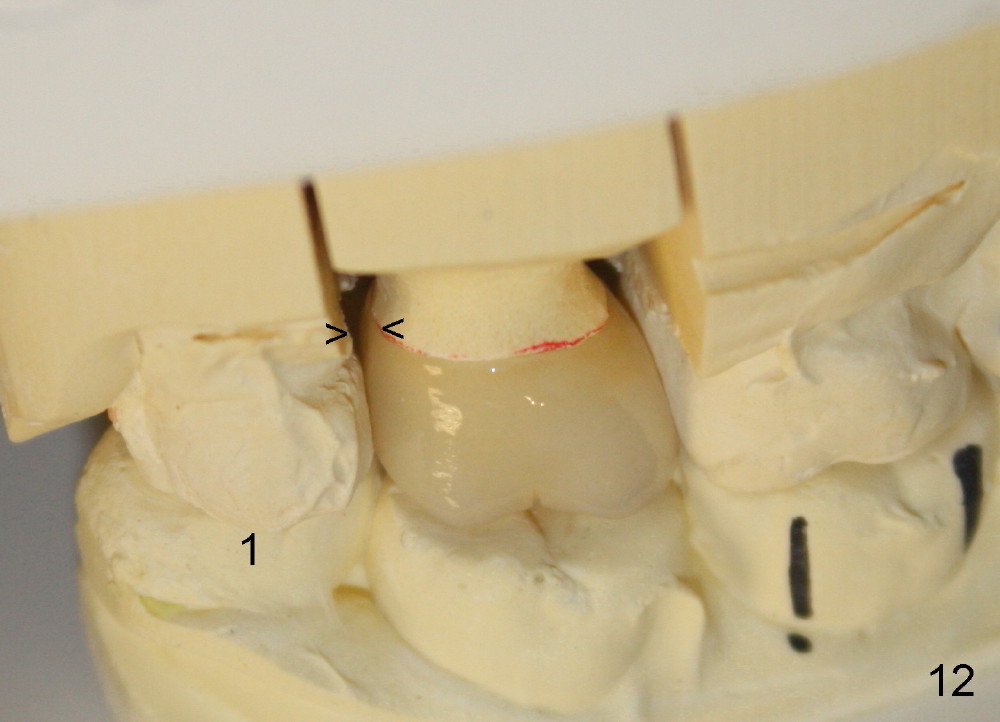
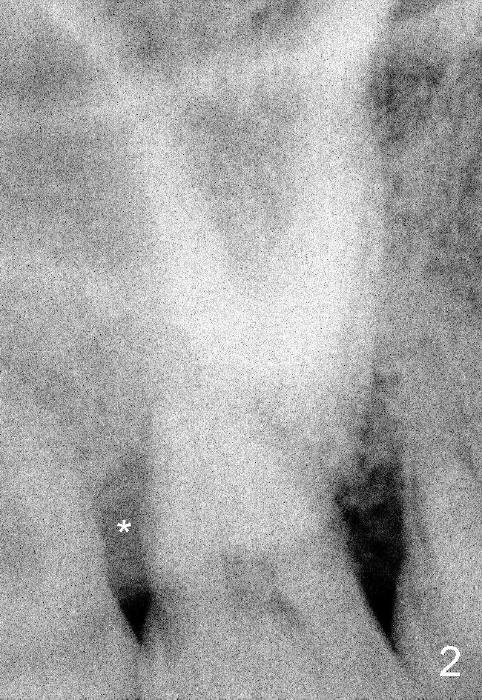
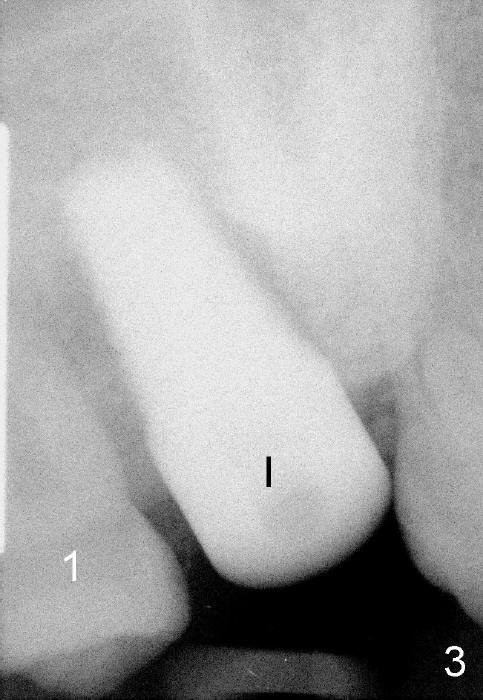
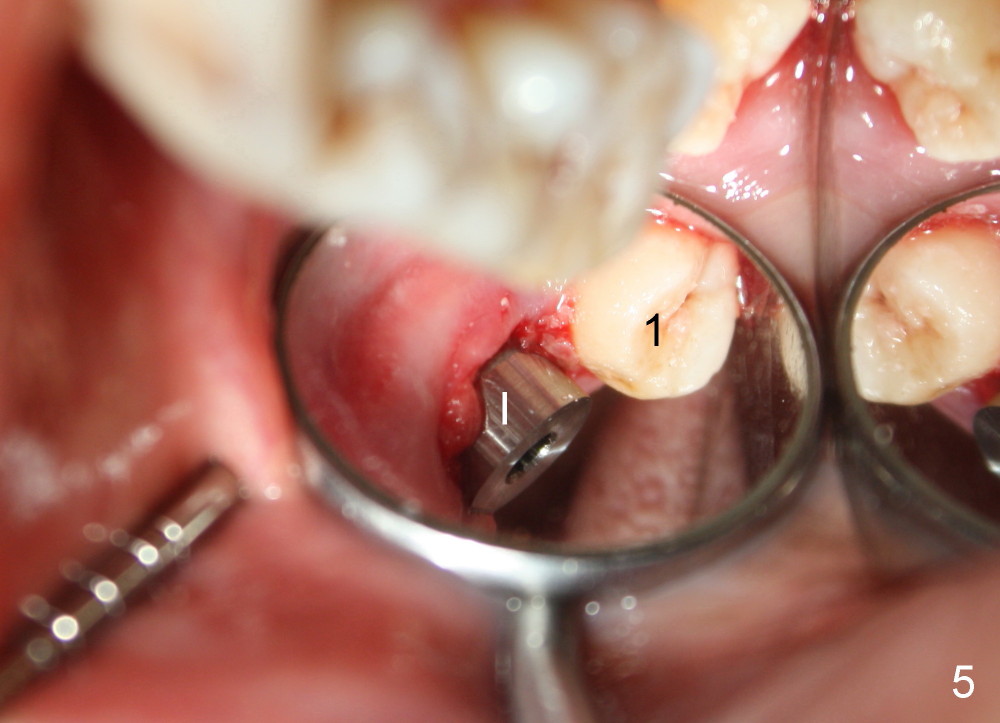
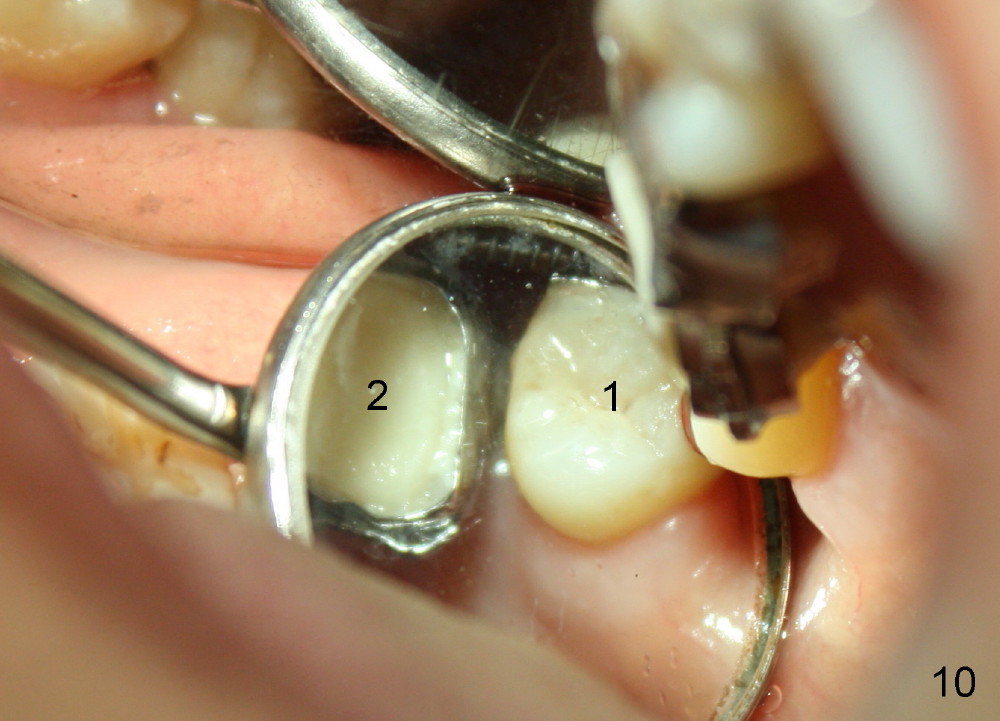
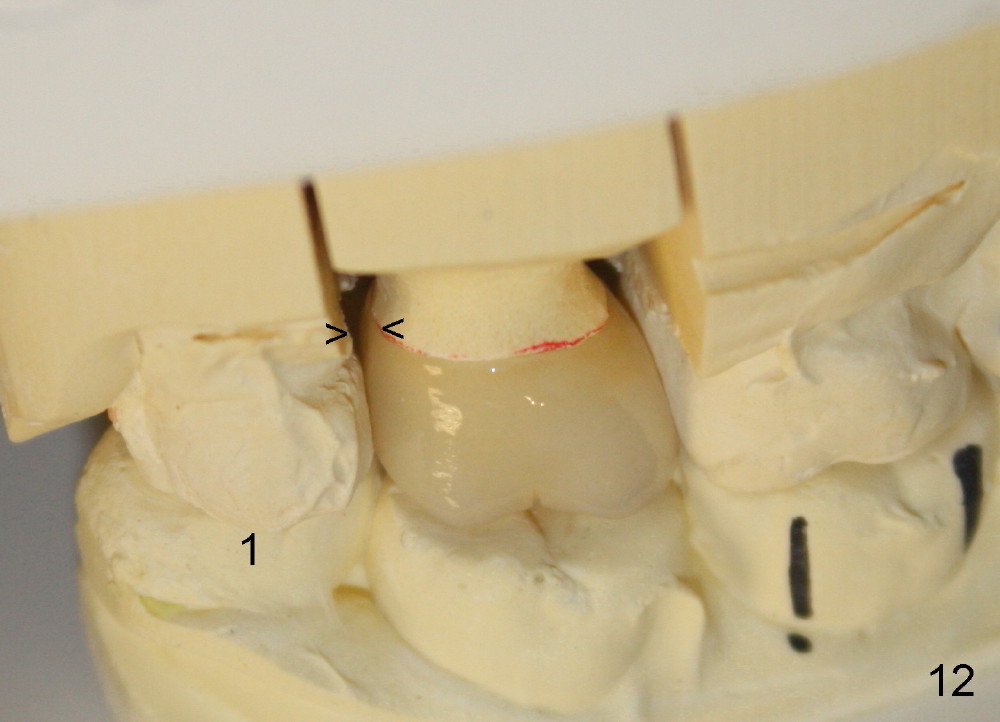
A 48-year-old lady is a dental phobic and has generalized chronic periodontitis. Bone loss around the tooth #2 has been severe for the last 5 years (Fig.1,2 *). Finally she agrees to have #2 (symptomatic) extracted and immediate implant placed (Fig.3 I). A 7x17 mm implant has to be used to achieve primary stability. The remaining buccal and lingual gaps are filled with allograft and membrane (Fig.4 *). Fig.5 shows that there is a space