
,%20no%20bone%20graft%20to%20reduce%20interference.jpg)






 |
 |
,%20no%20bone%20graft%20to%20reduce%20interference.jpg) |
|
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
|
Repair of Extensive Hard and Soft Tissue Defect
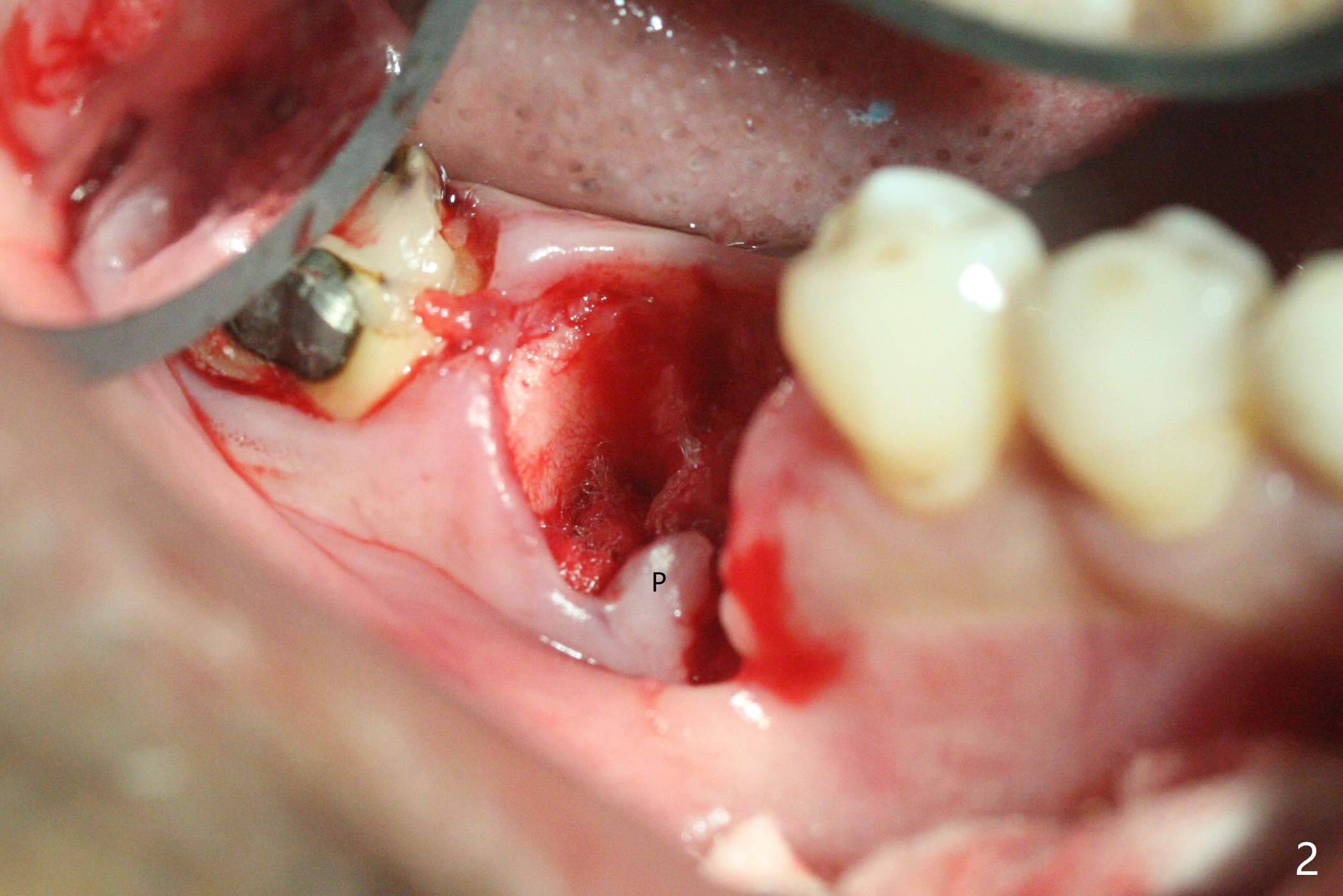
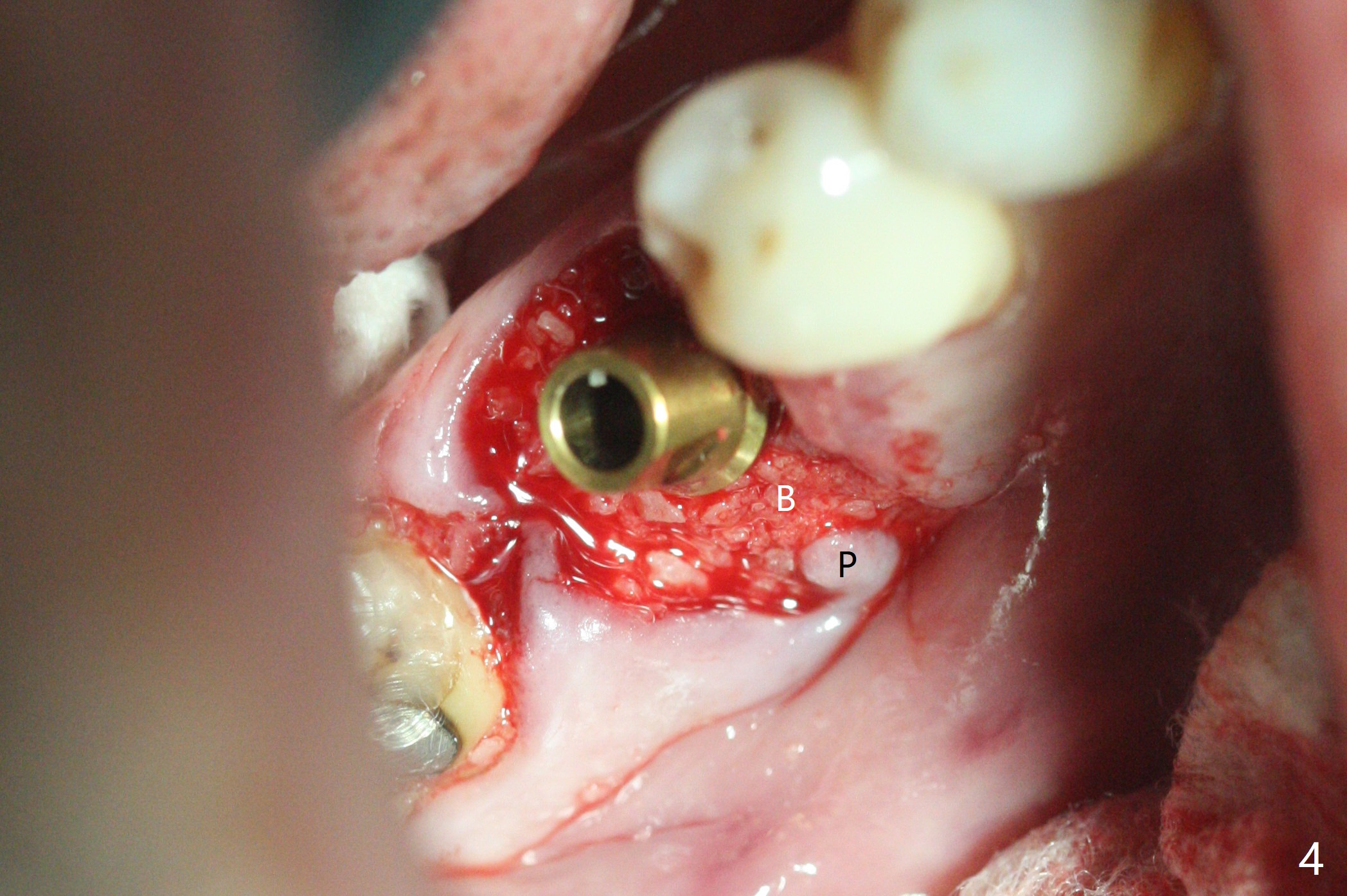
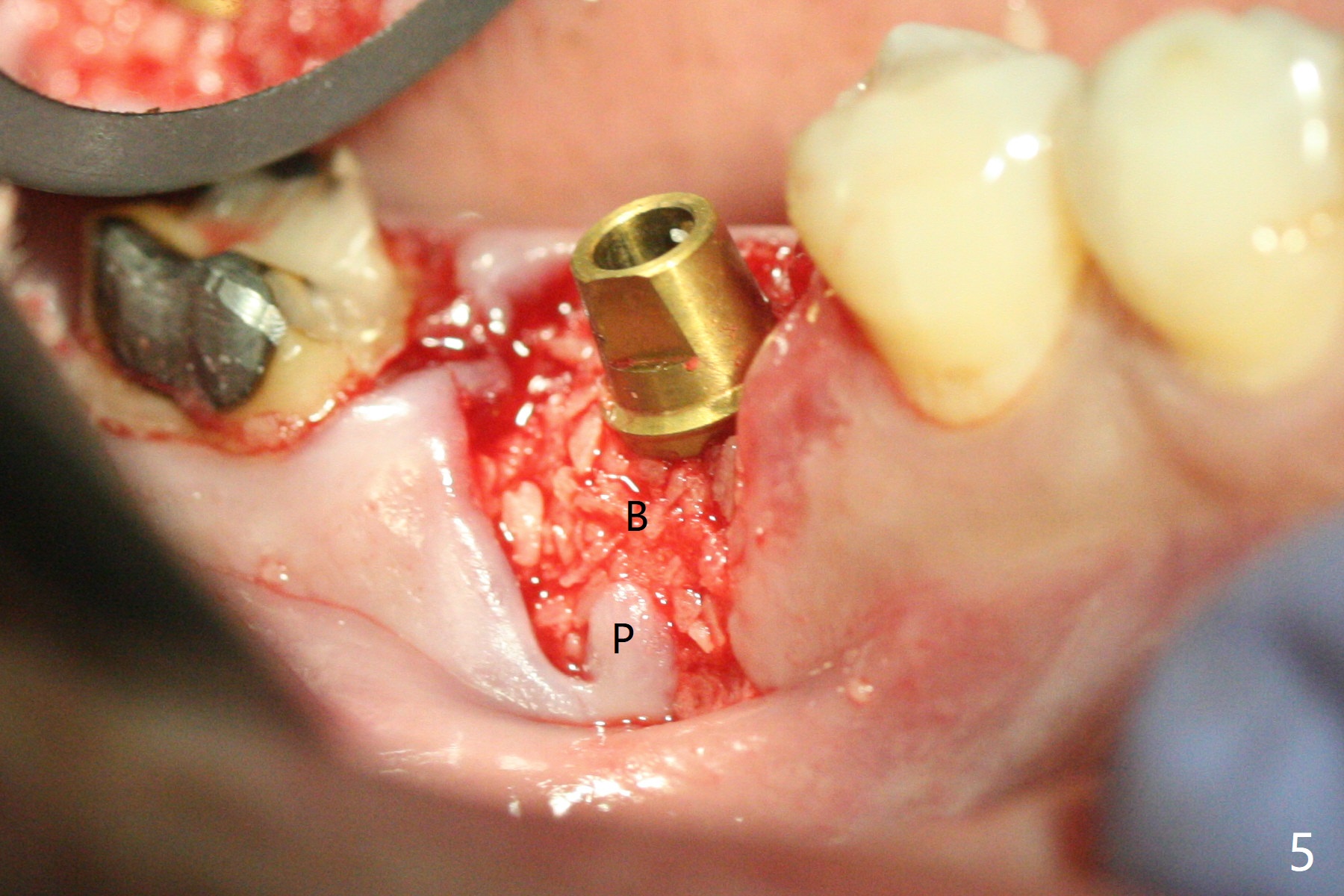
