




 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
Immediate Implant Placed in a Diabetic Patient
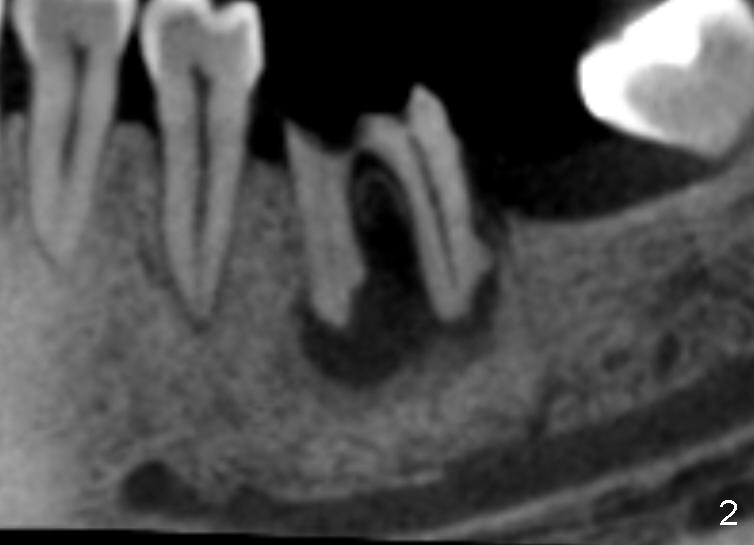
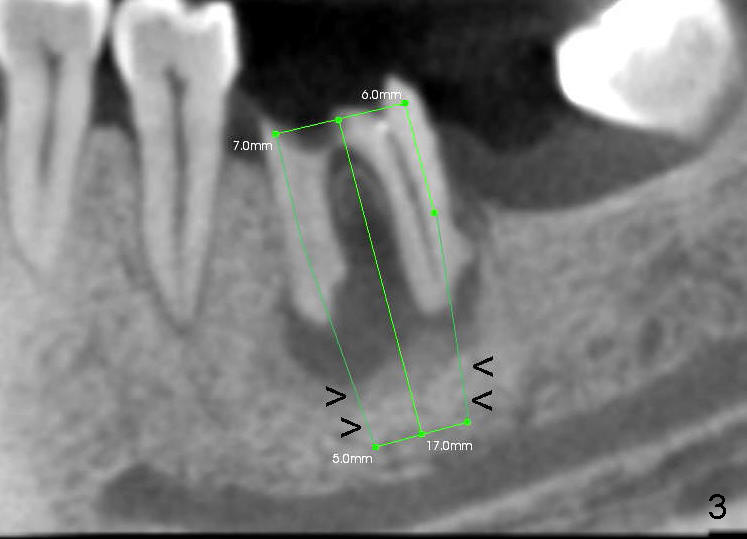
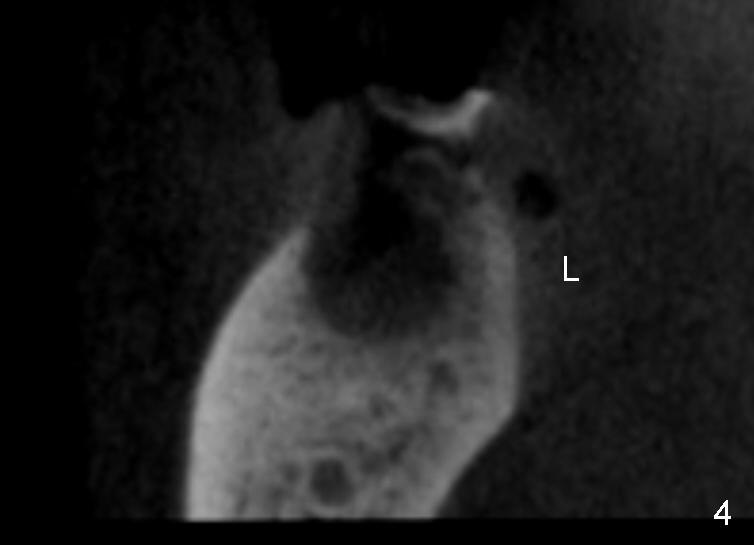
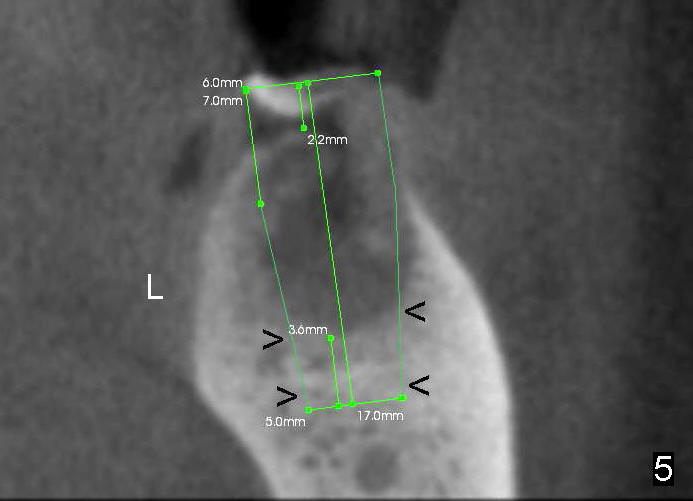
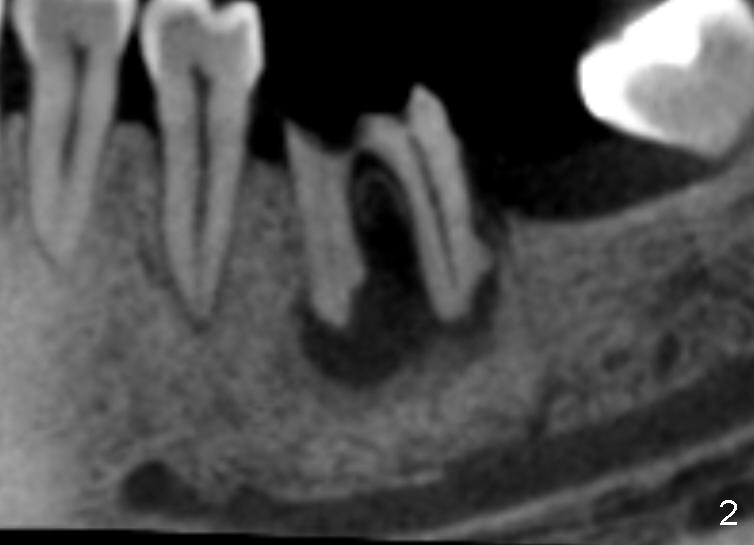
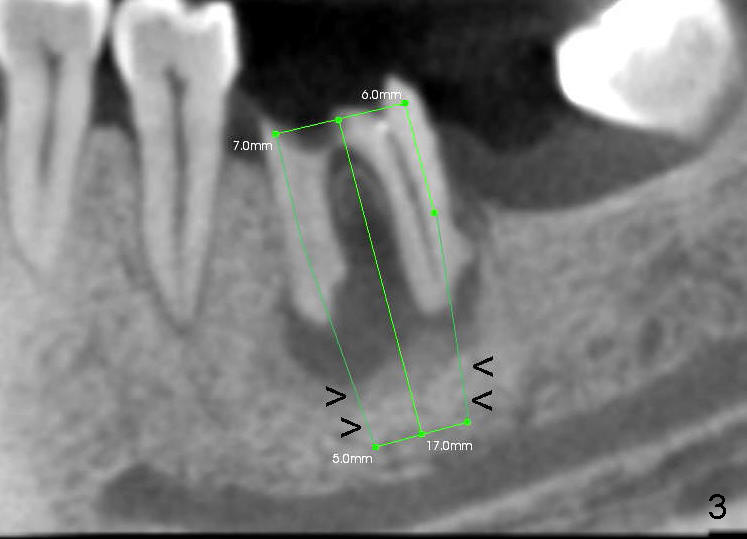
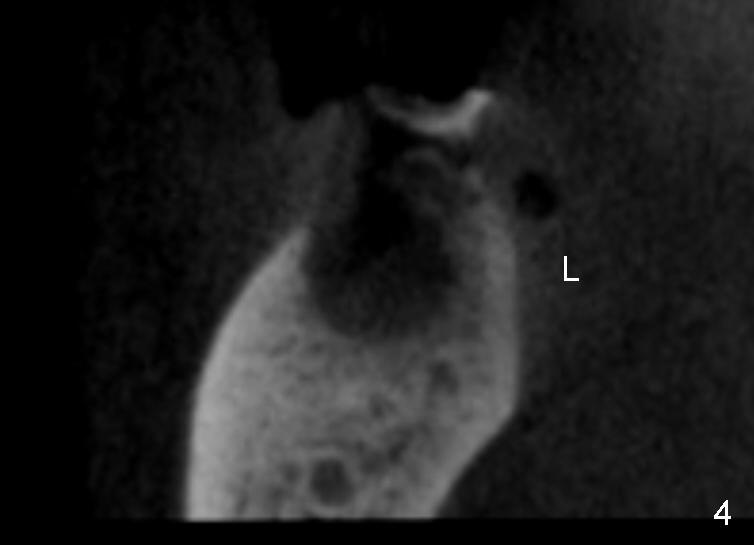
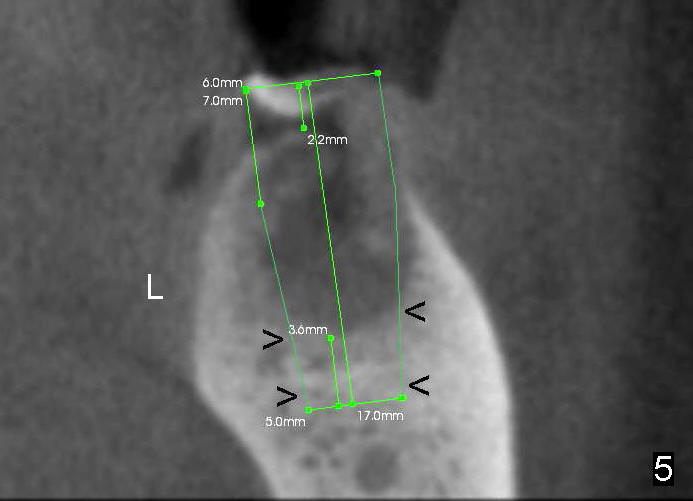
A 46-year-old female patient requests restoration of the lower left 1st molar (Fig.1). Although the patient refuses diabetes treatment, her wounds usually heal uneventfully. Her gag reflex is active. She could not tolerate a removable partial denture, which replaced the missing 2nd molar. Preop PA and CT shows extensive bone loss around the residual roots (Fig.1,2,4). It appears that extraction is simple. Immediate implant should not add too much additional trauma (Fig.3,5). Arrowheads in Fig.3,5 indicate the extent of osteotomy for implantation. With meticulous surgical manipulation, the wound should heal normally.
In addition, the patient is instructed to take Amoxicillin 500 mg tid and rinse with Chlorhexidine two days before surgery. Purulence discharges from the furca when intraligamental injection is applied. Infected granulation tissue is thoroughly curetted from the socket, followed by multiple application of Clindamycin gauze and copious irrigation. Reamers at slow speed (50 RPM) are used to save the autogenous bone, which is placed to the distal and buccal aspects of the socket after placement of 7x17 mm implant (35/40 Ncm). Large implant facilitates socket closure. Chromic suture (4-0) is used to close the wound distally, followed by application of multiple antibiotic ointment and perio dressing around the implant. The patient continues oral antibiotic and mouth rinse postop.
