 |
 |
 |
 |
 |
 |
 |
 |
||
 |
 |
 |
||
Place Implant in the Septum Between Sinus and Nasal Cavity
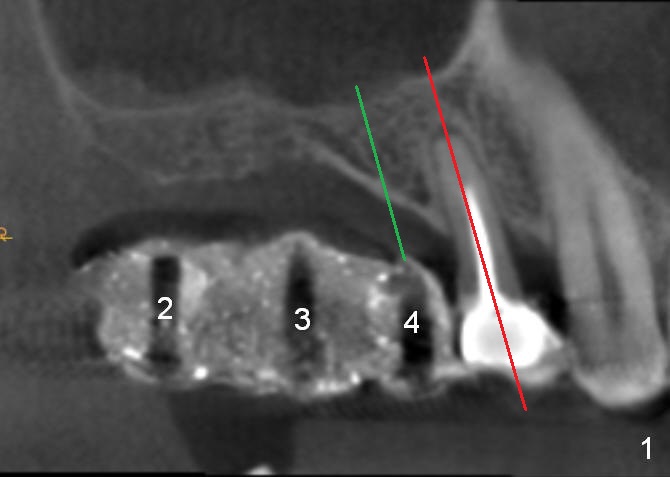
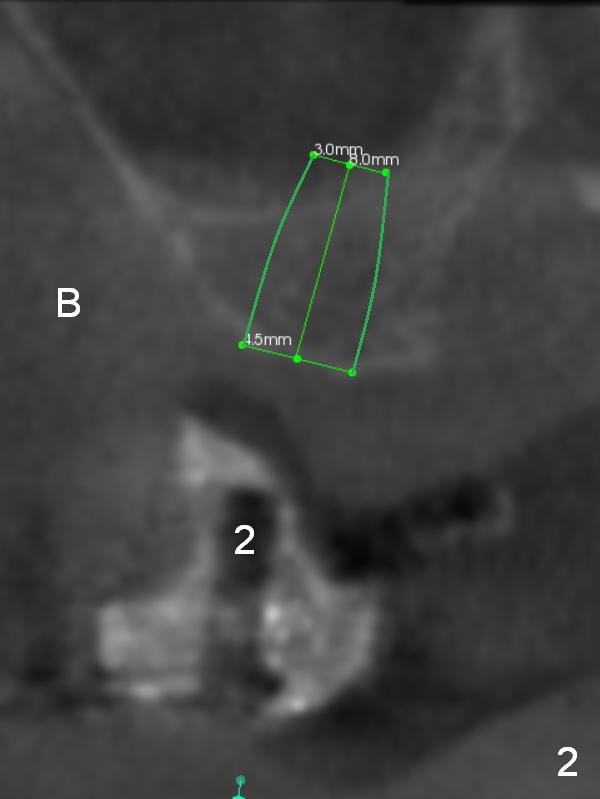
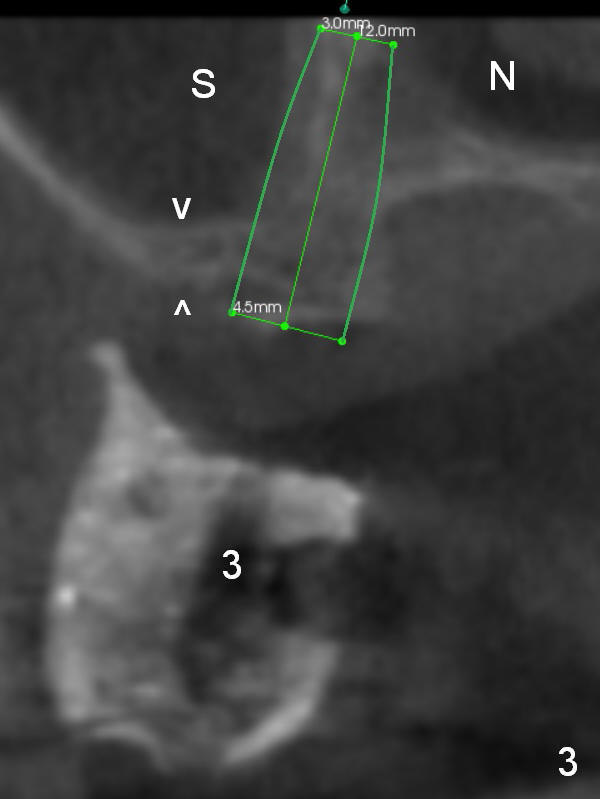
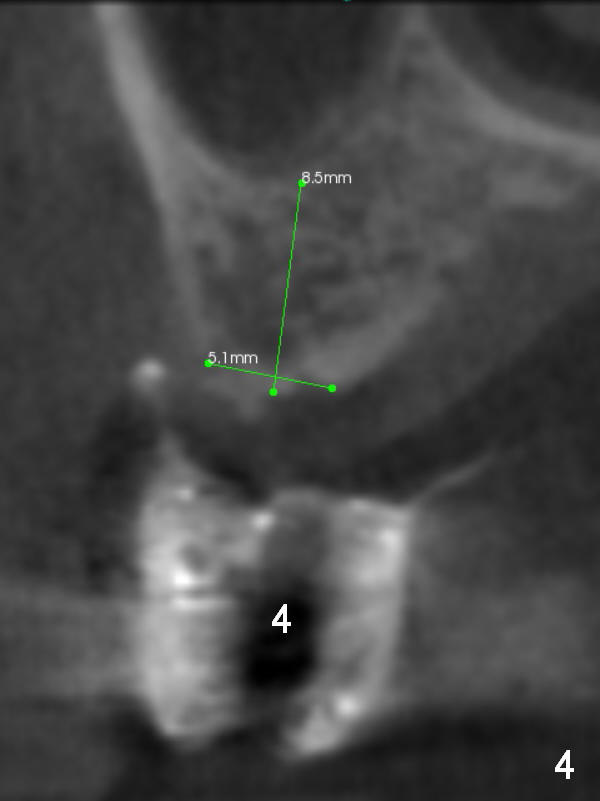
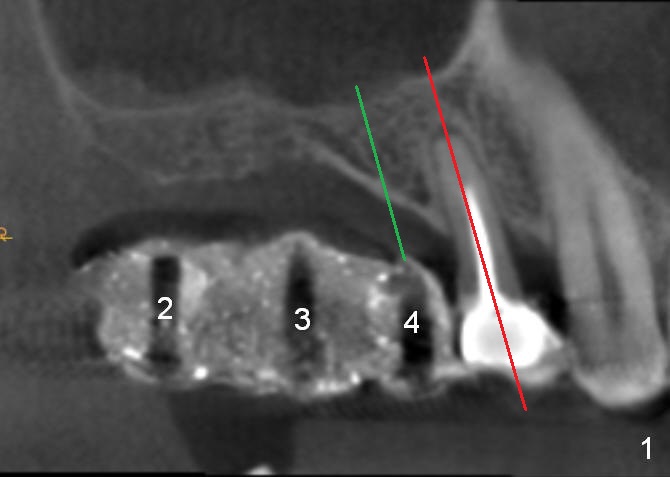
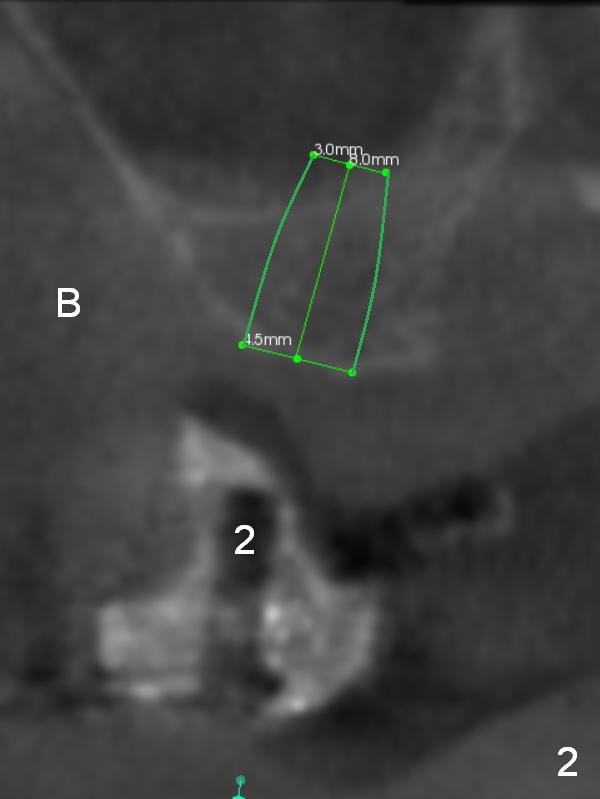
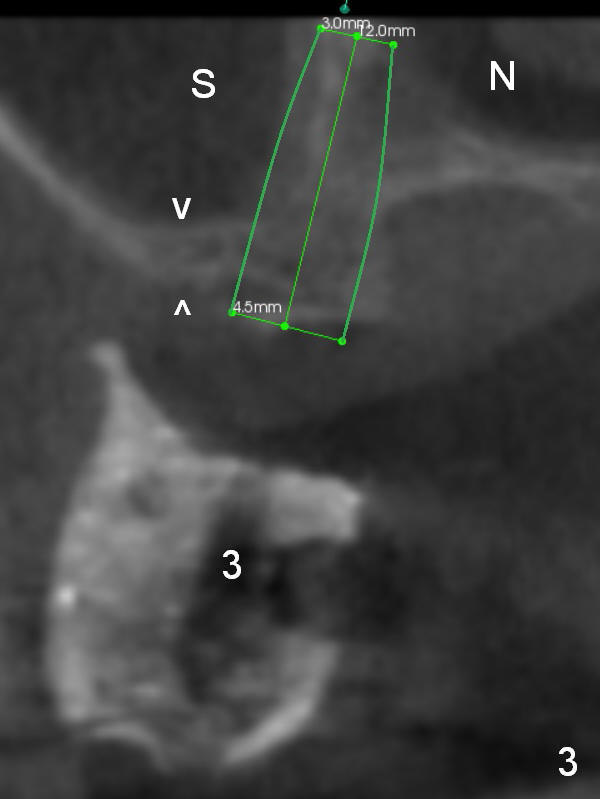
As mentioned earlier, the 56-year-old man is taking Plavix, one tablet every other day. The last time he took the medication is 4 days ago. For hemostasis, three carpules of 2% Xylocaine with 1:50,000 Epinephrine are administered in