
_later%20smaller%20diameter.jpg)
%20D%20margin%20deep.jpg)




 |
 |
 |
 |
 |
 |
_later%20smaller%20diameter.jpg) |
%20D%20margin%20deep.jpg) |
 |
 |
 |
 |
 |
 |
A Layer of Spongy Bone In Posterior Mandible
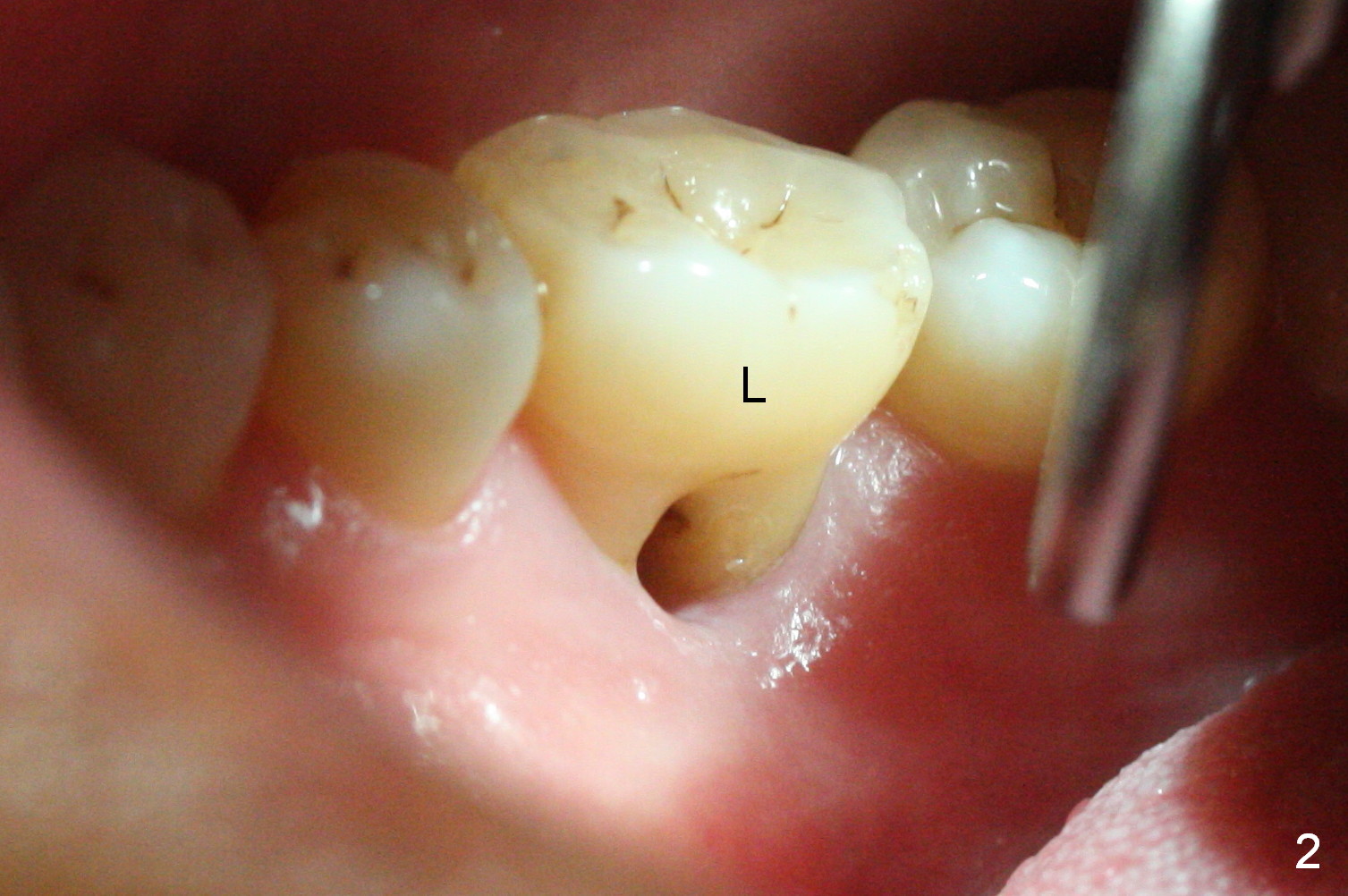