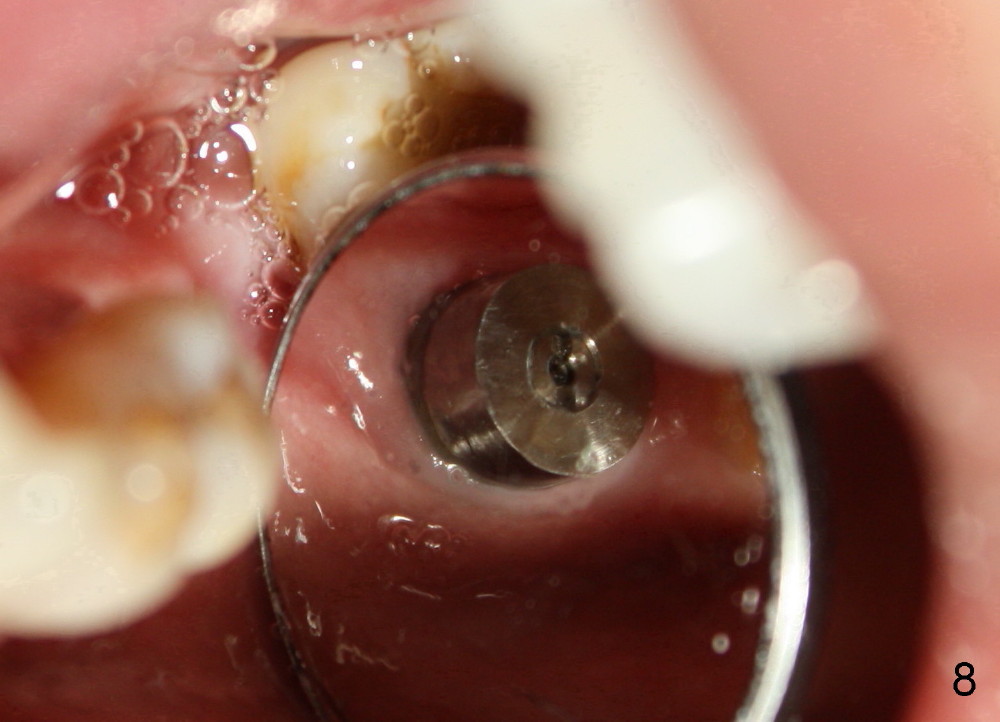
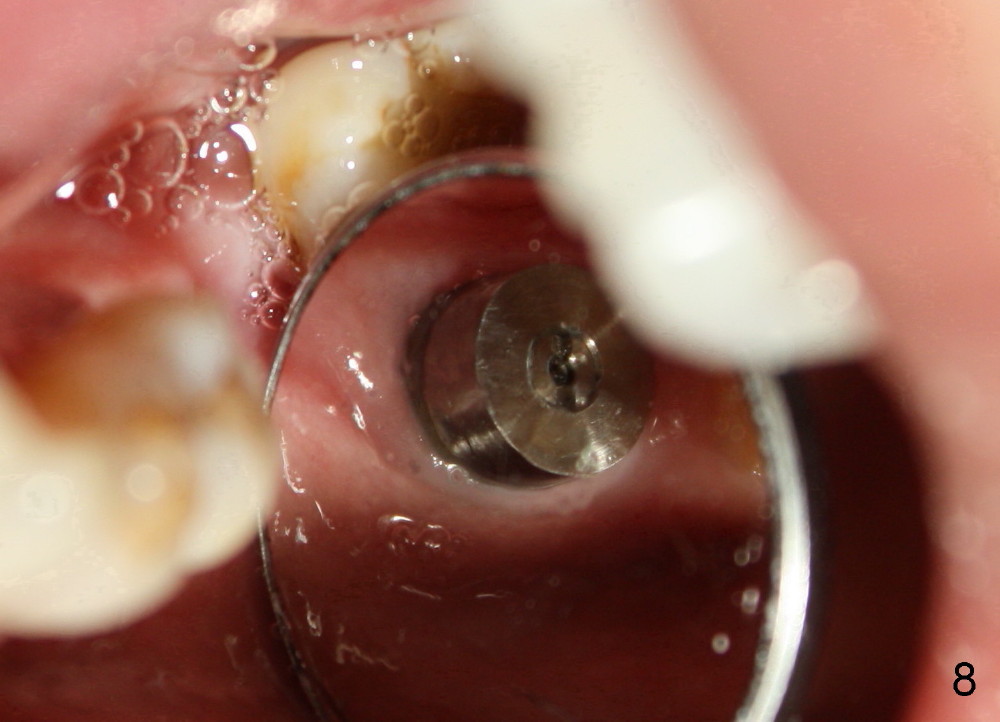
Seven days later, there is no sign of infection around the implant (Fig.6). Chronic infection prior to extraction may recruit our defense mechanism (such as white blood cells), which help prevent posteop infection. Two months postop, the gingiva is healthy around the implant (Fig.7,8).
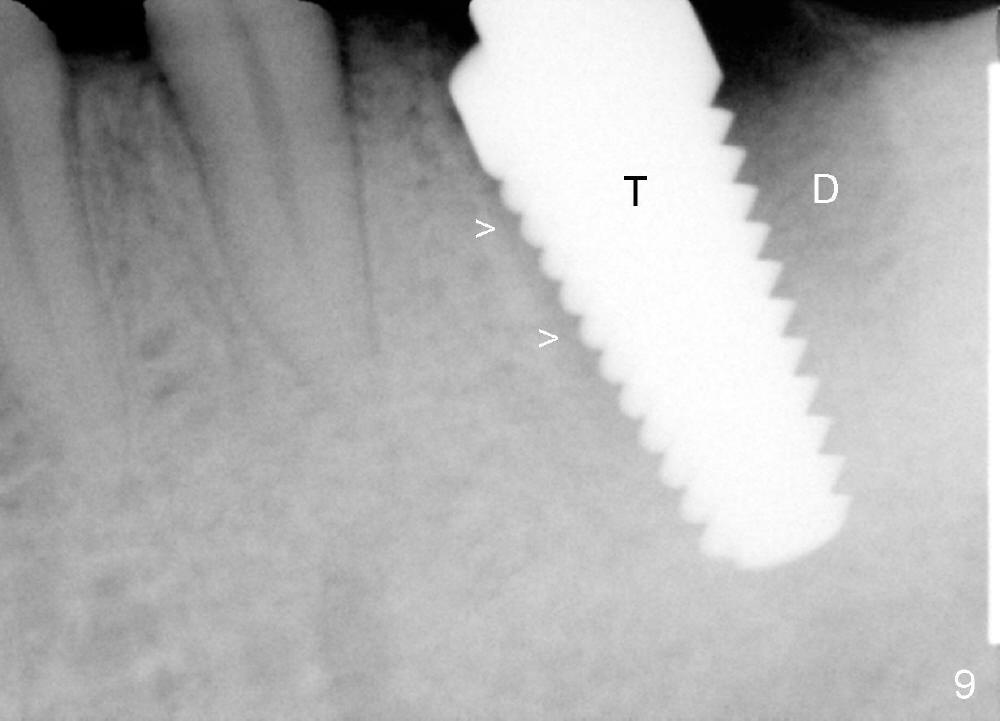
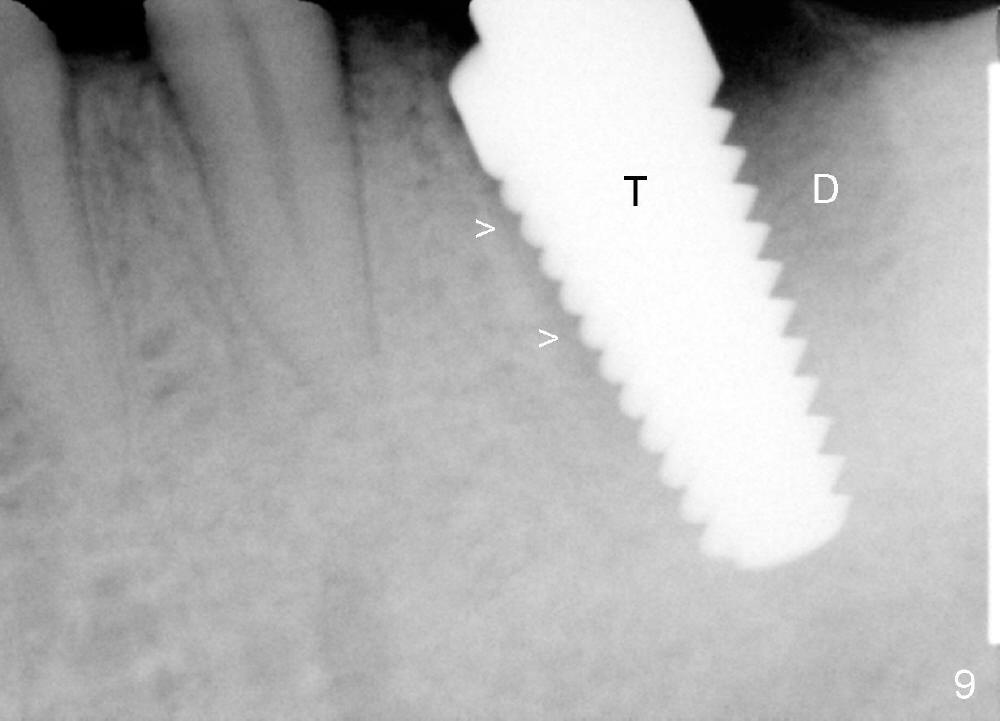
The implant is placed in the mesial socket (Fig.9 T: 7x17 mm tap): the mesial space is being obliterated (>), while the distal one (D) should have been filled with bone graft and the overlying gingiva is approximated with suture (Fig.6). Bone graft is not placed, because graft may increase chance of infection. In fact this assumption is wrong. First, when the tooth #8 is extracted a few months later, bone graft is done with immediate implant. No infection occurs. Second, no bone graft in #18 distal socket leads to gingival recession, as shown below.