infiltration. Initial osteotomies are established through the CT scan stent (Fig.1-4: #2-4). Then an incision is made. After raising the flap, the osteotomy sites are checked. Ridge split is made between these sites with a chisel without much success. Bone is soft between #2 and 3. Sinus lift (Fig.2,4) is attempted at #2 and 4 (3.6 mm), whereas bone expansion is accomplished at #3, in the bone between the sinus (Fig.3 S) and the nasal cavity (N).
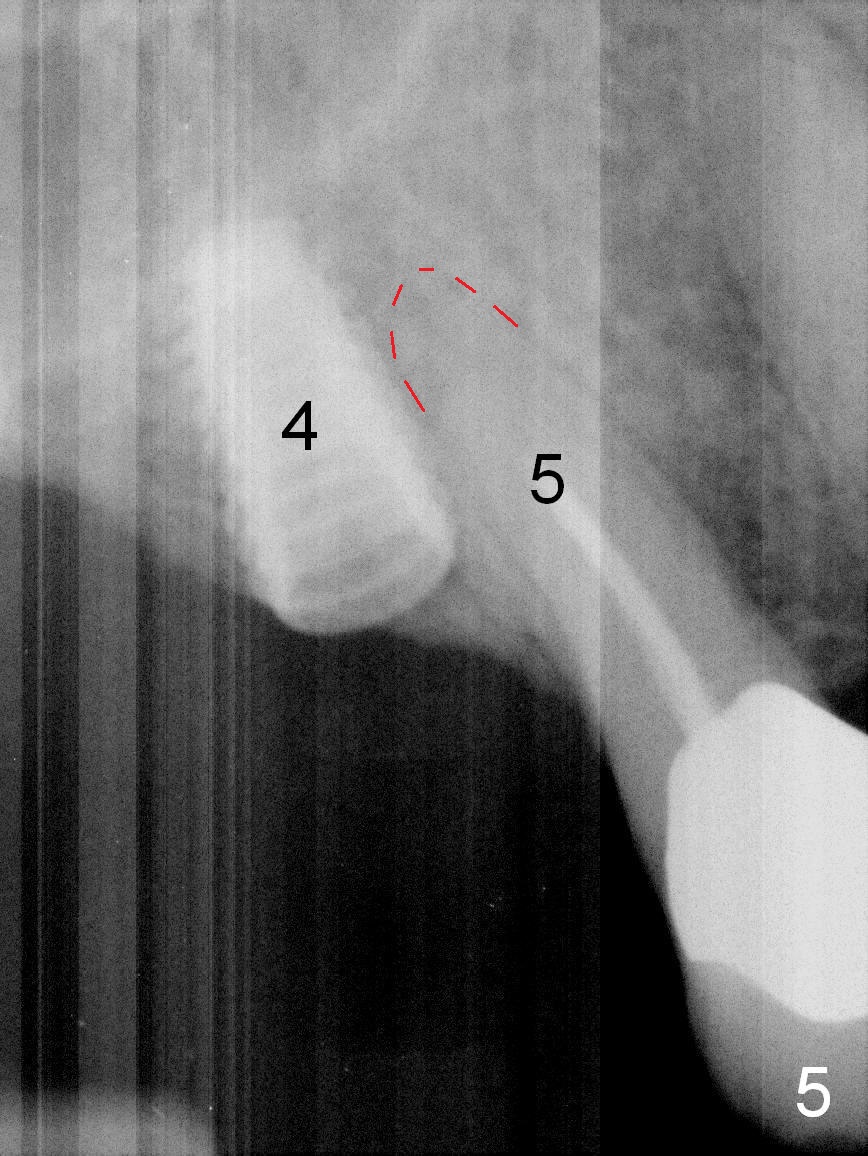
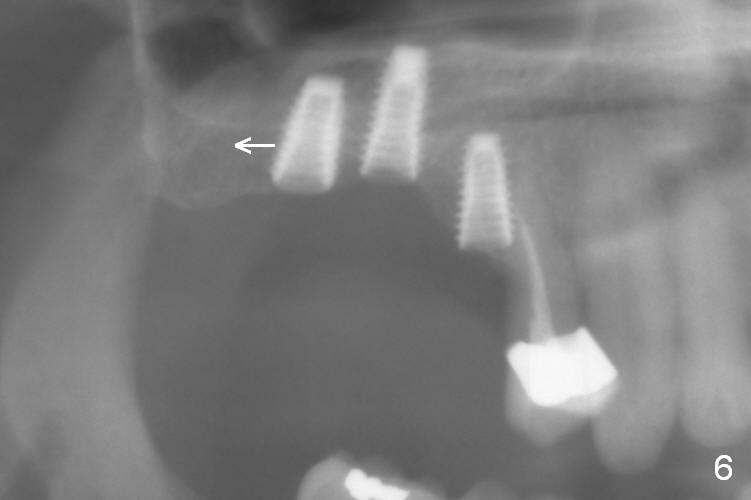
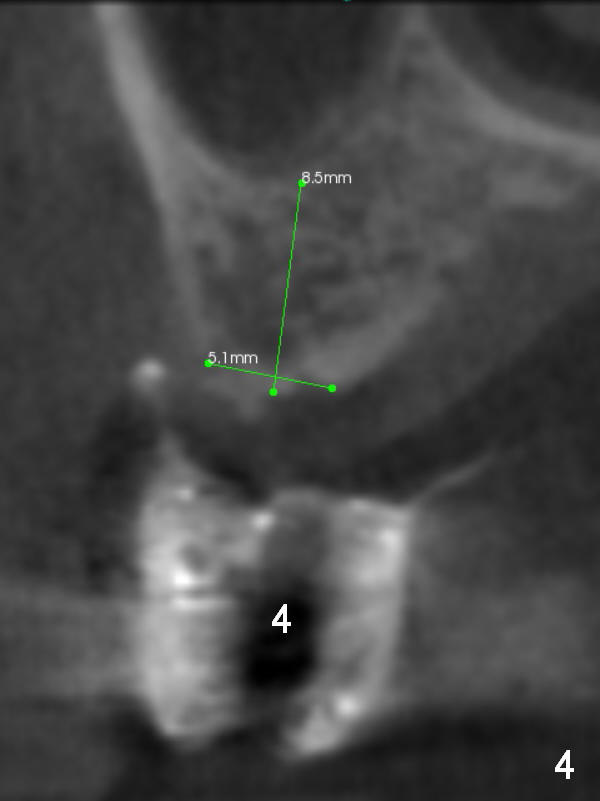
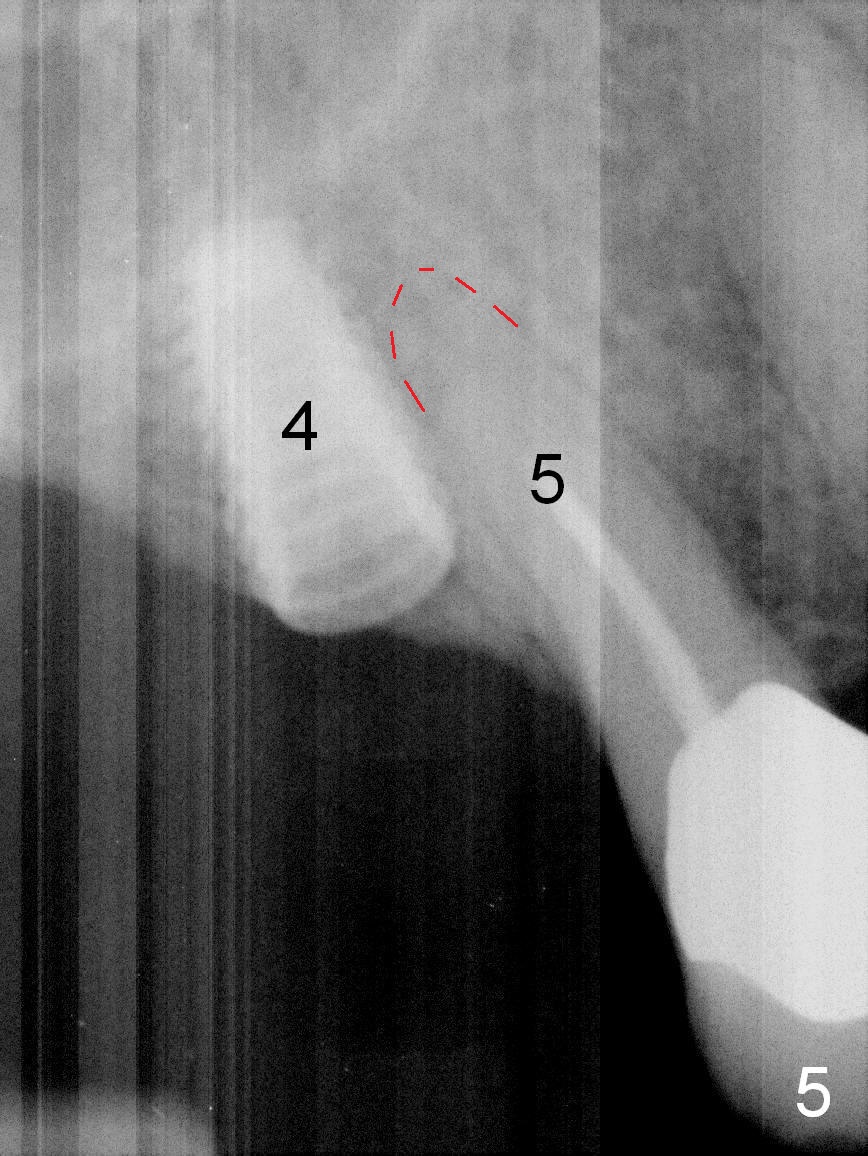