between the tooth #1 (asymptomatic) and the immediate implant (I). The wound/socket is protected by applying perio dressing around an abutment (Fig.6 A). Postop the patient is pain free; the perio dressing dislodges by itself. She returns 3.5 months later for restoration; but the tooth #1 has shifted mesially (Fig.6 arrow). The patient is not so willing to have #1 removed. Bands and bracket are placed in the neighboring teeth including a provisional crown to move the shifted tooth (with mobility) distally (Fig.7,9). The 2nd reason for #1 shifting is abnormal occlsual scheme on the right posterior region (Fig.8); mobility of #1 is the 1st one. The 3rd one is probably bruxism. In 5-6 weeks, the tooth #1 has moved to a desirable position (Fig.10, as compared to Fig.3,5). There is enough space for restoration (Fig.11,12).
In all, posterior immediate provisional should have normal proximal contact so that the neighboring periodontally affected teeth do not shift while the implant is osteointegrating. In order to avoid fibrointegration, the occlusal contact should be off. The patient requests an immediate provisional for the next implant. The same restoration will be fabricated for an implant at a healed site.
Return to Upper Molar
Immediate Implant,
Posterior Immediate Provisional
Xin Wei, DDS, PhD, MS 1st edition 09/28/2014, last revision 01/19/2018