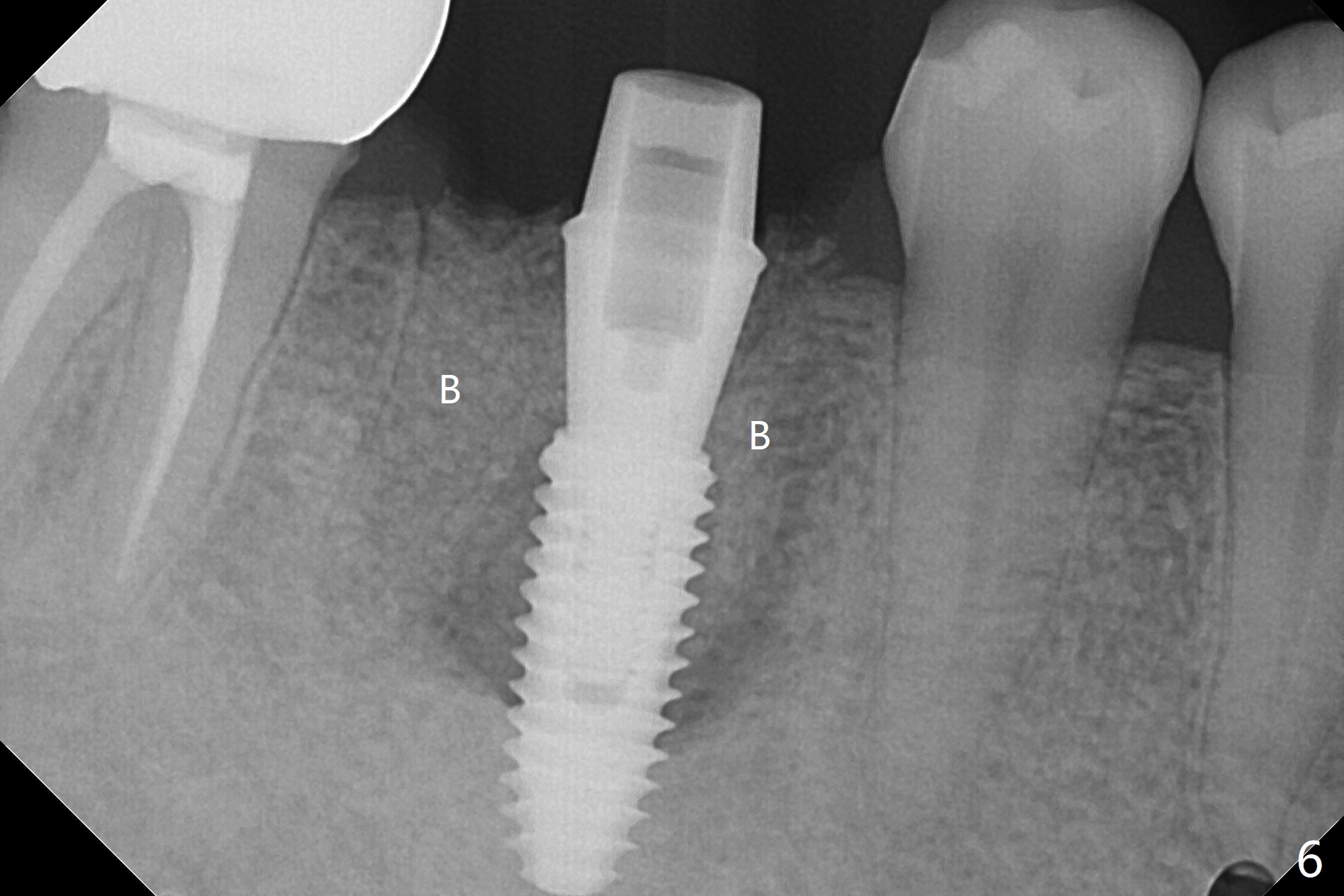
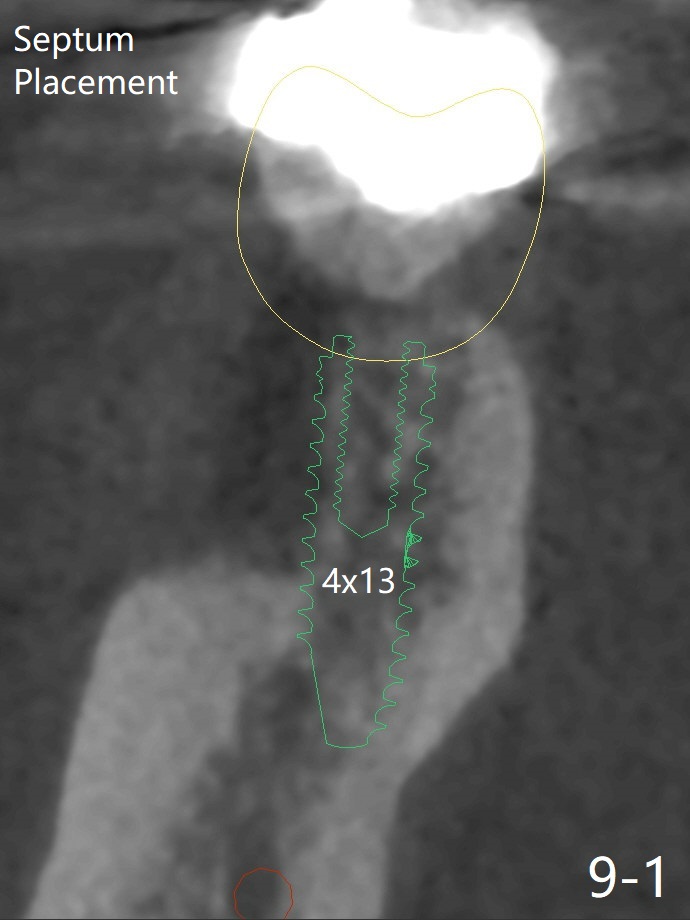
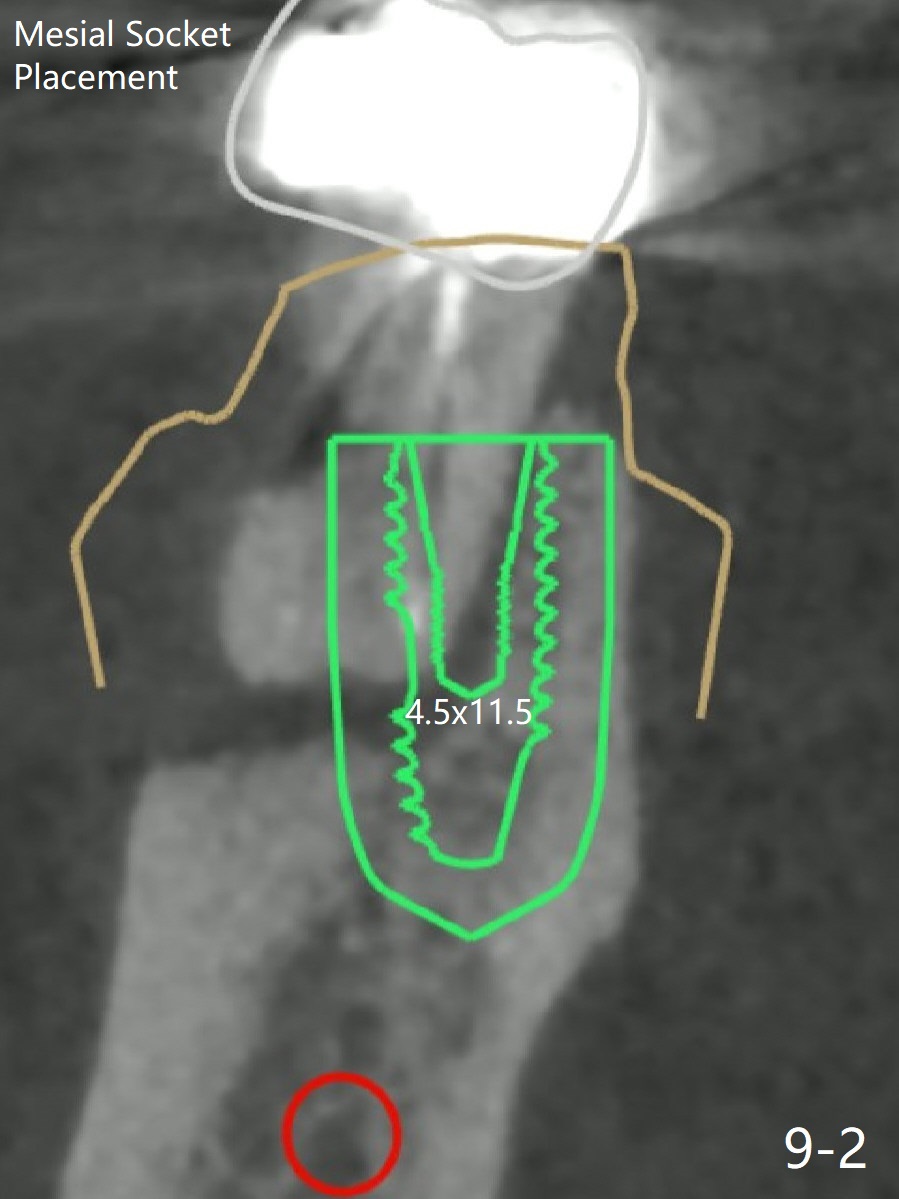
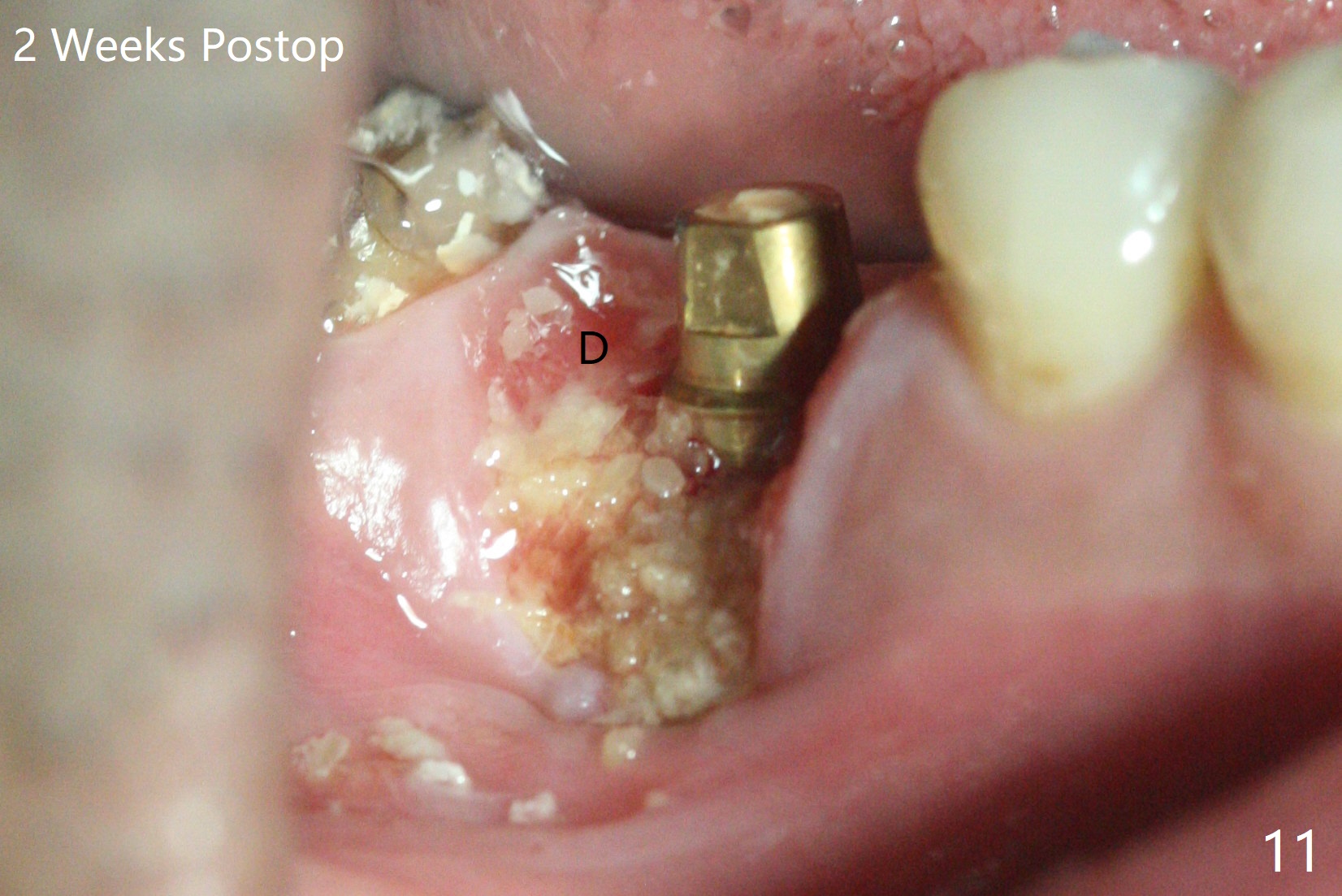
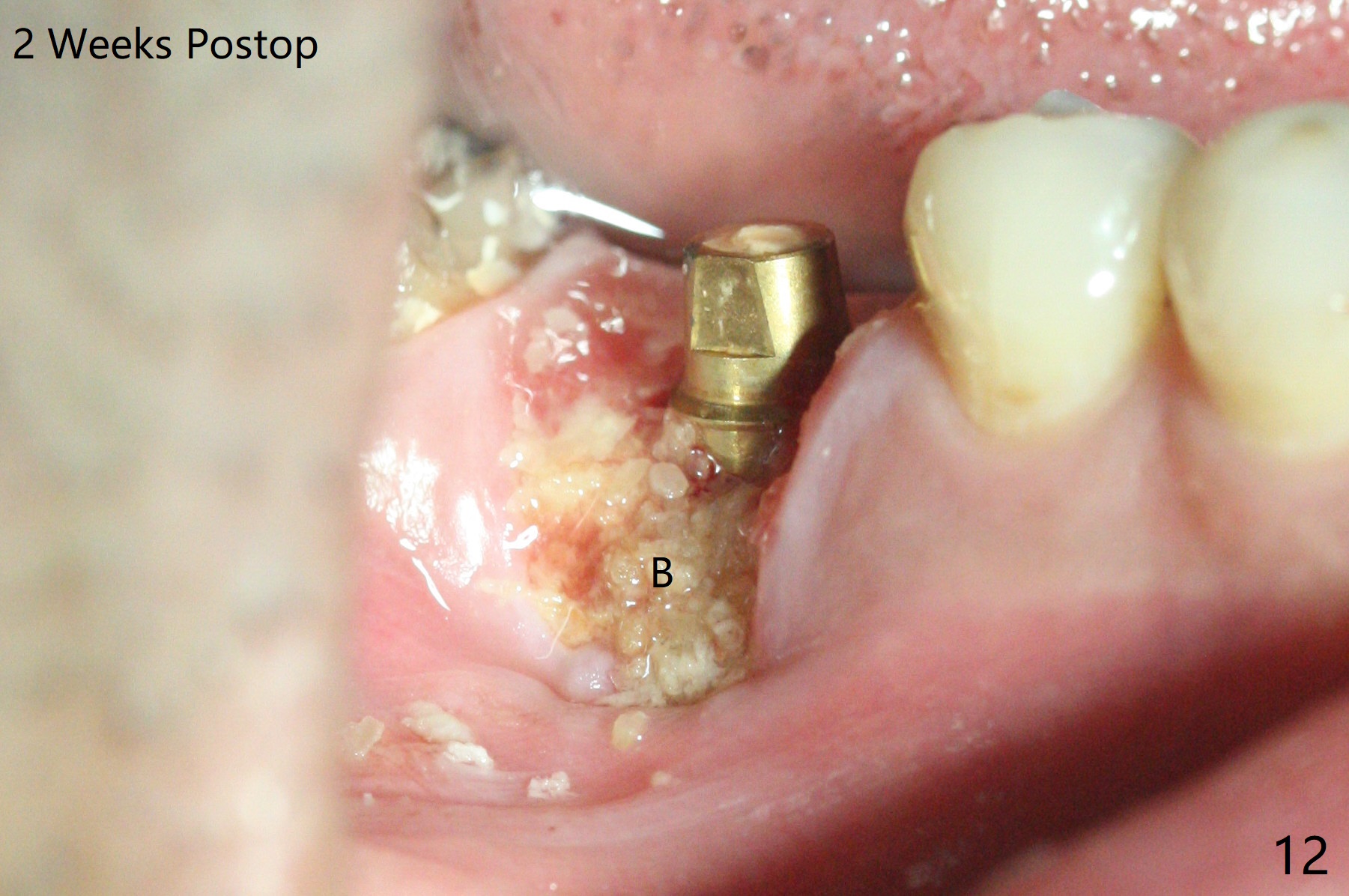
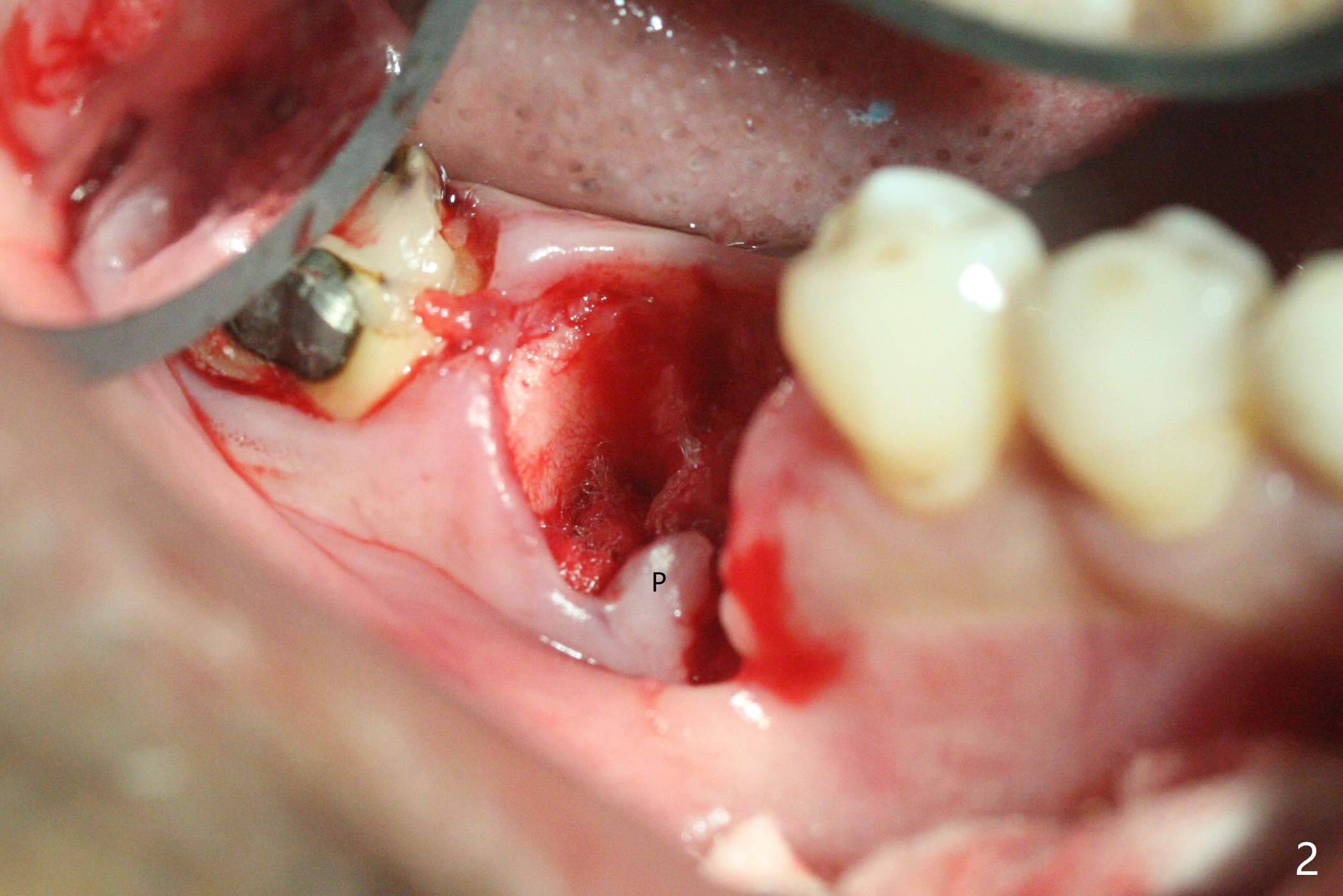
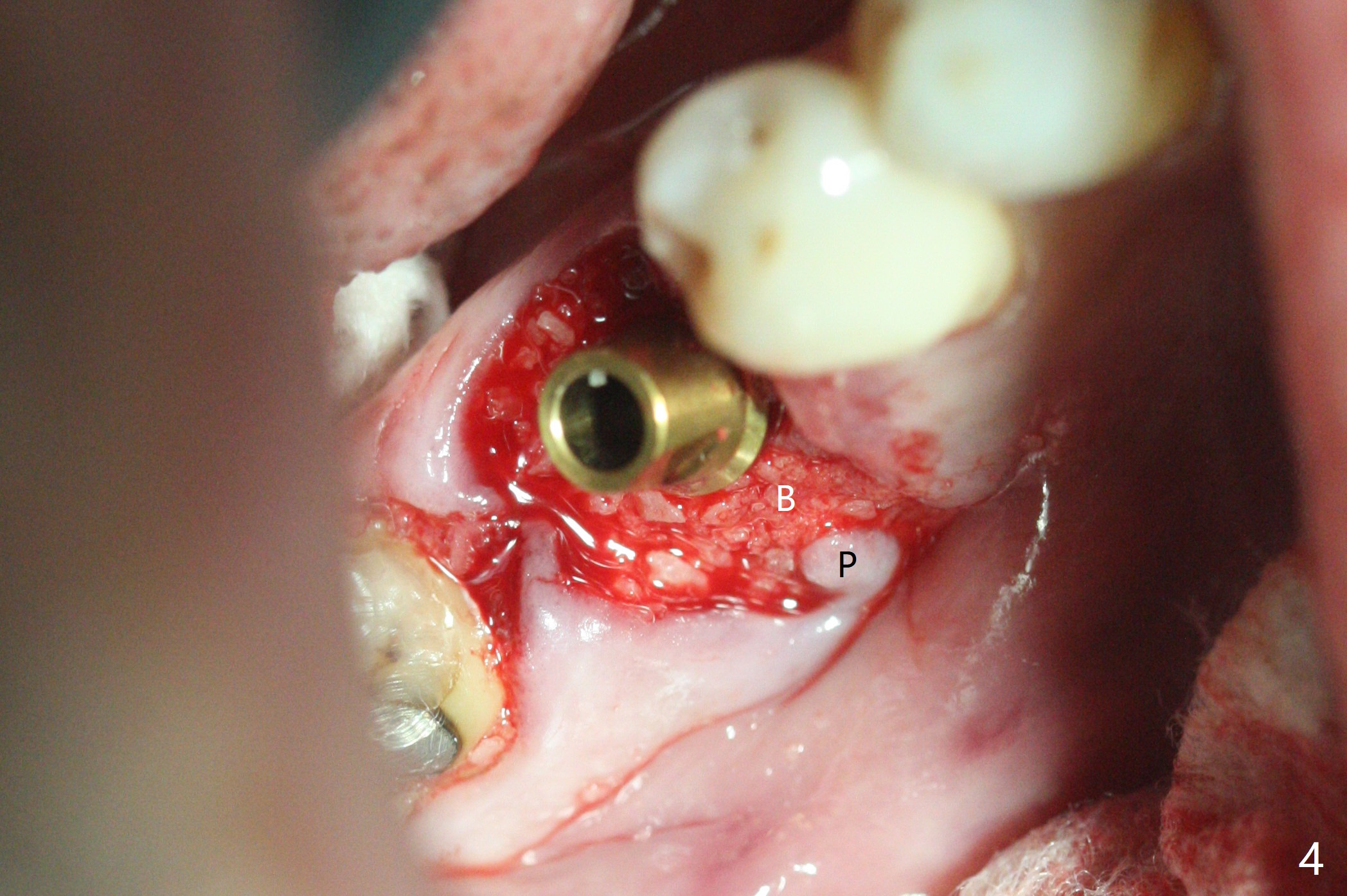
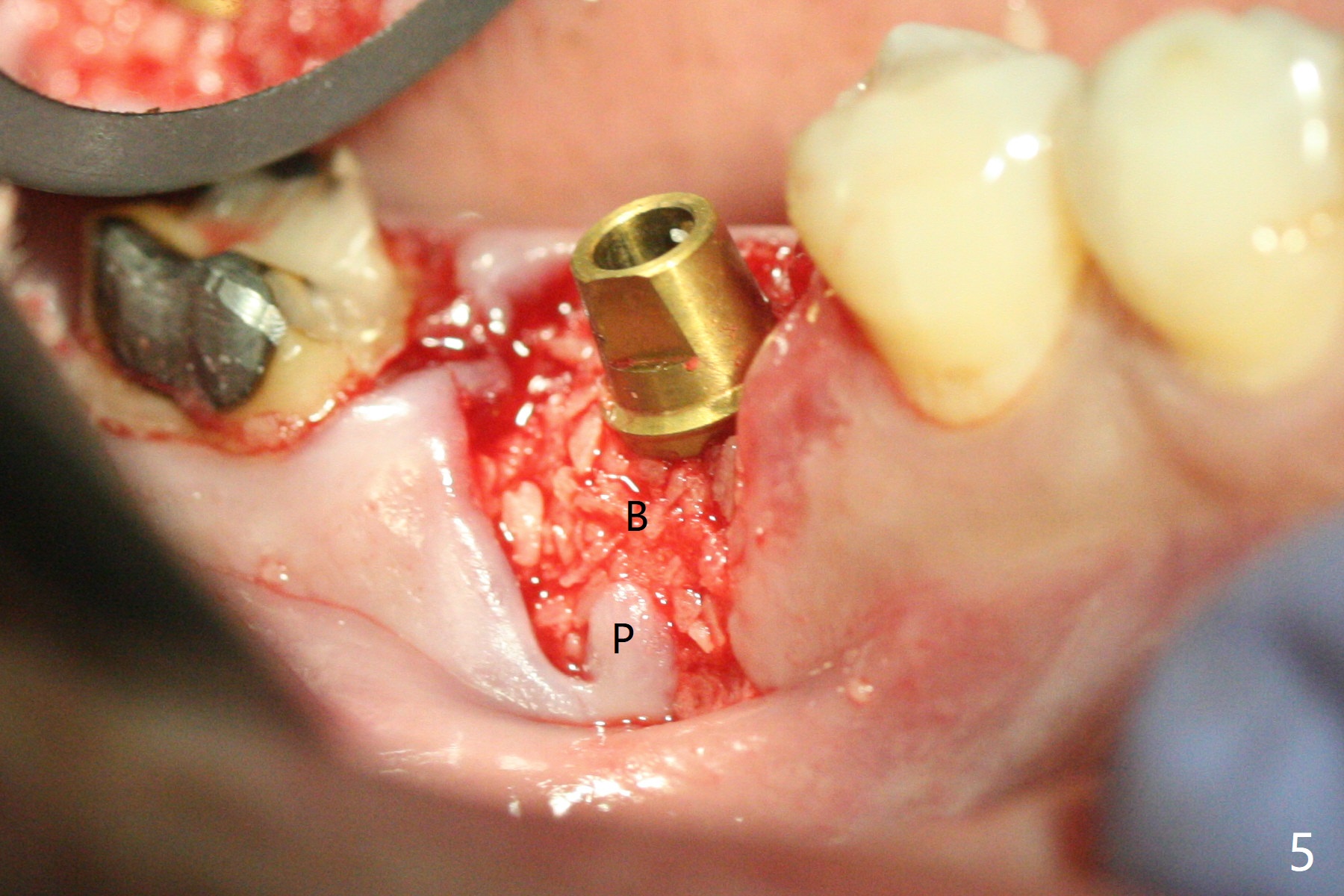