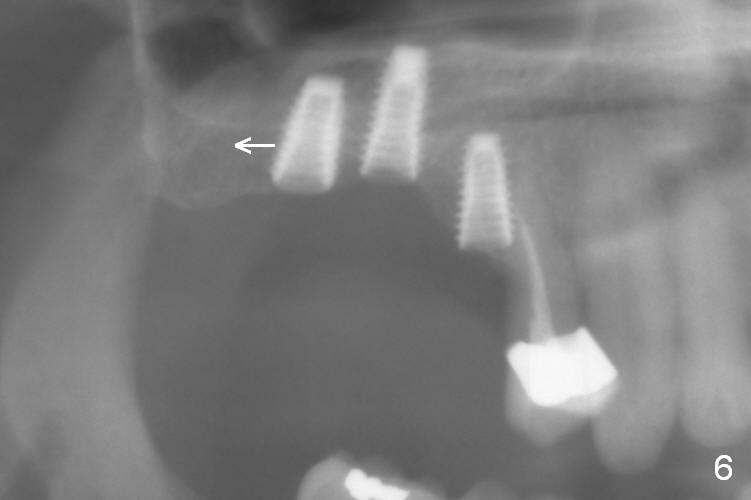
After use of 2.8 mm round bur at #4 for sinus lift, a 4x8.5 mm regular drill is used with resultant sinus membrane perforation at the sinus floor. The latter is repaired with insertion of Osteogen plug prior to place 4.5x8.5 mm implant (Fig.5,6). The similar mistake occurs at #3: after using 2.4/3.7 mm bone expander for 10 mm, a 4x10 mm is used, which also results in sinus perforation, probably sideway, buccally. Trimmed Osteogen plug is placed before a 4.5x10 mm implant is placed with primary stability (Fig.6). The reason for use of the regular drills is to avoid ridge fracture due to under prep.