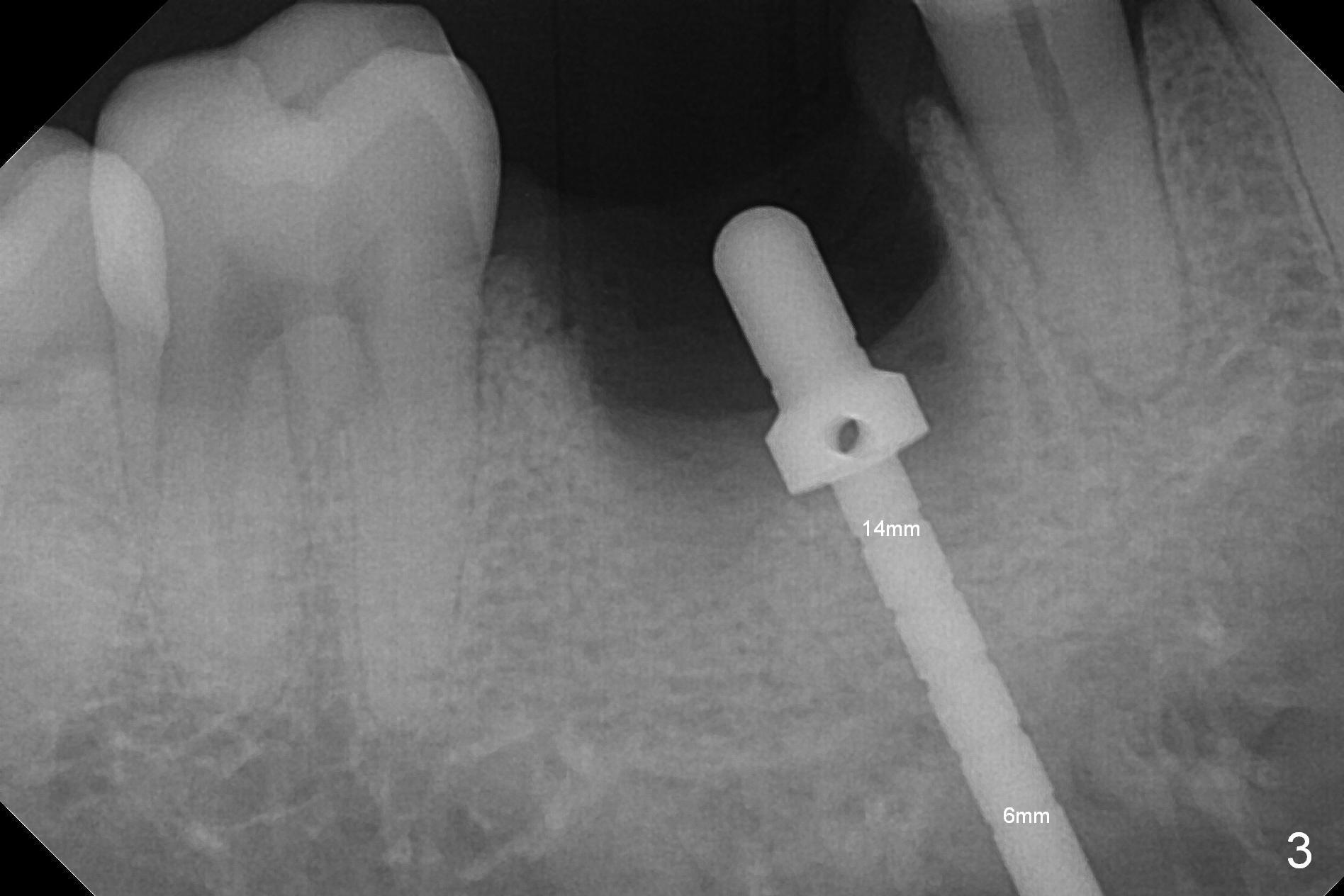
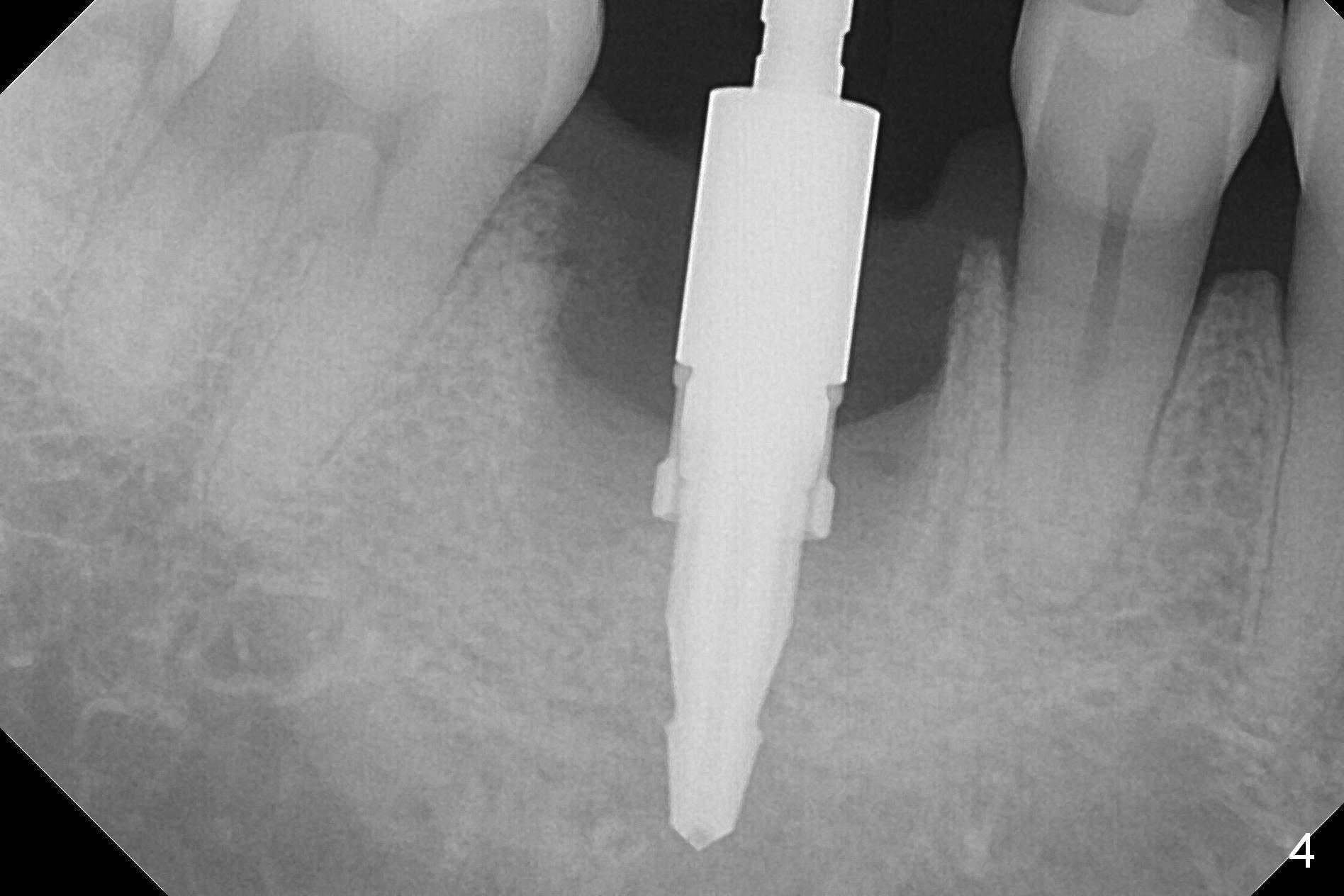
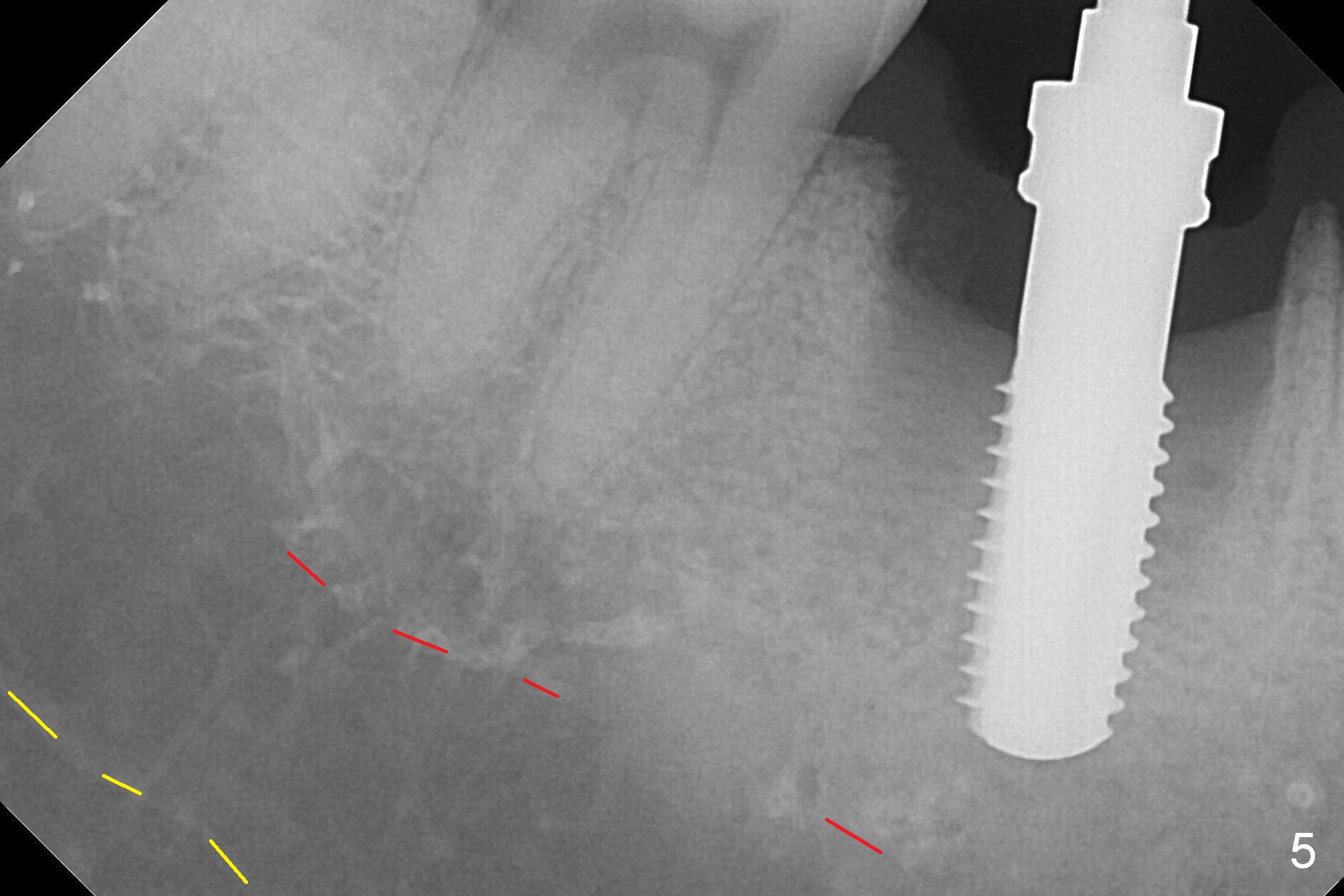
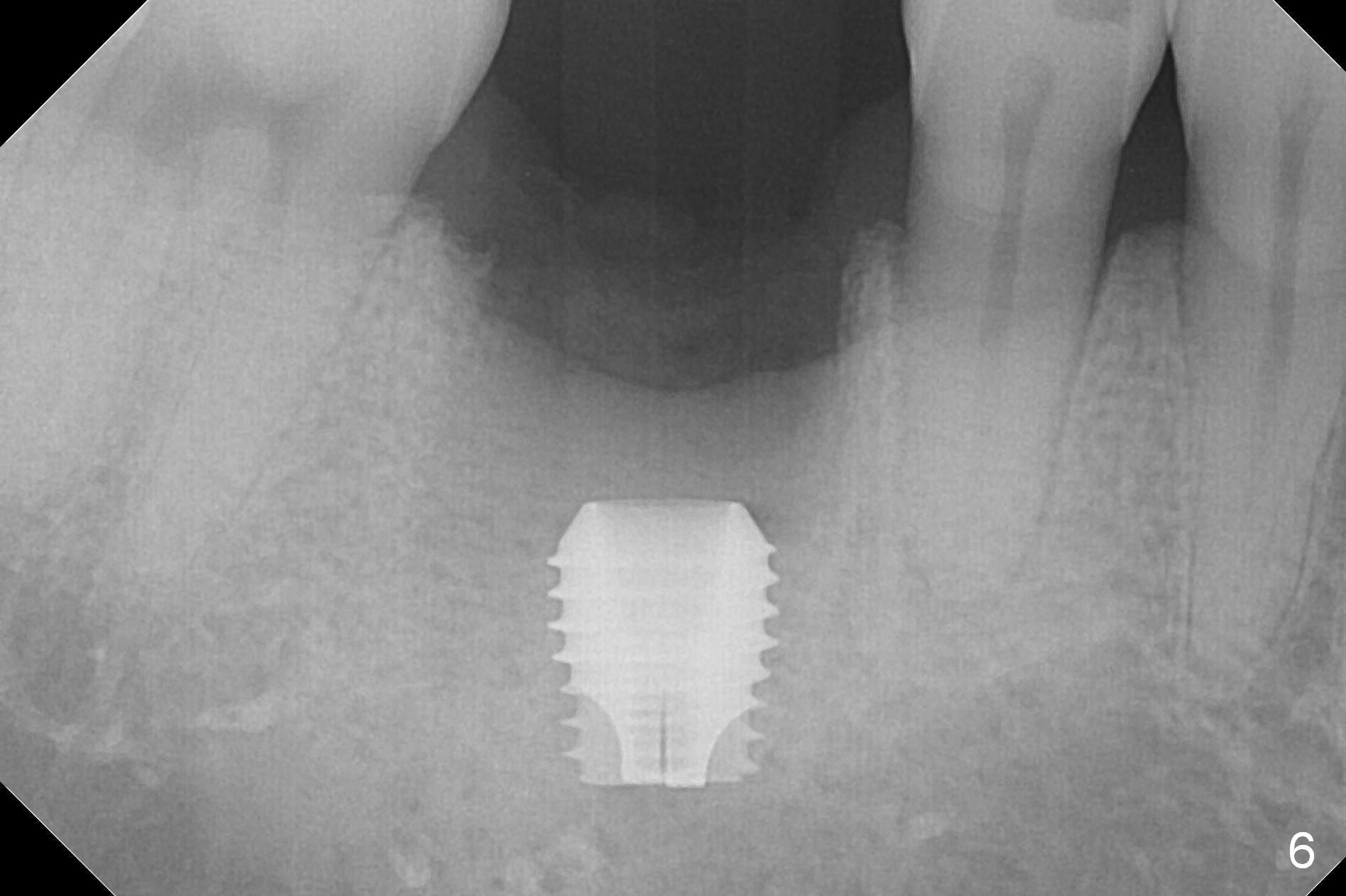
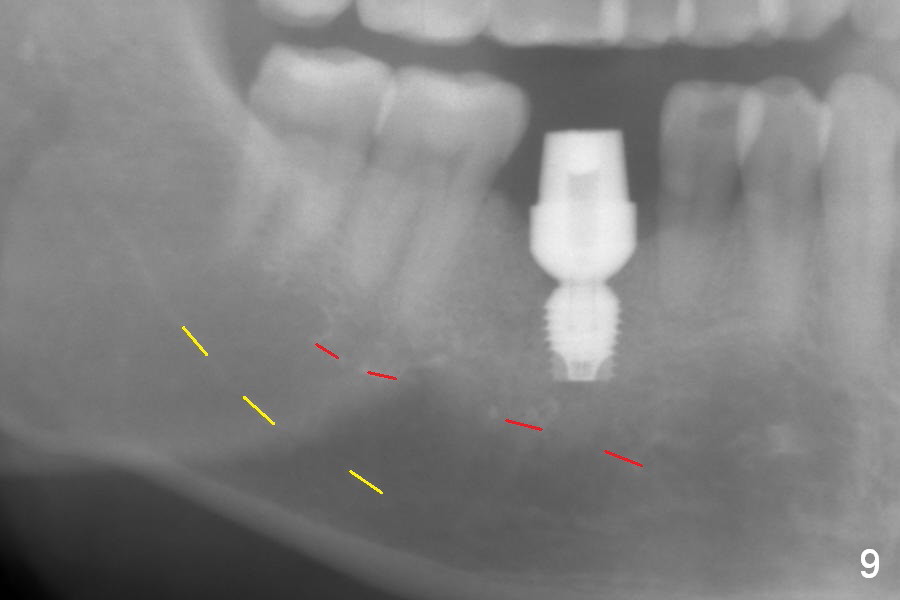
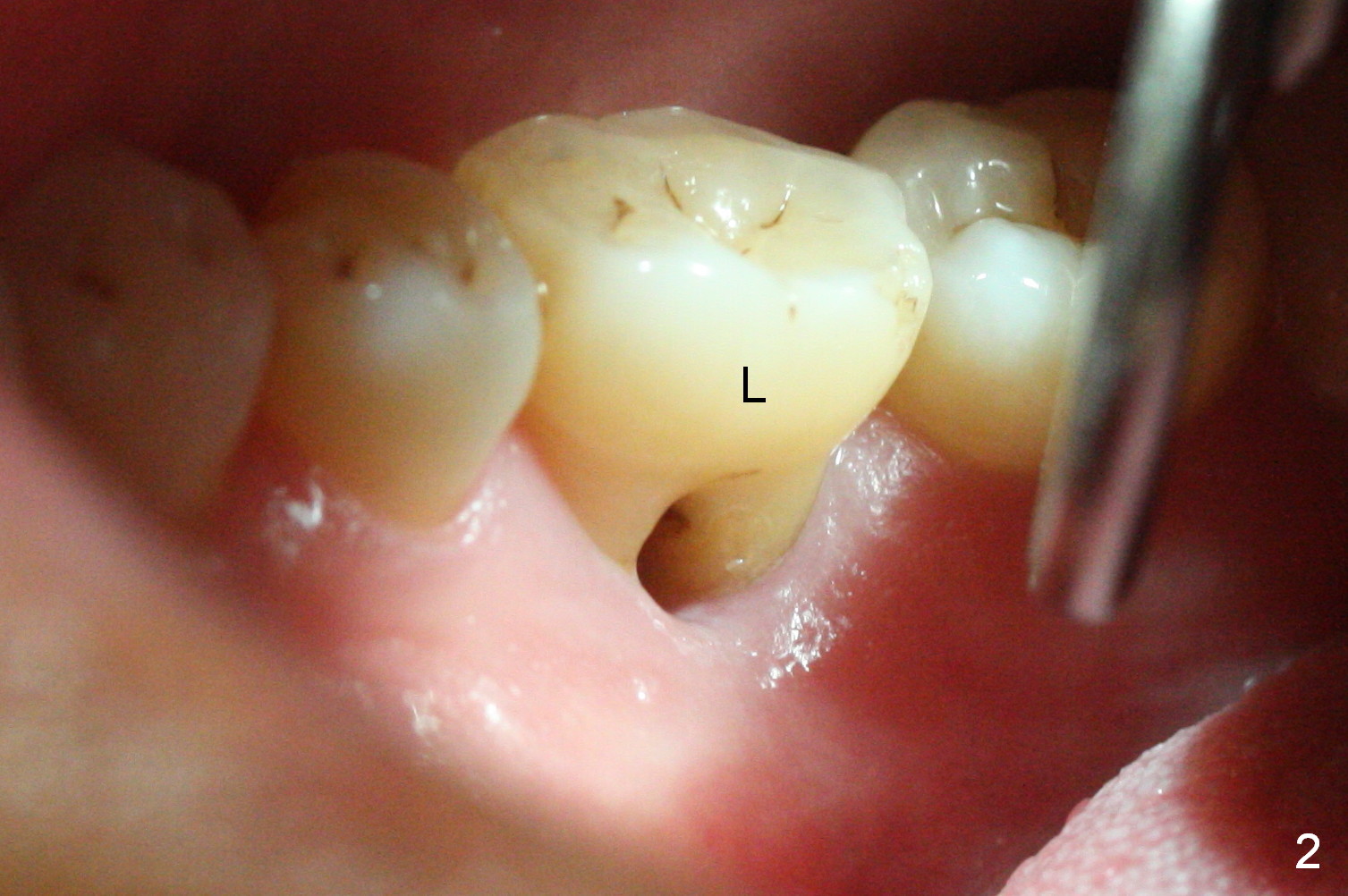