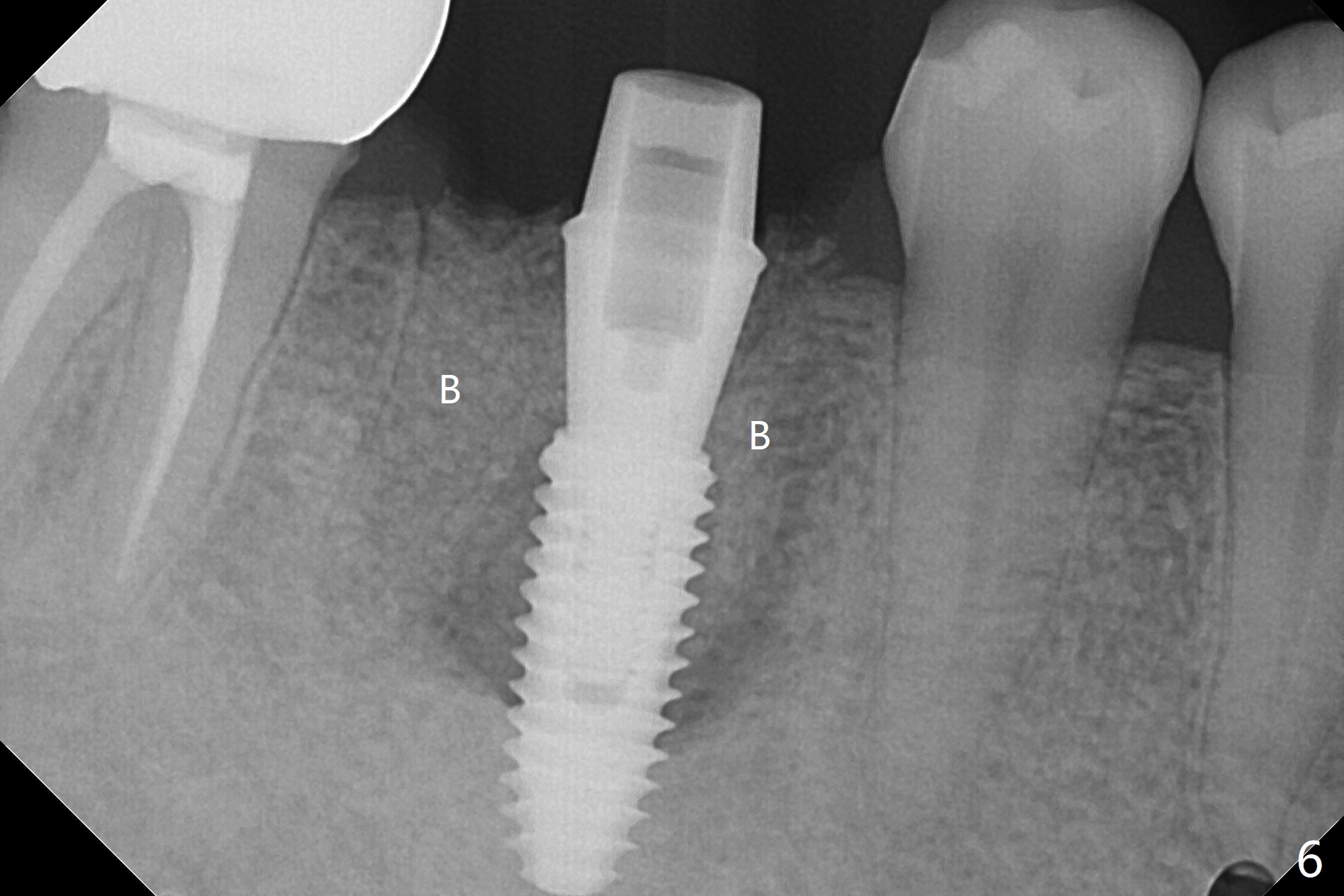
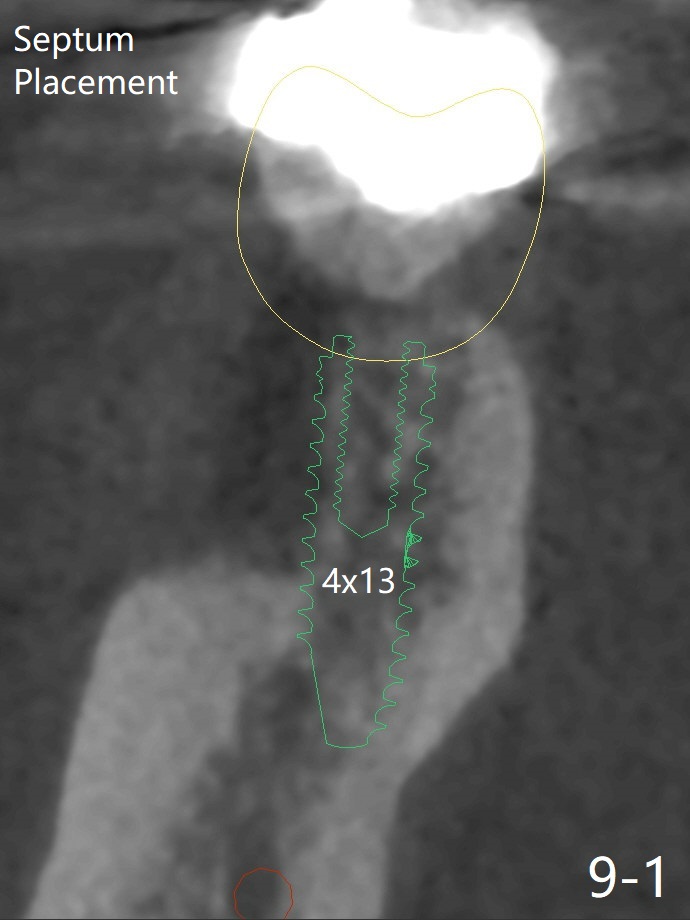
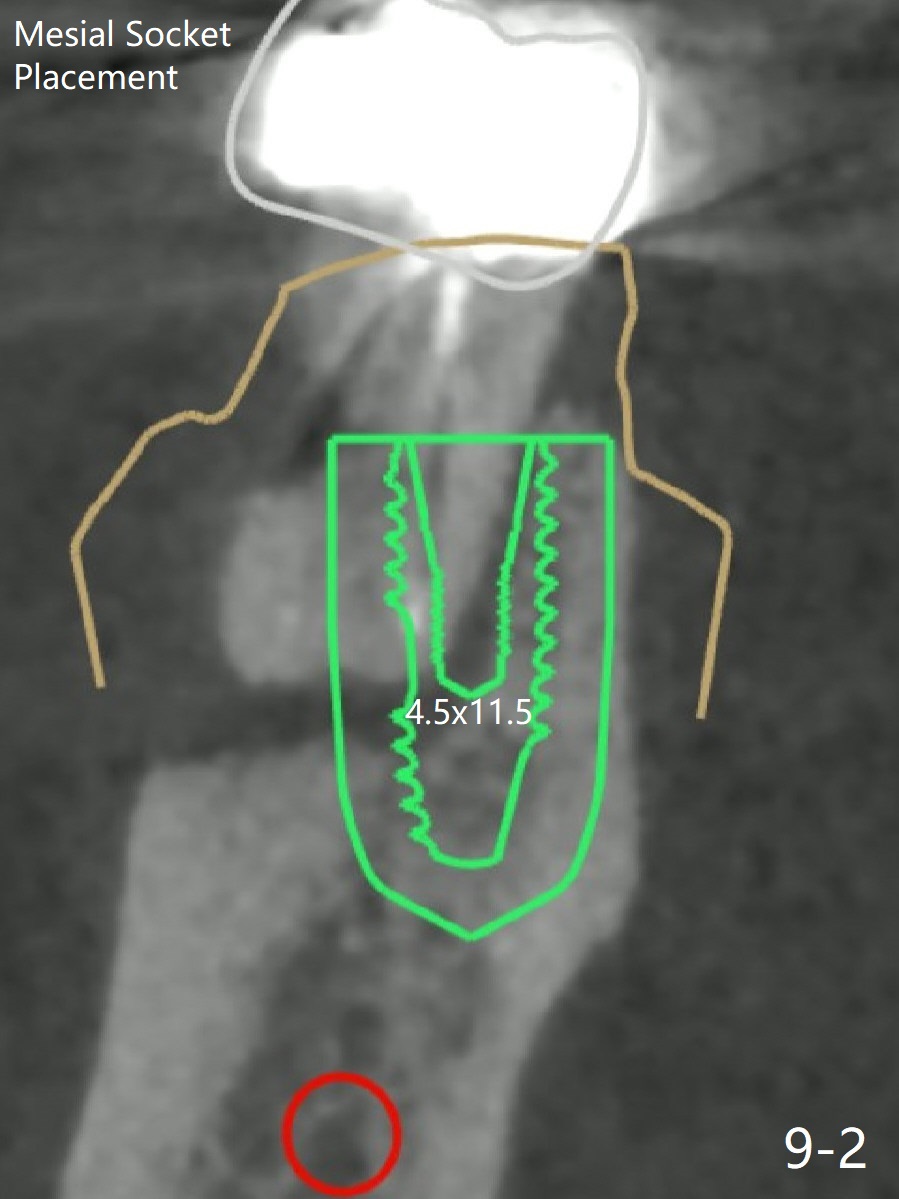
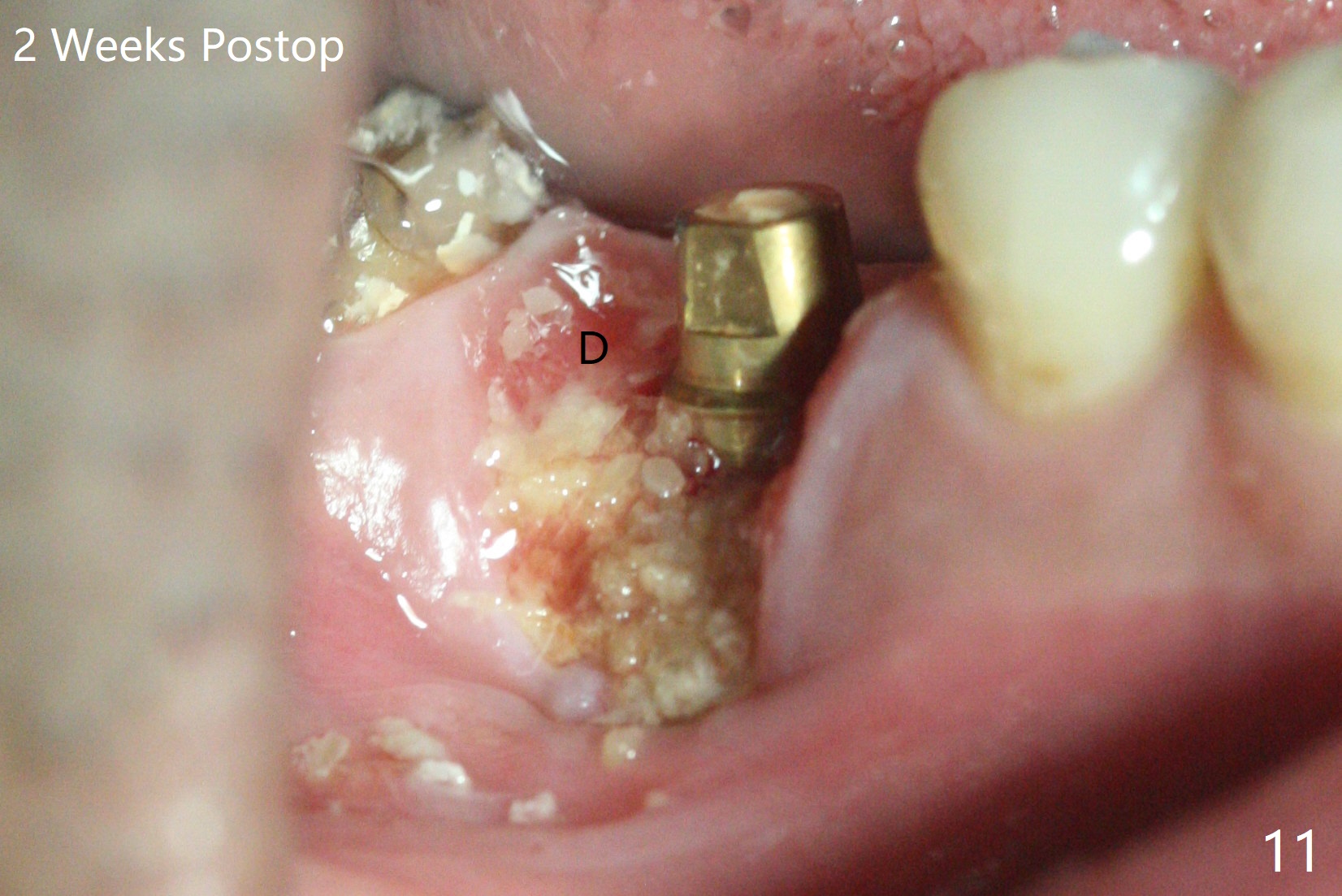
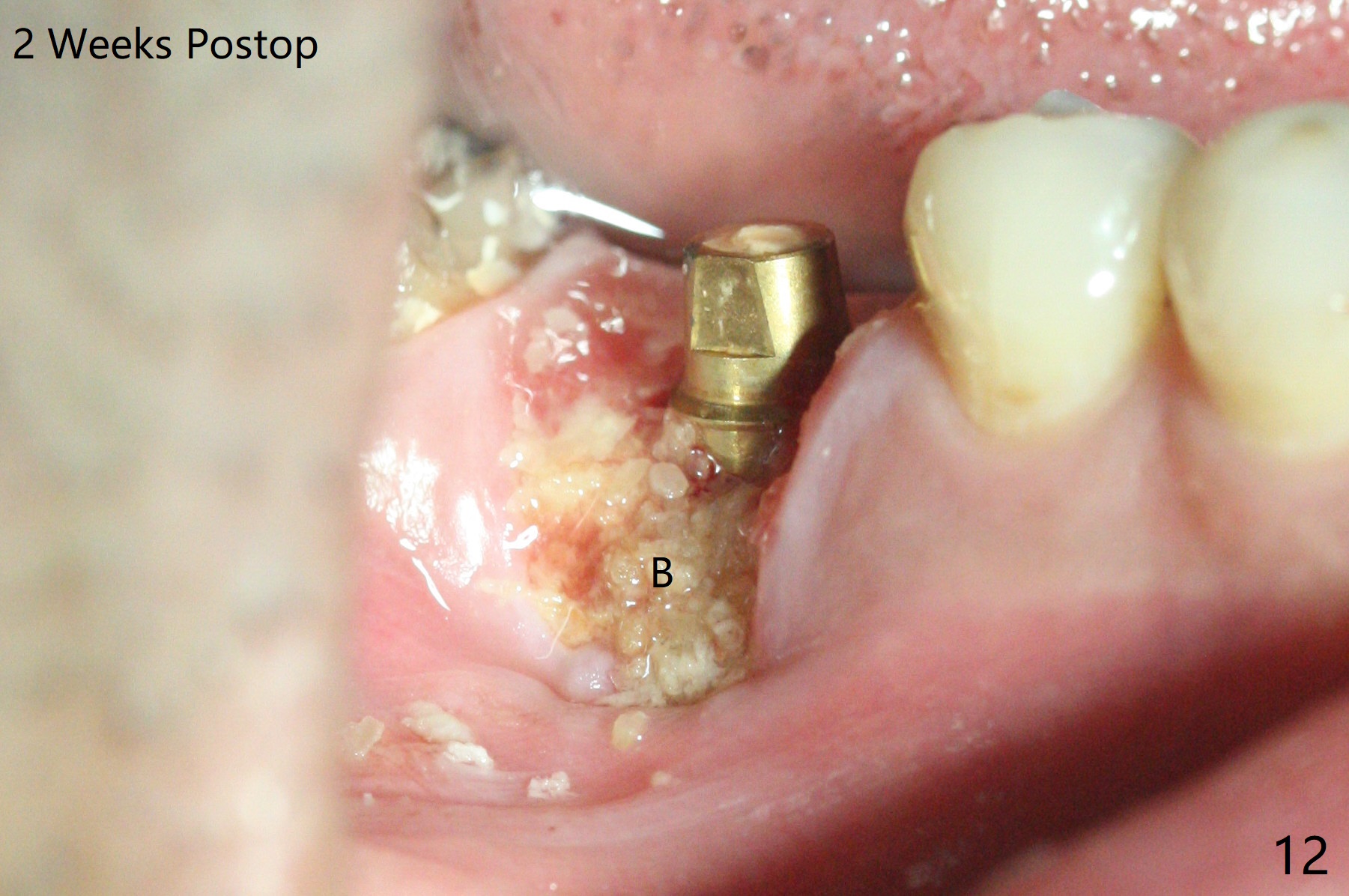
When the tooth #30 is extracted, the gingiva buccal to the septum (S in Fig.1,2 (P: papilla between the mesial and distal