Since the bone at #2 is soft, the 3.6 mm round drill is used after 2.8 mm one. When a 5x8.5 mm implant is placed, there is no ridge fracture. The implant at #2 should have been placed more distal (Fig.6 arrow).
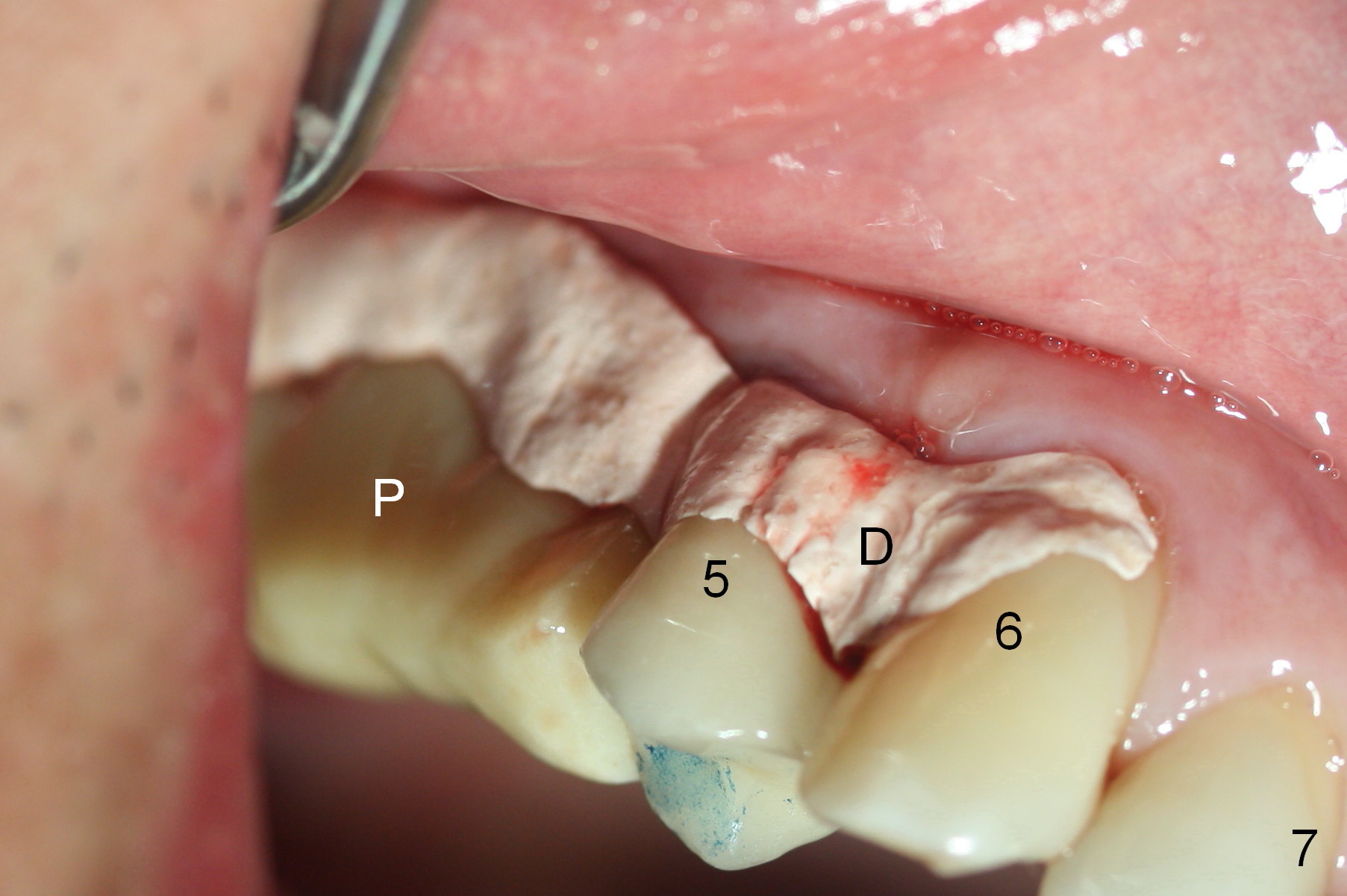
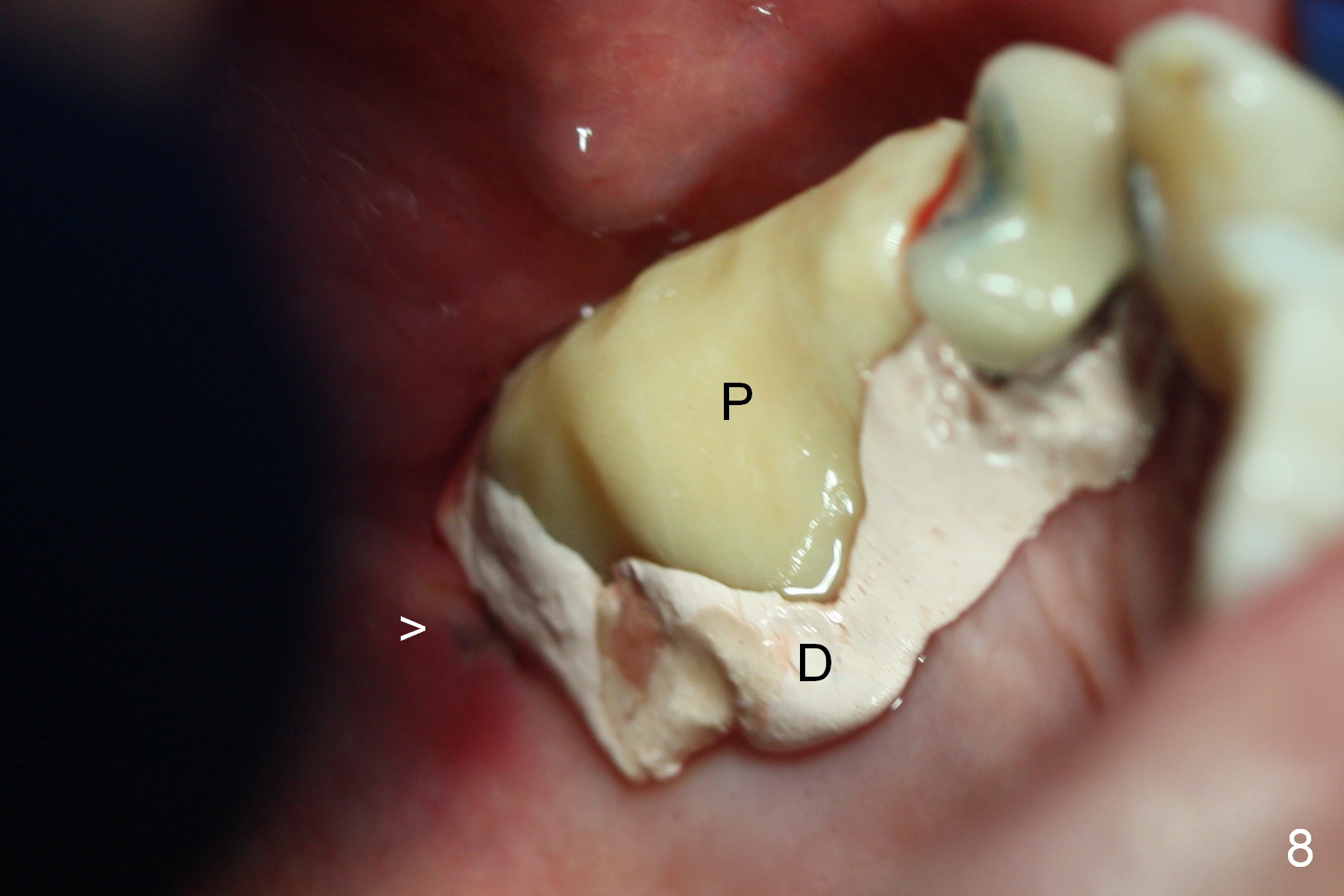
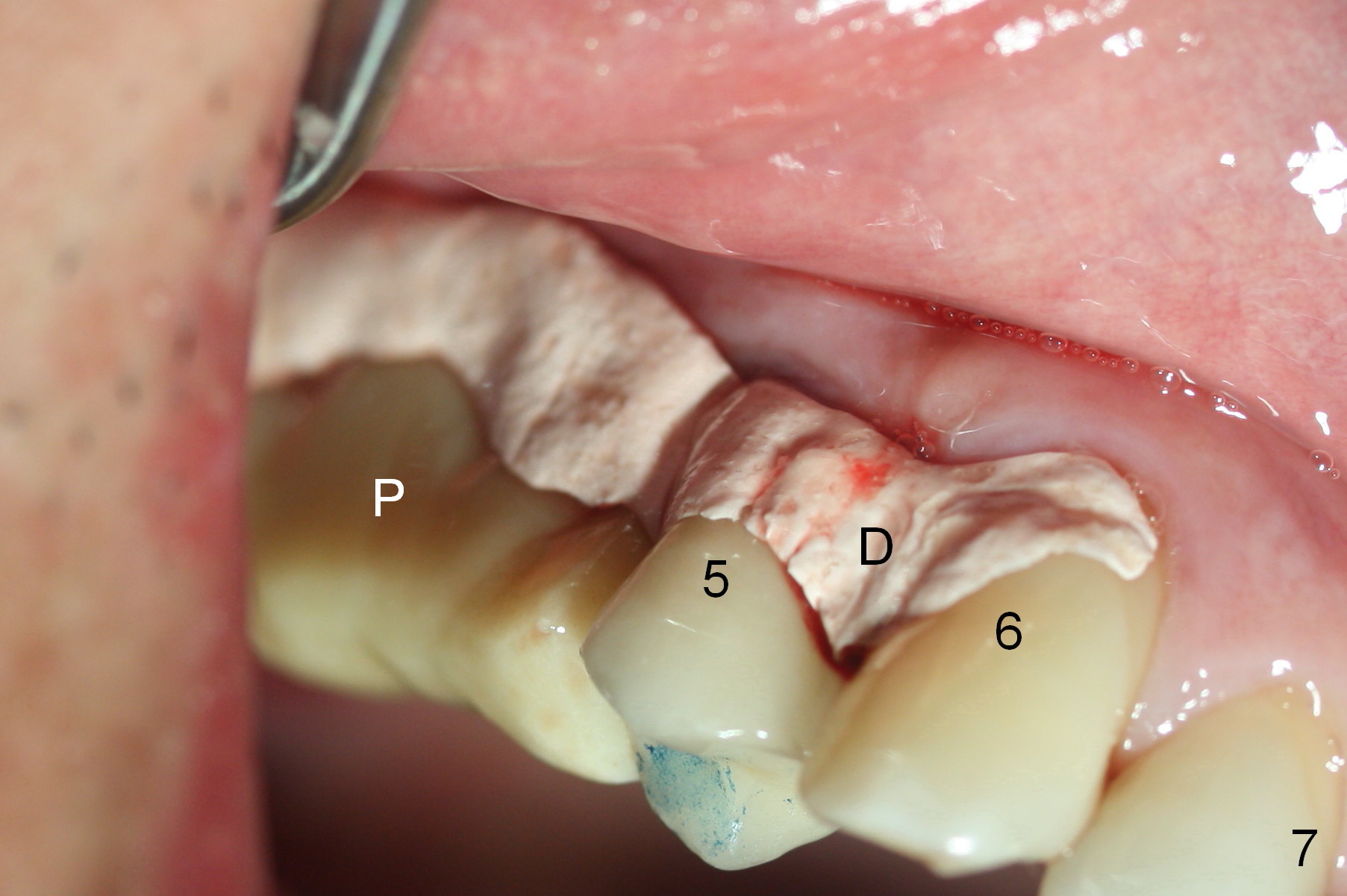
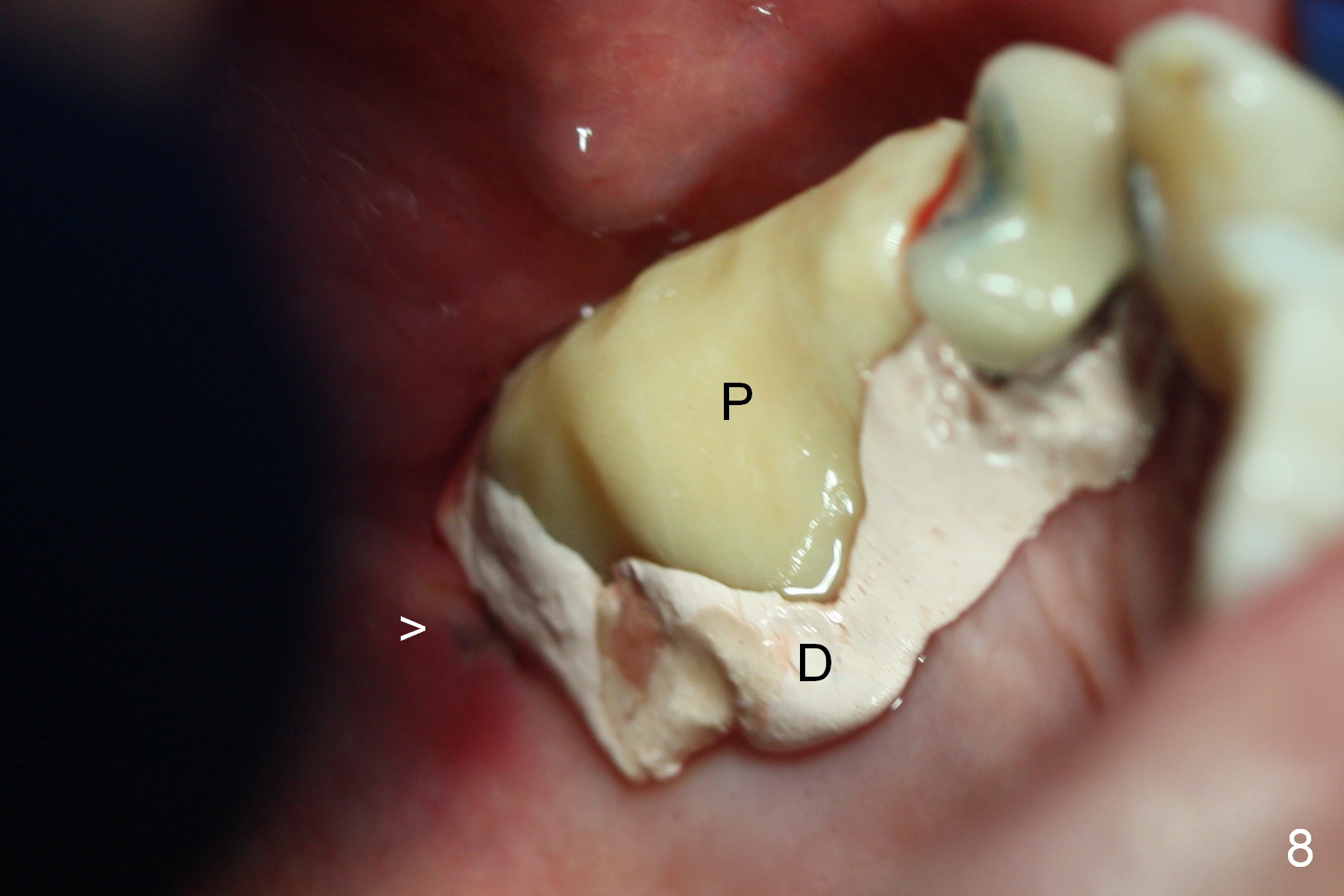