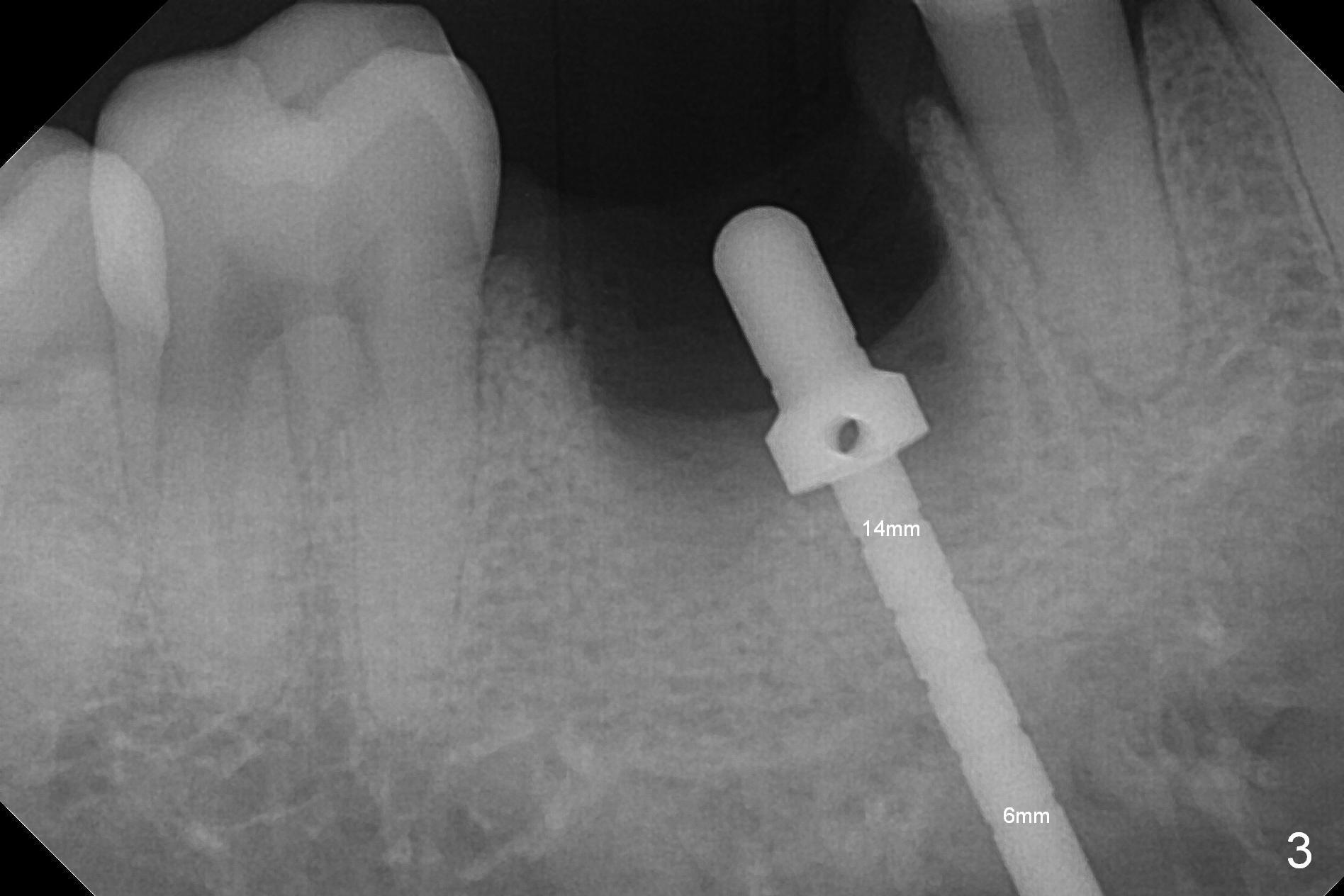
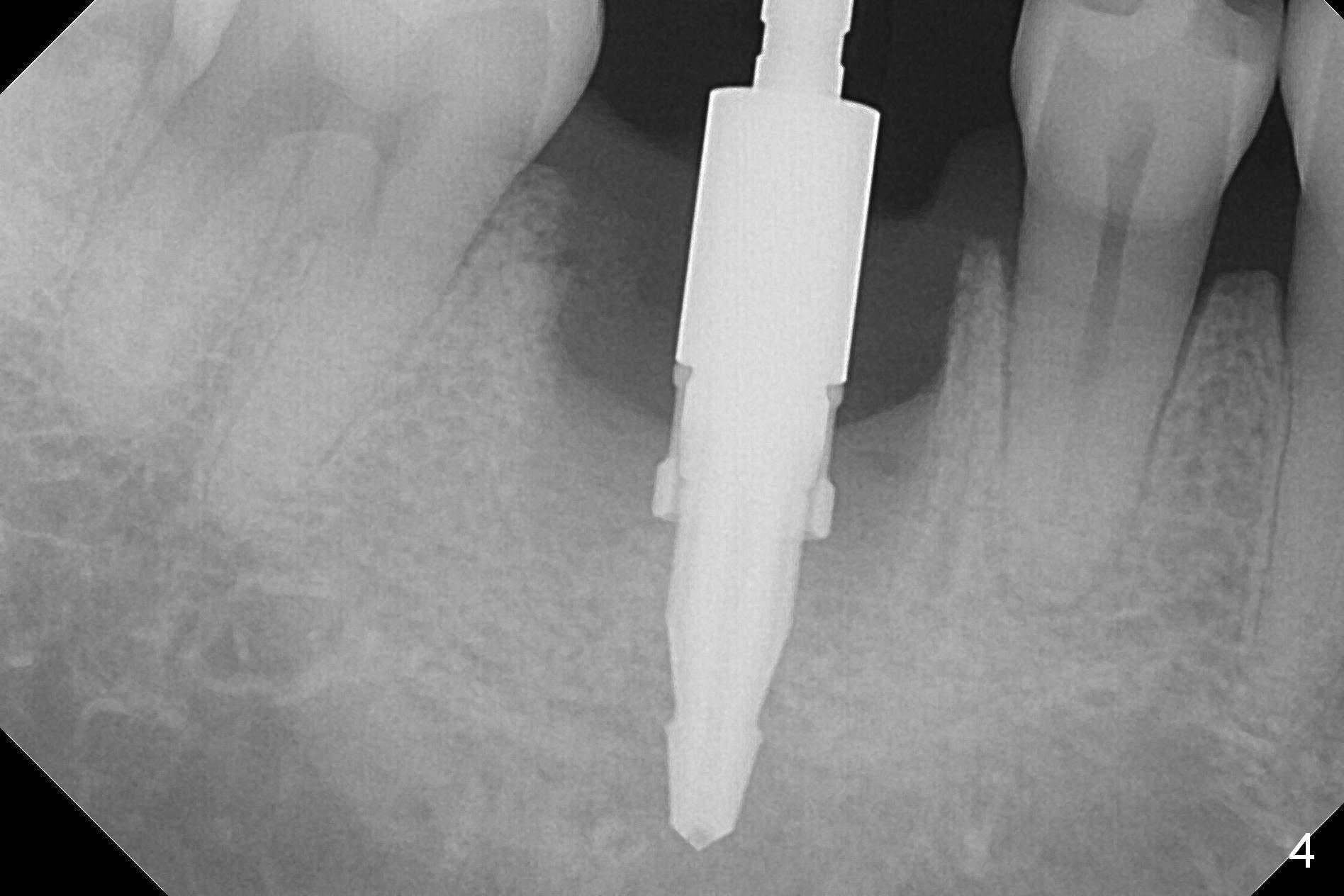
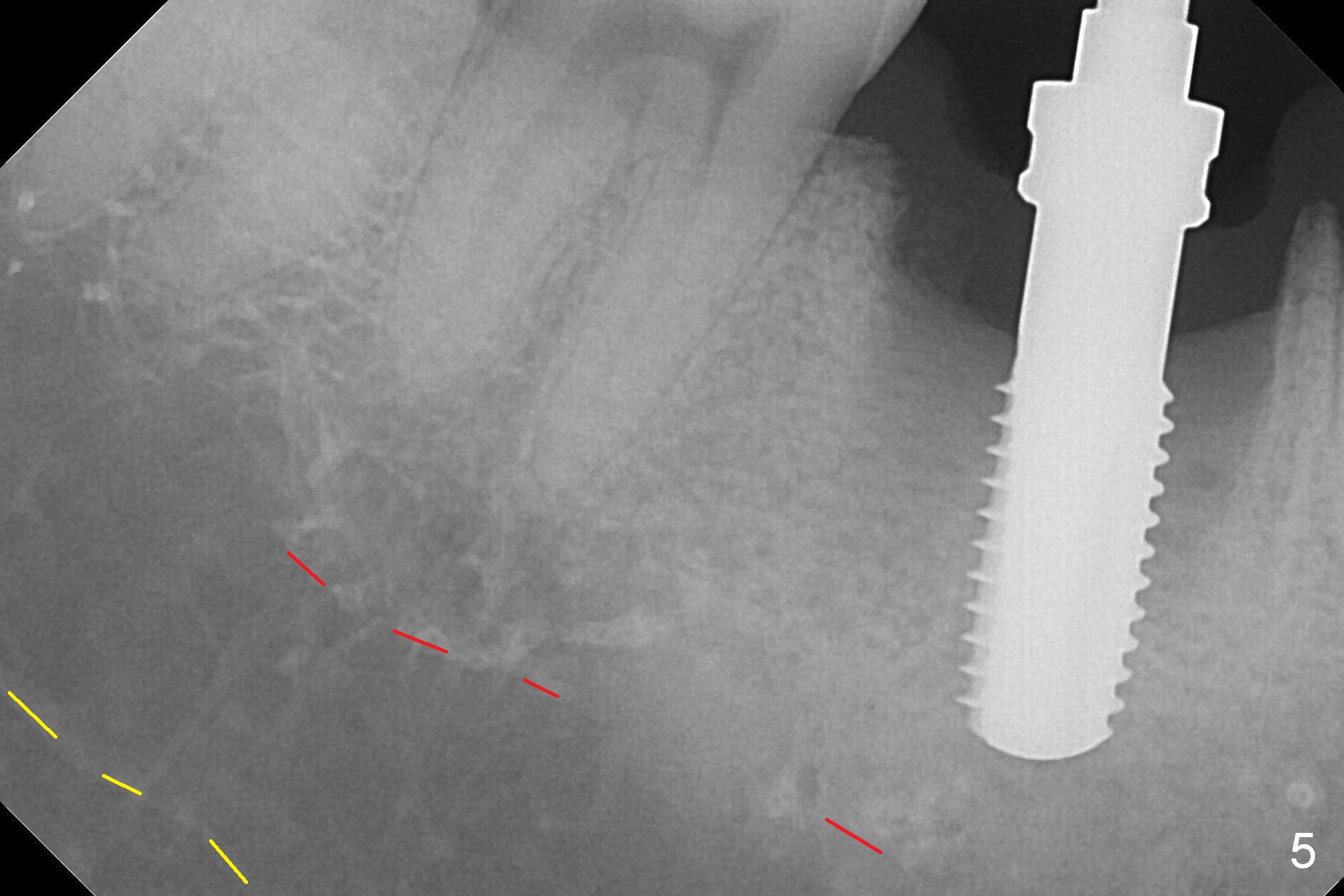
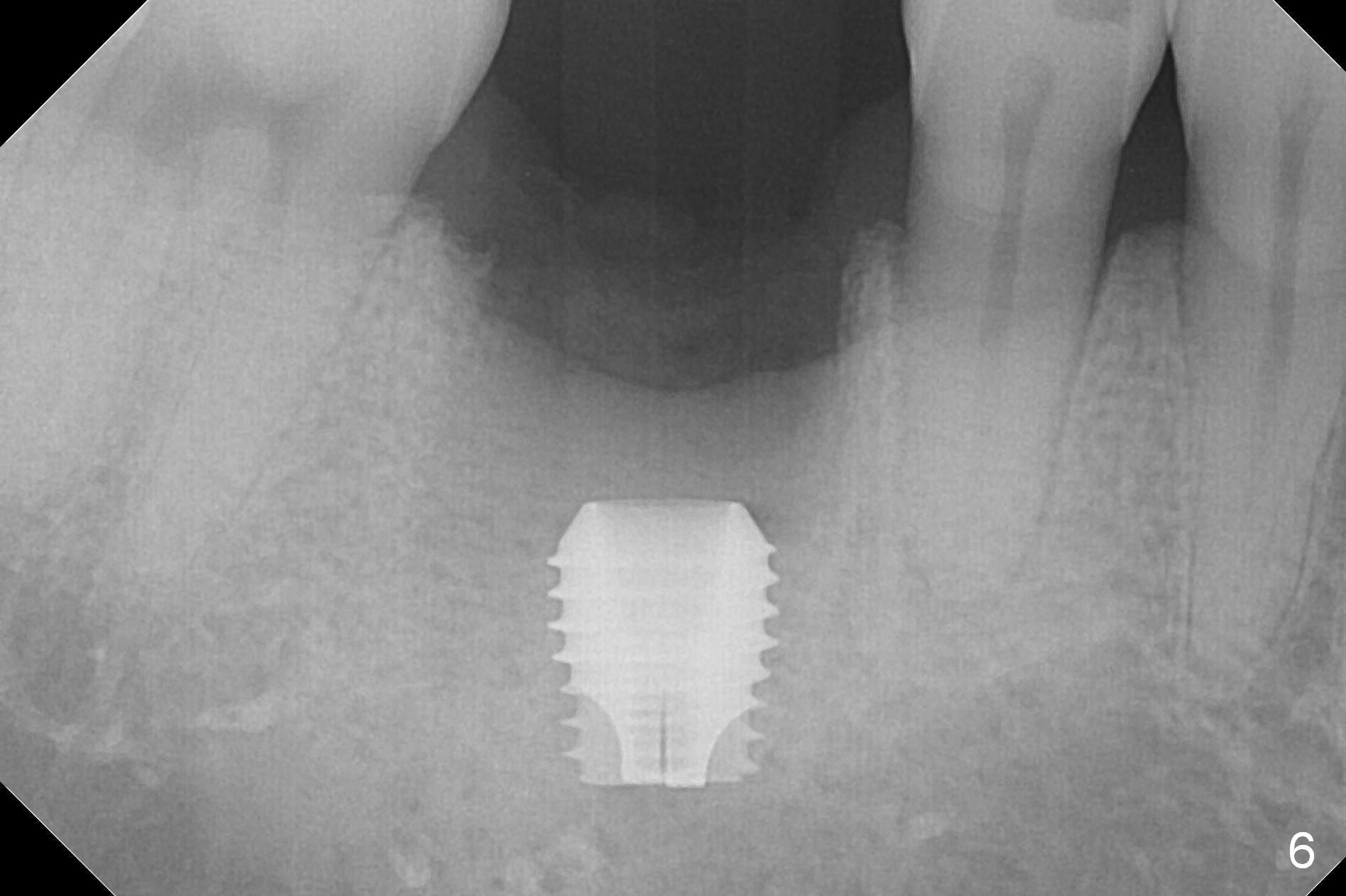
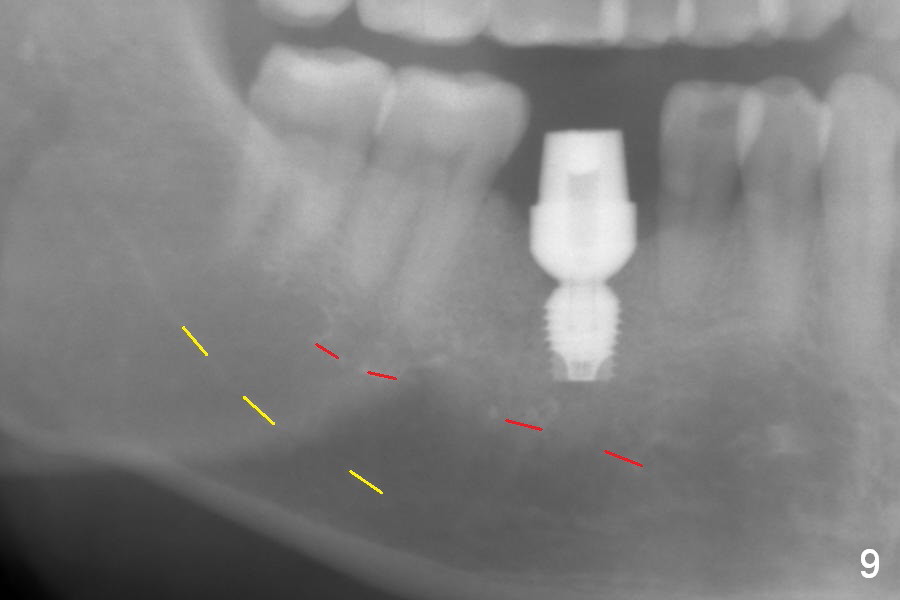
After extraction of the tooth #30 with Class V furcation involvement (Fig.1 (>),2 (L: lingual)), initial osteotomy depth is 8 mm with infiltration anesthesia, but a parallel pin is able to be inserted for 16 mm without pain (Fig.3). There is oozing from the osteotomy. Osteotomy increases in diameter with depth at 8 mm (Fig.4 (3.8 mm drill),5 (5.3 mm tap)). As the Inferior Alveolar Canal (IAC) is indistinct with increased pain during osteotomy, a 5.9x6 mm implant is placed with >50 Ncm following Septocaine infiltration (Fig.6). When bone graft (Fig.7 *) and 7.8x5.5(6) mm abutment (Fig.7,8) are placed, panoramic X-ray is taken (Fig.9). There appears to be a thick layer of spongy bone in the posterior mandible between the red and yellow dashed lines (Fig.5,9). Panoramic X-ray and/or CBCT should be taken if preop PA does not reveal IAC. This patient seems to be a bruxer. There are mandibular tori. Bone loss (furcation involvement) is not proportional to his oral hygiene status. Functional loading (progressive) should be delayed due to bruxism and the short implant.