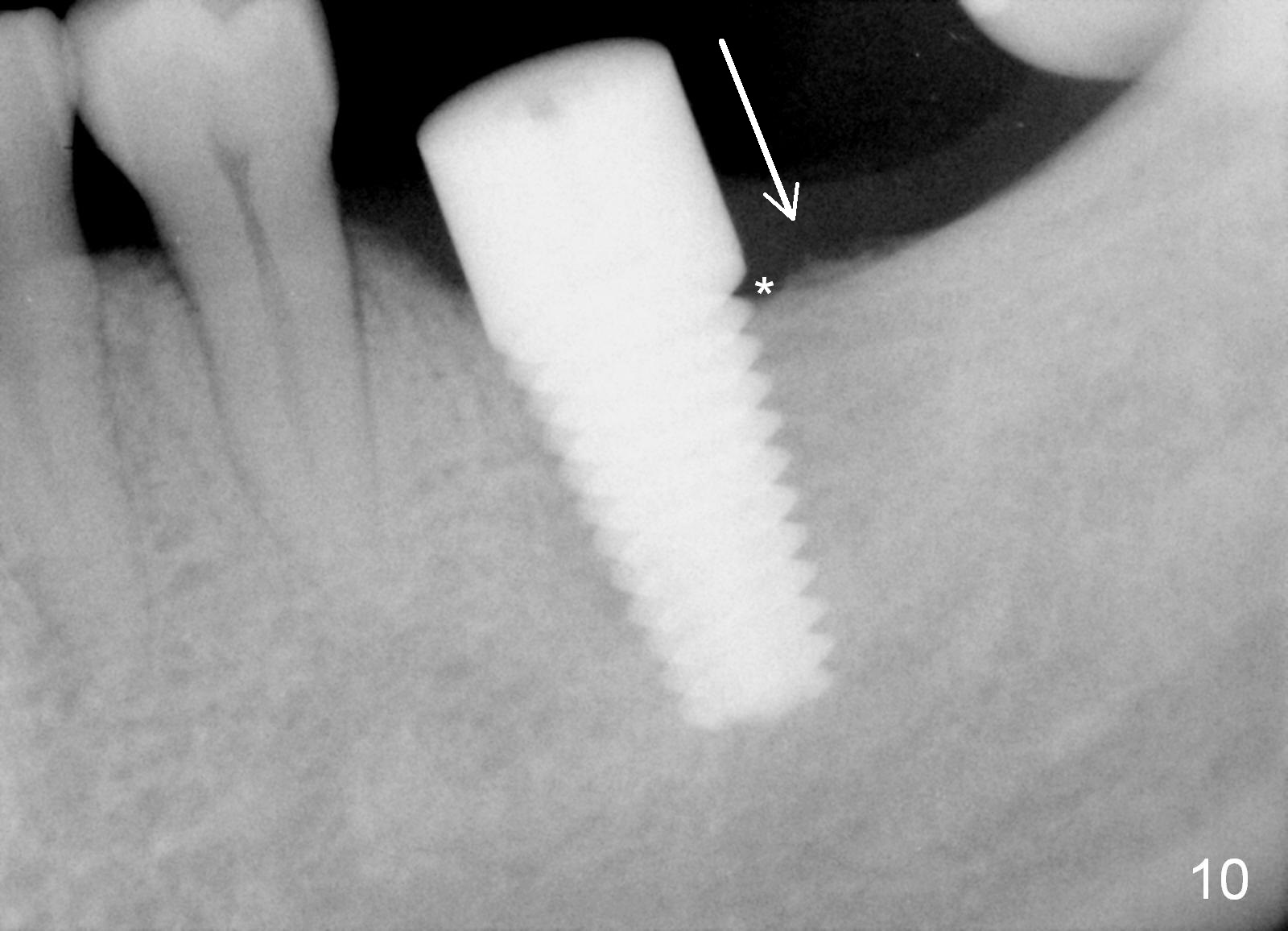
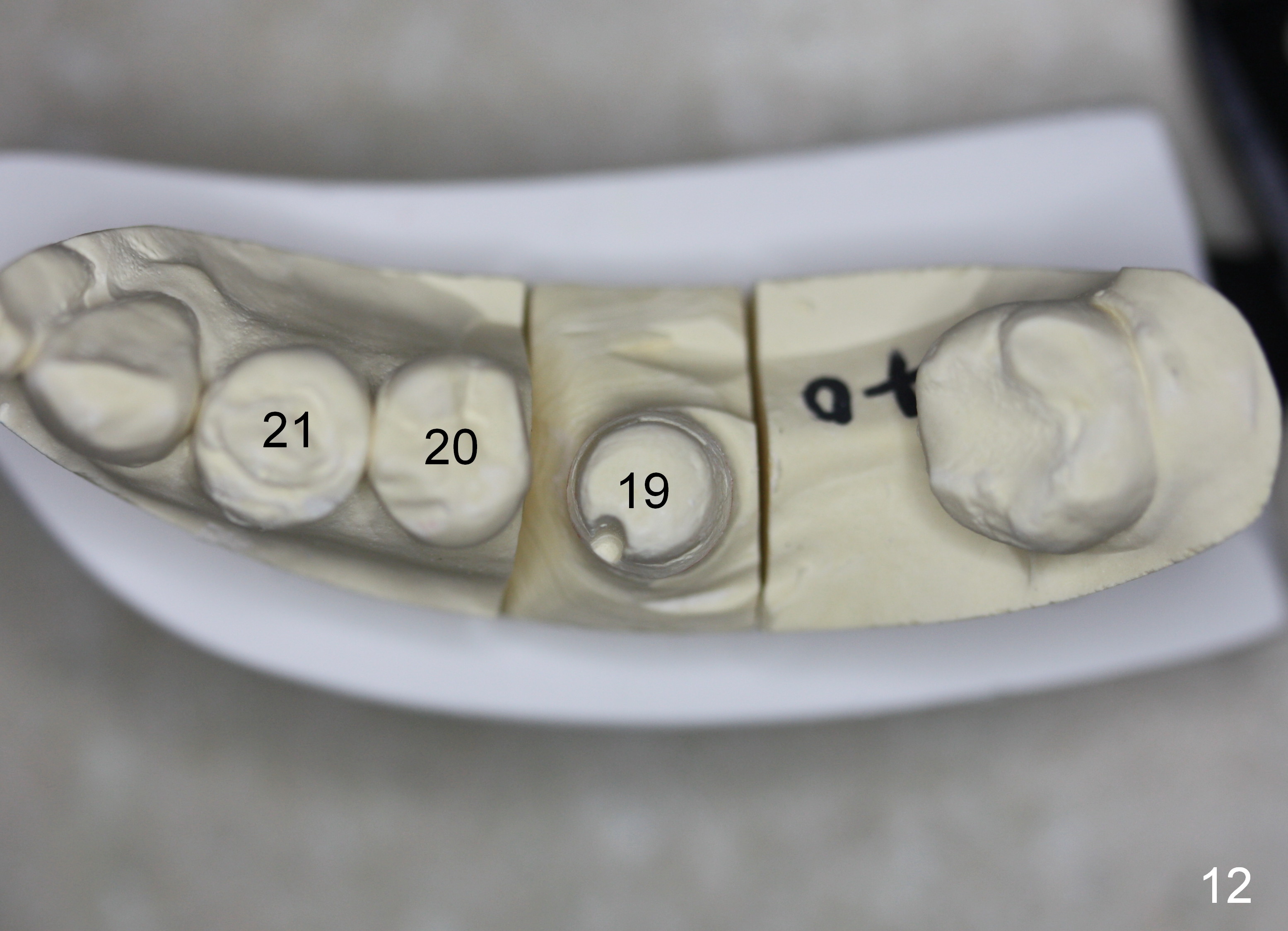
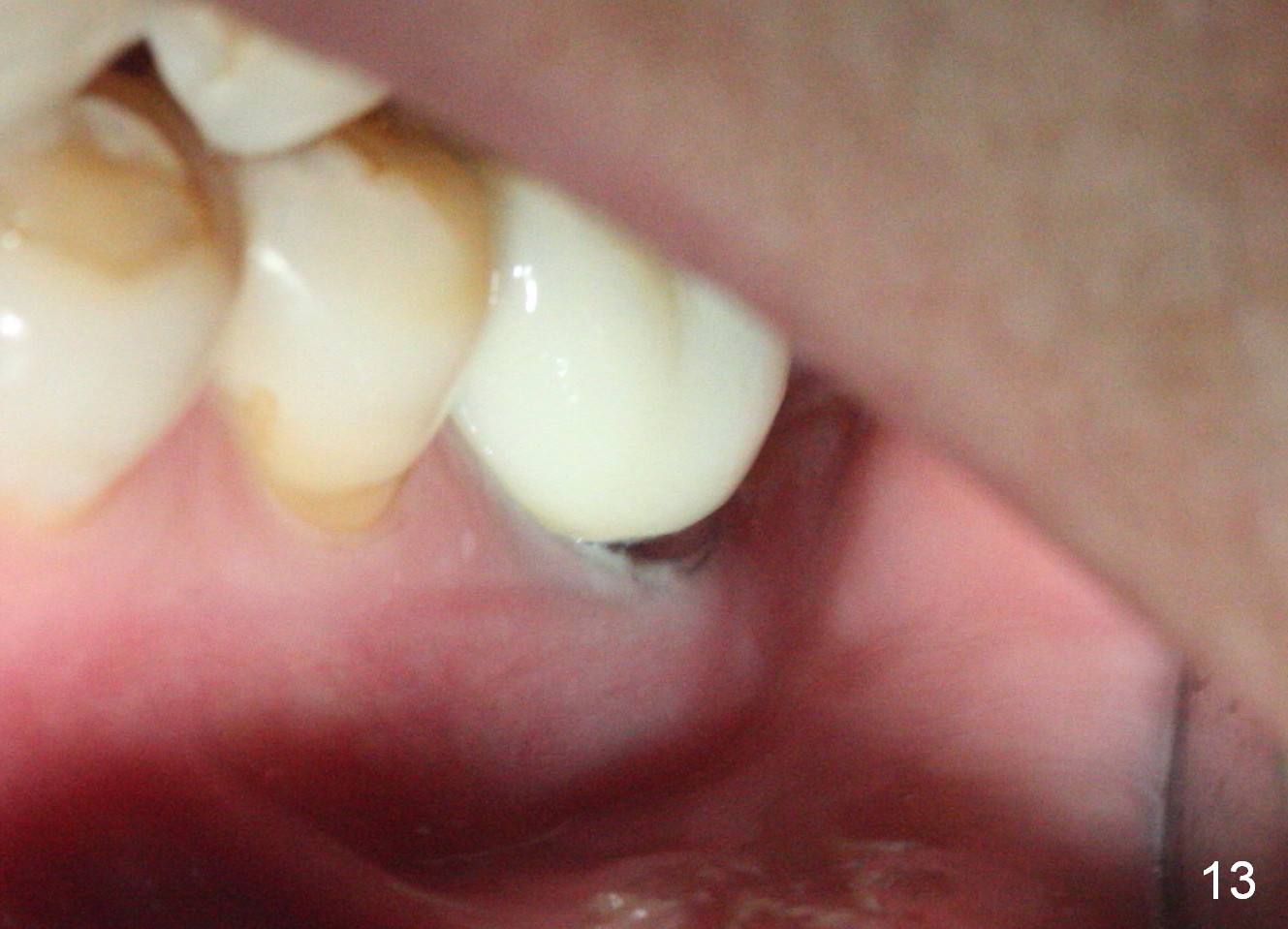
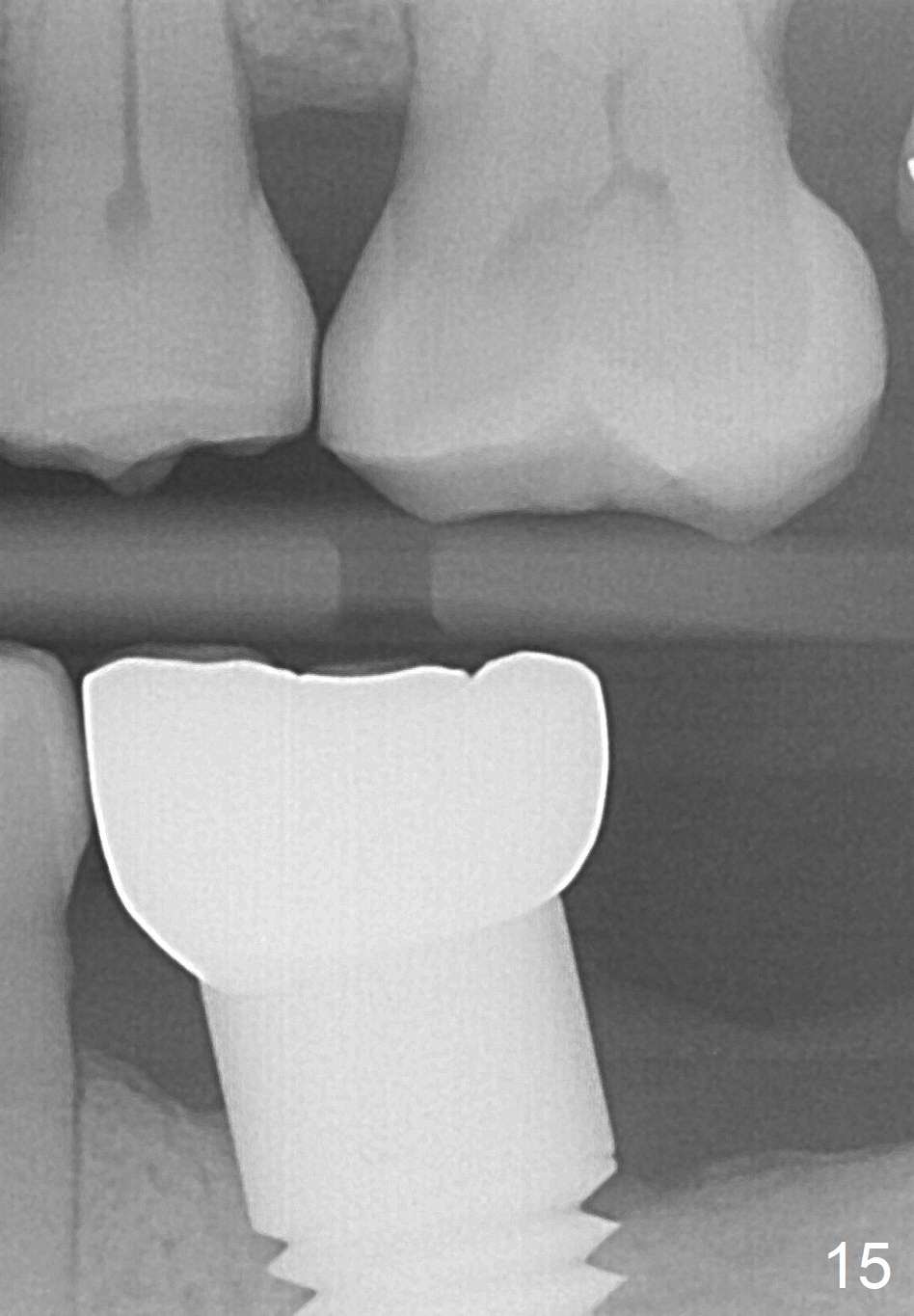
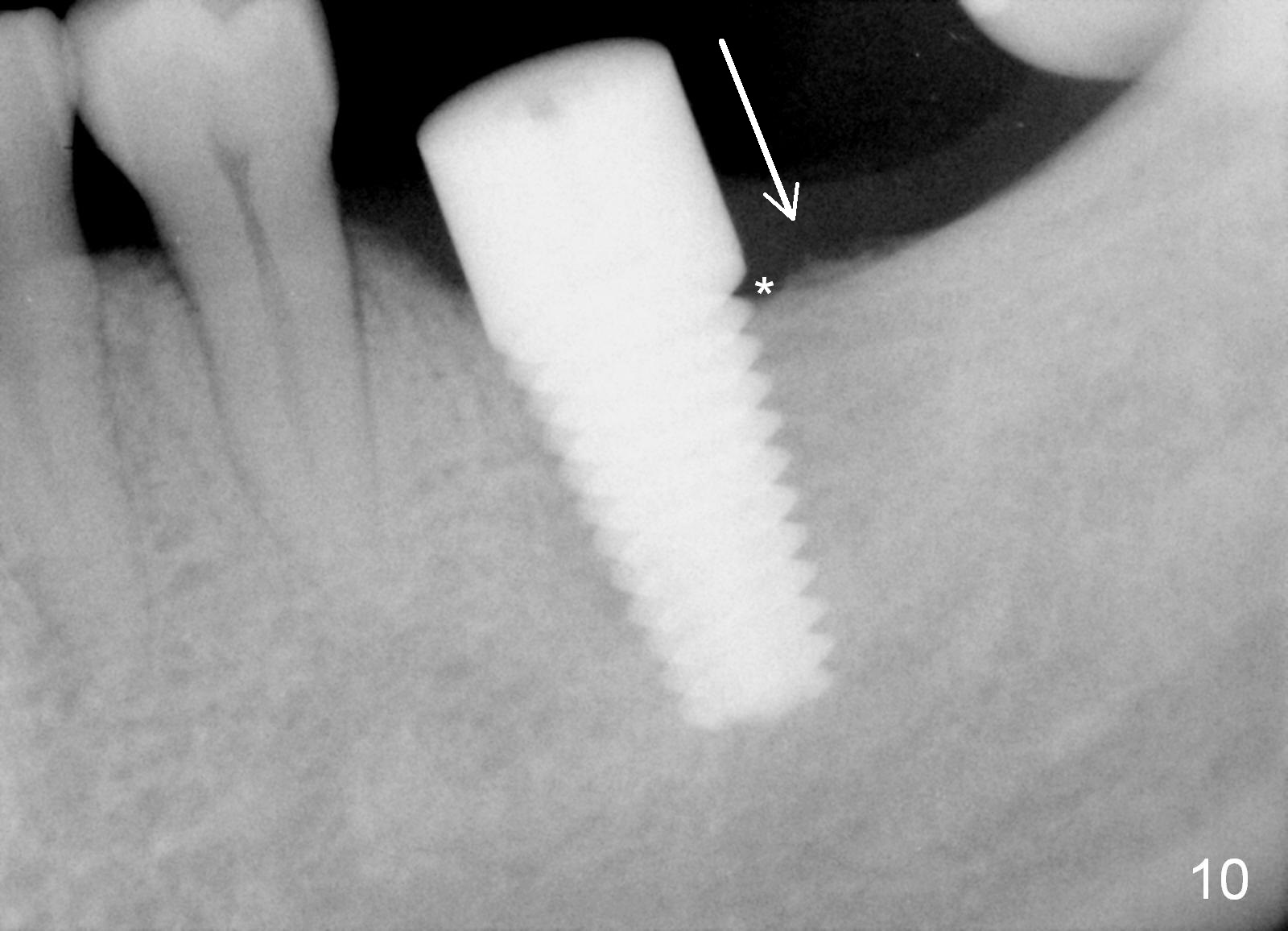
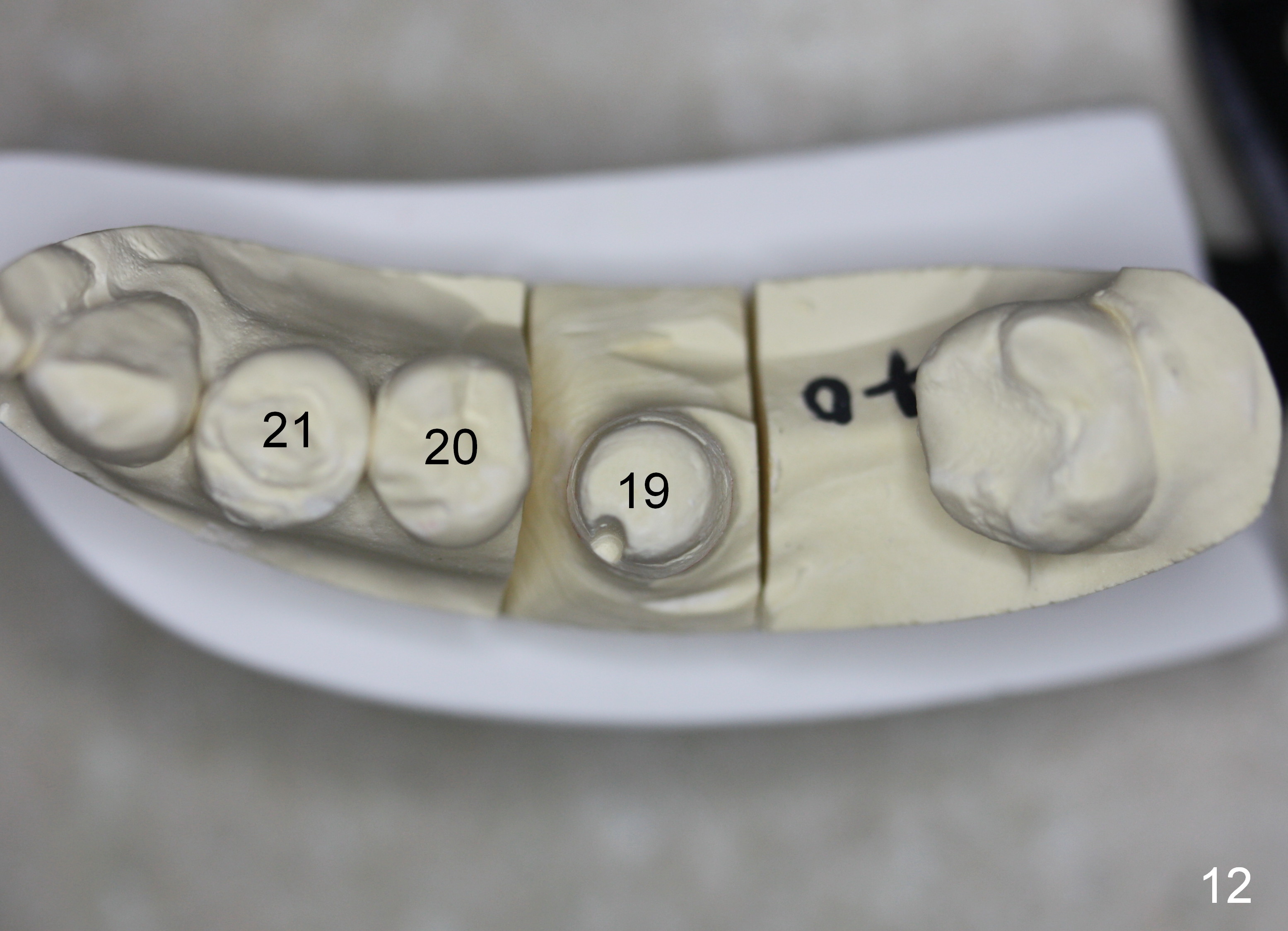