Insertion torque of the three implants is ~ 50 Ncm. Three long (because of severe vertical bone resorption (Fig.1,6)) abutments are placed immediately for immediate splinted provisional (Fig.7,8 P). The latter should have hemostatic effect. Application of peridontal dressing (D) has additional hemostatic function, exerting pressure the most anterior (Fig.7 between the teeth #5,6) and the most posterior (Fig.8 arrow) incision, where the provisional cannot. Sulcus incision is good to remove subgingival calculus. It seems that chronic periodontits and bruxism play roles in pathogenesis of bone loss.
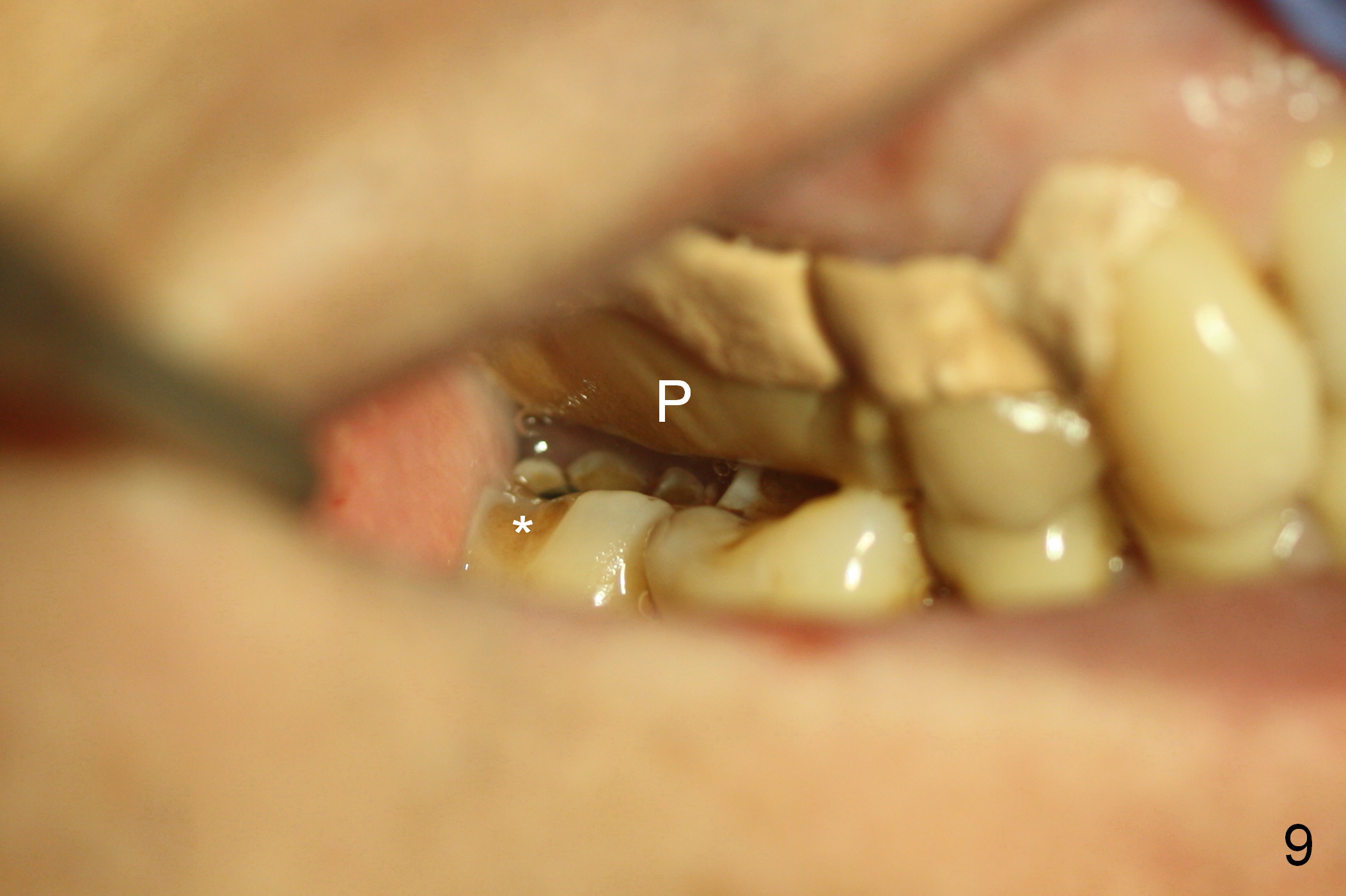
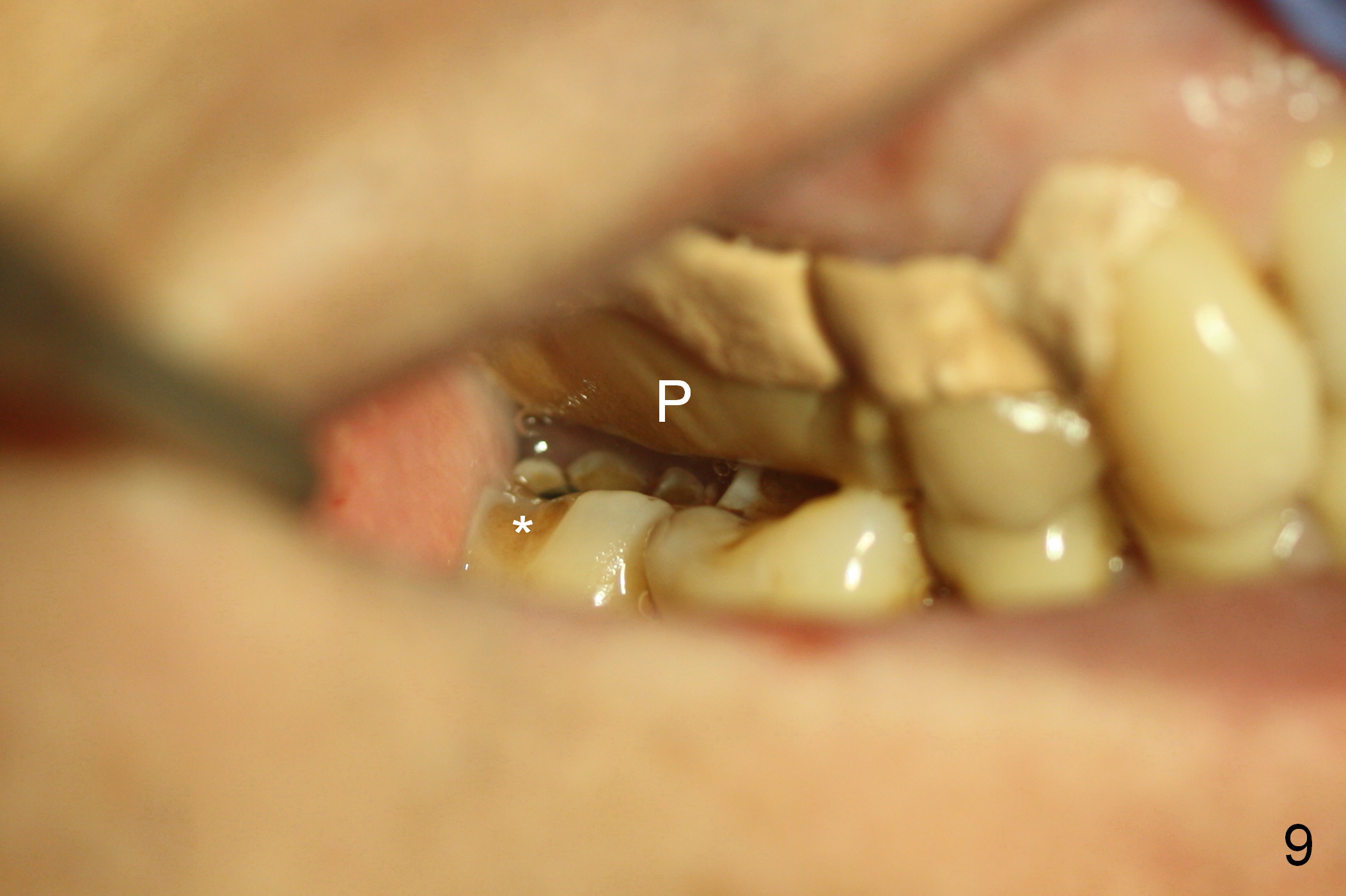
The patient returns for follow up 6 days postop. The periodontal dressing and the immediate provisional (Fig.9 P) remain in place. The provisional is off occlusion and seems to be in excessively cross bite. The wear facet in the buccal occlusal surface of the lower 2nd molar (Fig.9 *) appears to indicate that the former occlusion is normal, not cross bite. It is planned 2 months postop that the acrylic is to be added to the provisional to establish normal or cross bite prior to final impression.