roots)) collapses. The latter is fixed with placement of a 4.5x11.5 mm implant (with guide), a 5.2x4(5) mm cemented abutment (Fig.3) and mixture of cortical bone (125μm – 850μm) and cortical/cancellous bone (.5-1 mm) with PRF (sticky bone, B in Fig.4-6). After placement of 2 pieces of PRF membrane over the bone graft, a temporary crown is fabricated to cover the buccal defect (Fig.7 T). Approximately 7.5 mm of the buccal threads are covered by the thick layer of bone graft (Fig.8 B). It is amazing to expect that the bone graft will turn into the buccal plate. It would be better if a narrower implant (4 instead of 4.5 mm) were placed more lingually or there were < 4 mm implant thread exposure (Fig.9). The gingiva reacts to the provisional nicely 7 days postop (Fig.10). The provisional will be removed for modification in 1 month. The patient complains of bad smell from the provisional 2 weeks postop. The provisional is removed. The distal socket (Fig.11 D) is healing, whereas the buccal bone graft (Fig.12 B) seems not have been vascularized. Pedicled flaps (I) should be transferred to cover the buccal bone graft. The margin of the provisional is polished, becomes short, and covered by periodontal dressing, which dislodges 2 days later. One week later, granulation tissue is forming apically with use of oral antibiotic and water jet (Fig.13 *). The bad smell reduces. The superficial loose bone graft changes colar and becomes detached 1 month 10 days postop. The temporary crown with the shortened buccal shelf is reseated for self cleansing or reapplication of PRF if needed (Fig.14).
Return to No Deviation Shield Removal
Xin Wei, DDS, PhD, MS 1st edition 05/13/2020, last revision 02/14/2021