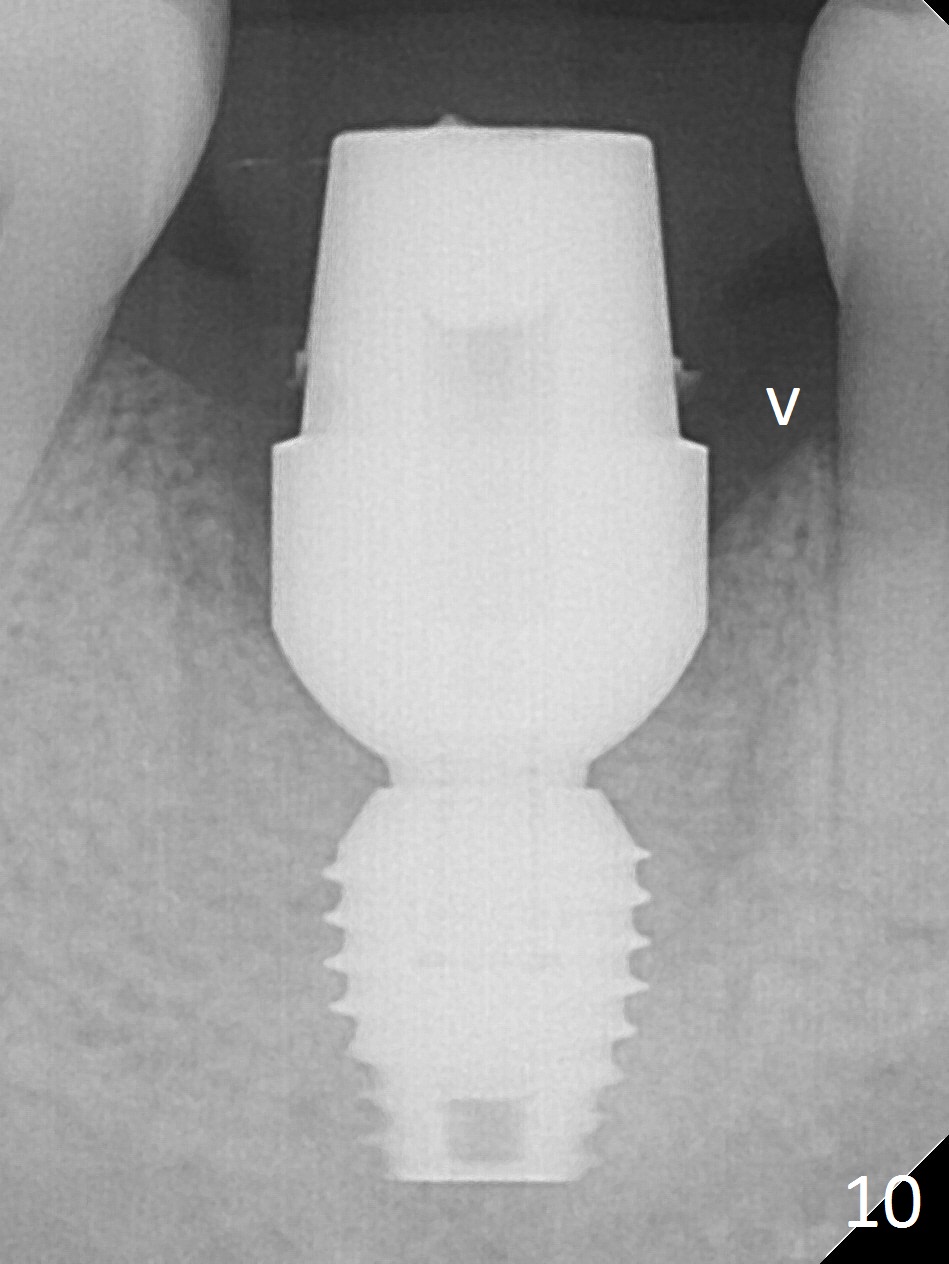
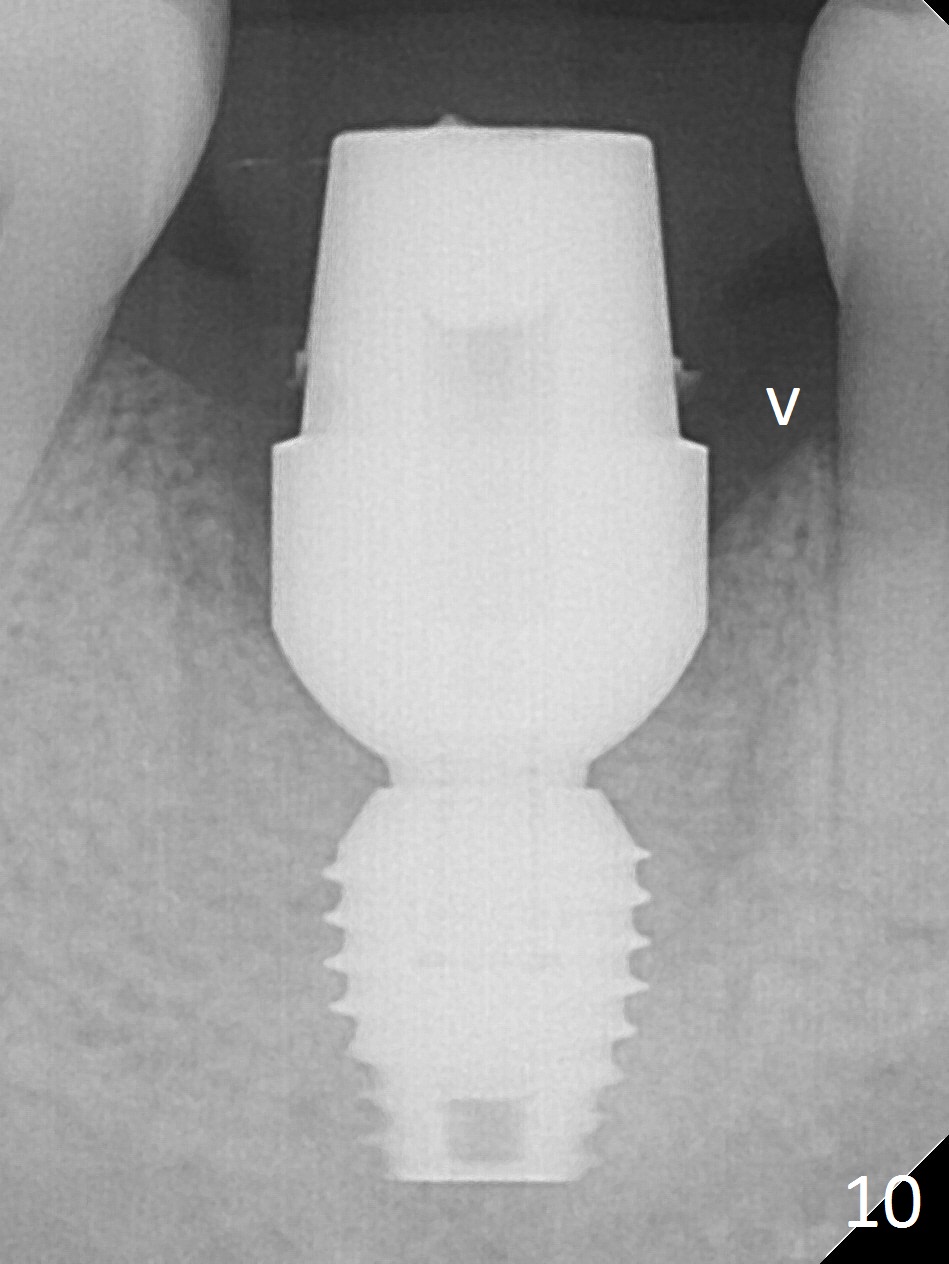
The bone (Fig.10 arrowhead) and soft tissue (Fig.11 *) heal 2 months postop. Gingivectomy is done with Diode prior to impression (Fig.12). The provisional is relined to keep the margin (Fig.13, 2 weeks later) and a permanent crown tries in (Fig.14).
Return to
Lower
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table), IBS
1st Year
Xin Wei, DDS, PhD, MS 1st edition 03/14/2017, last revision 06/11/2017