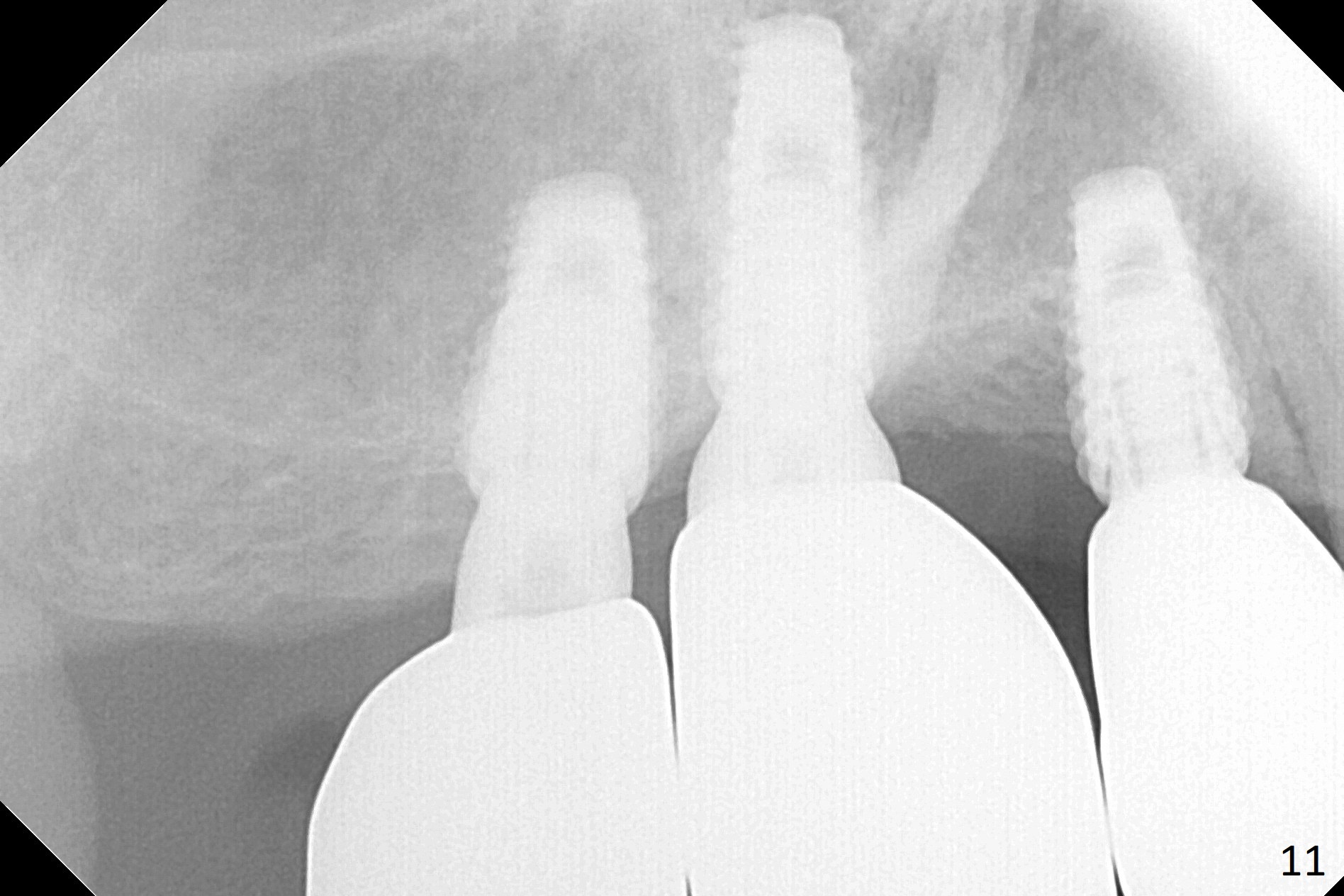
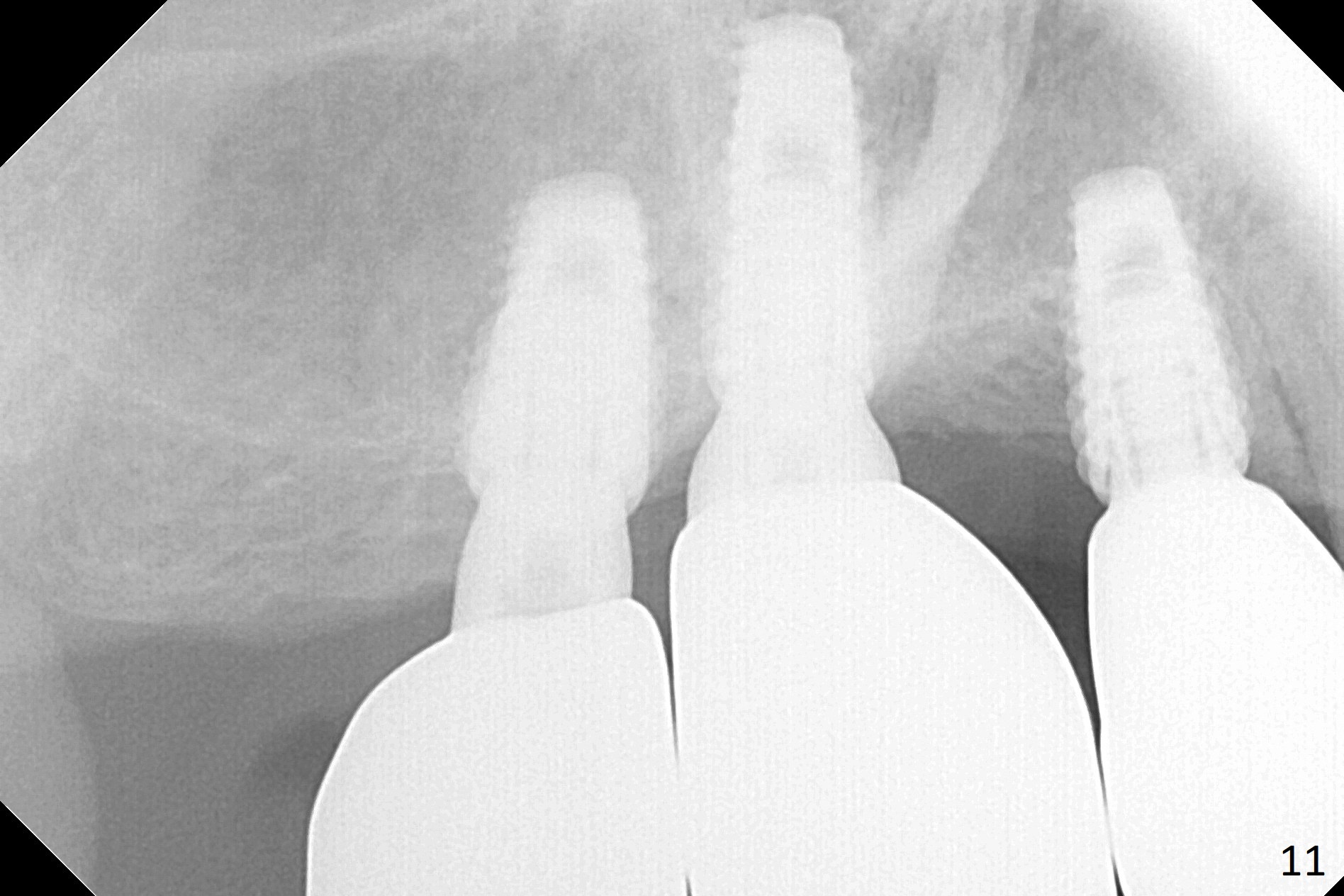
In fact, these implants seem to heal normally 2.5 months post (Fig.10). After change in abutments at #2 (from 5.5x7(4) to 4.5x5.5(5) mm) and #4 (from 5.5x7(2) to 4.5x5.5(1) mm) and torquing, impression is taken. The implant at #3 appears to be associated with the septal bone (Fig.10 *). There is no apparent bone loss 1 years 4 months post cementation (Fig.11). The patient will return for 14,15 implants.
Return to
Upper Arch Immediate Implant,
Posterior Immediate Provisional,
Professionals,
Berkeley
Anatomy
Xin Wei, DDS, PhD, MS 1st edition 01/22/2016, last revision 03/04/2018