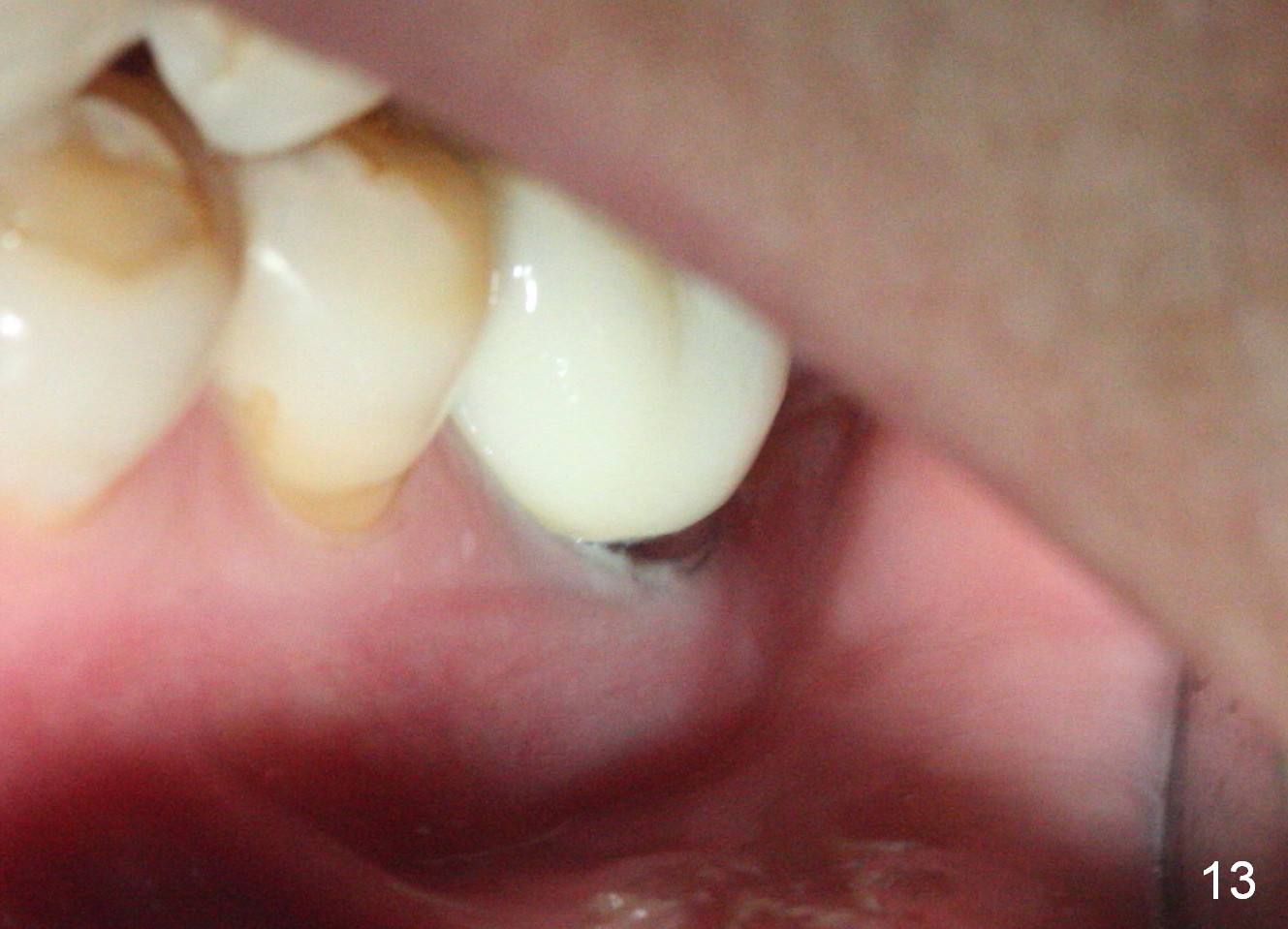
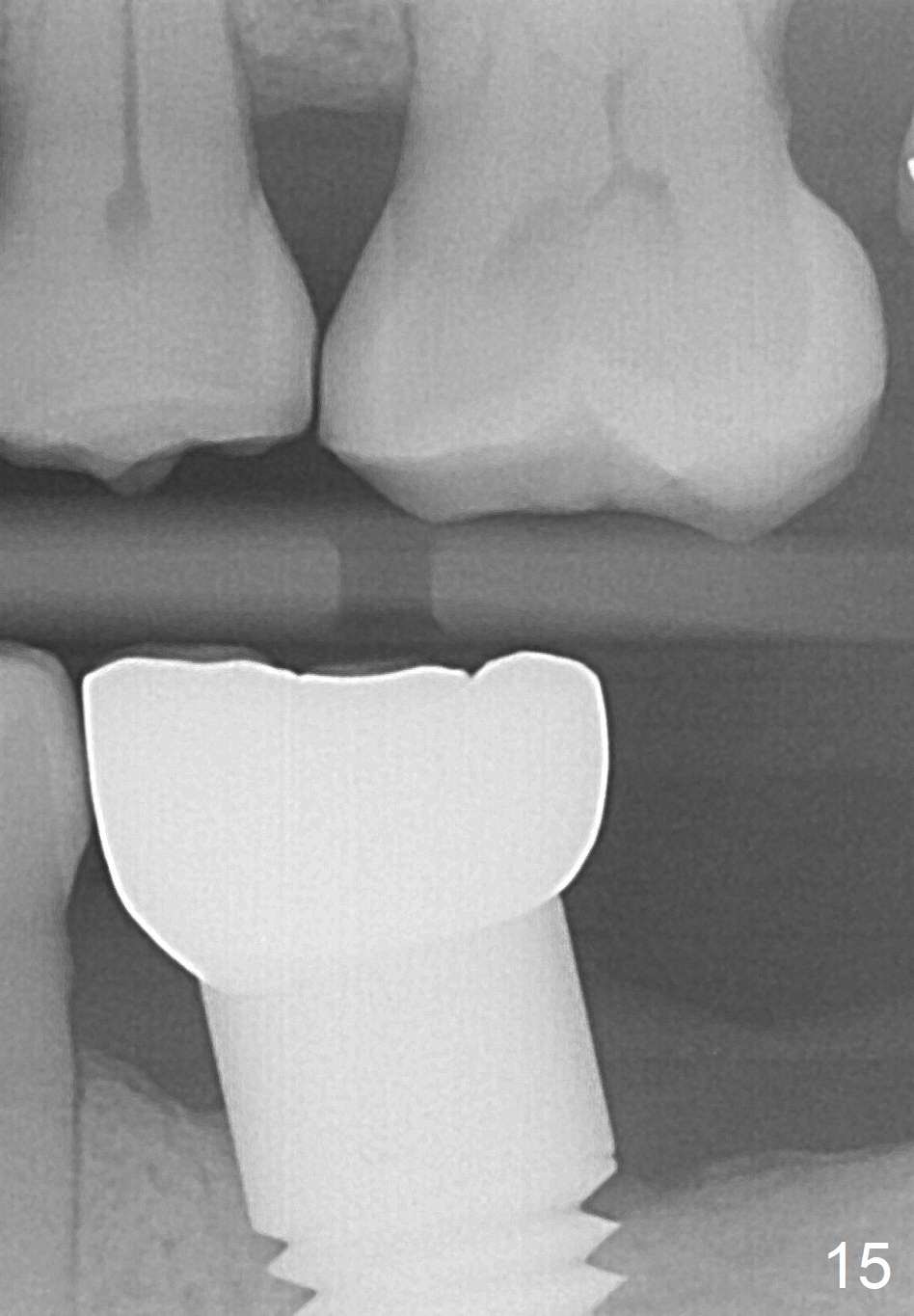
The patient returns for #19 restoration one year postop. The distal coronal threads appear not covered by bone (Fig.10 *) with distobuccal gingival recession (Fig.11). The buccal bulging (Fig.11 arrowheads) may be related to thin or no buccal plate. Bone graft at time of immediate implant may decrease the likelihood. In addition, the implant is placed buccally slightly (Fig.12). The gingival recession appears to have decreased 1 year 9 months post cementation (Fig.13). A thick keratinized gingiva forms around the implant at #8 1 year 11 months post cementation. There seems to be no bone loss 2.5 years post cementation (Fig.14,15, as compared to Fig.10)
Systemic Diseases,
Introduction to Immediate Implant,
Lower Molar Immediate Implant
矫正,糖尿病,种植水平
Xin Wei, DDS, PhD, MS 1st edition 12/29/2013, last revision 12/06/2020