








%20trimmed%20before,%20flat%20surface%20linguodistal.jpg)
 |
 |
 |
 |
|
 |
 |
 |
||
 |
|
 |
||
 |
 |
 |
 |
|
 |
 |
 |
||
 |
 %20trimmed%20before,%20flat%20surface%20linguodistal.jpg) |
|||
Bone Graft Before Implant M
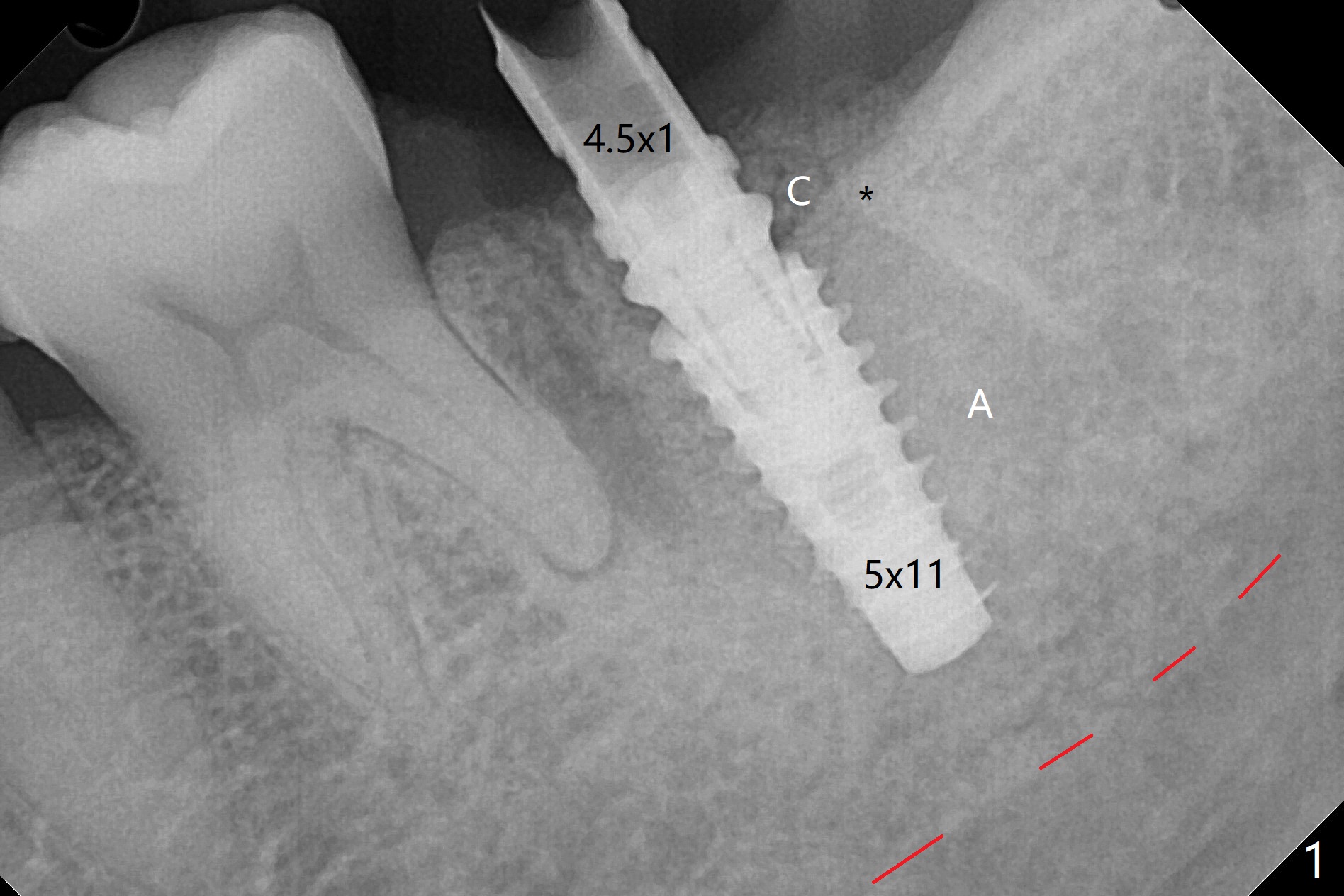
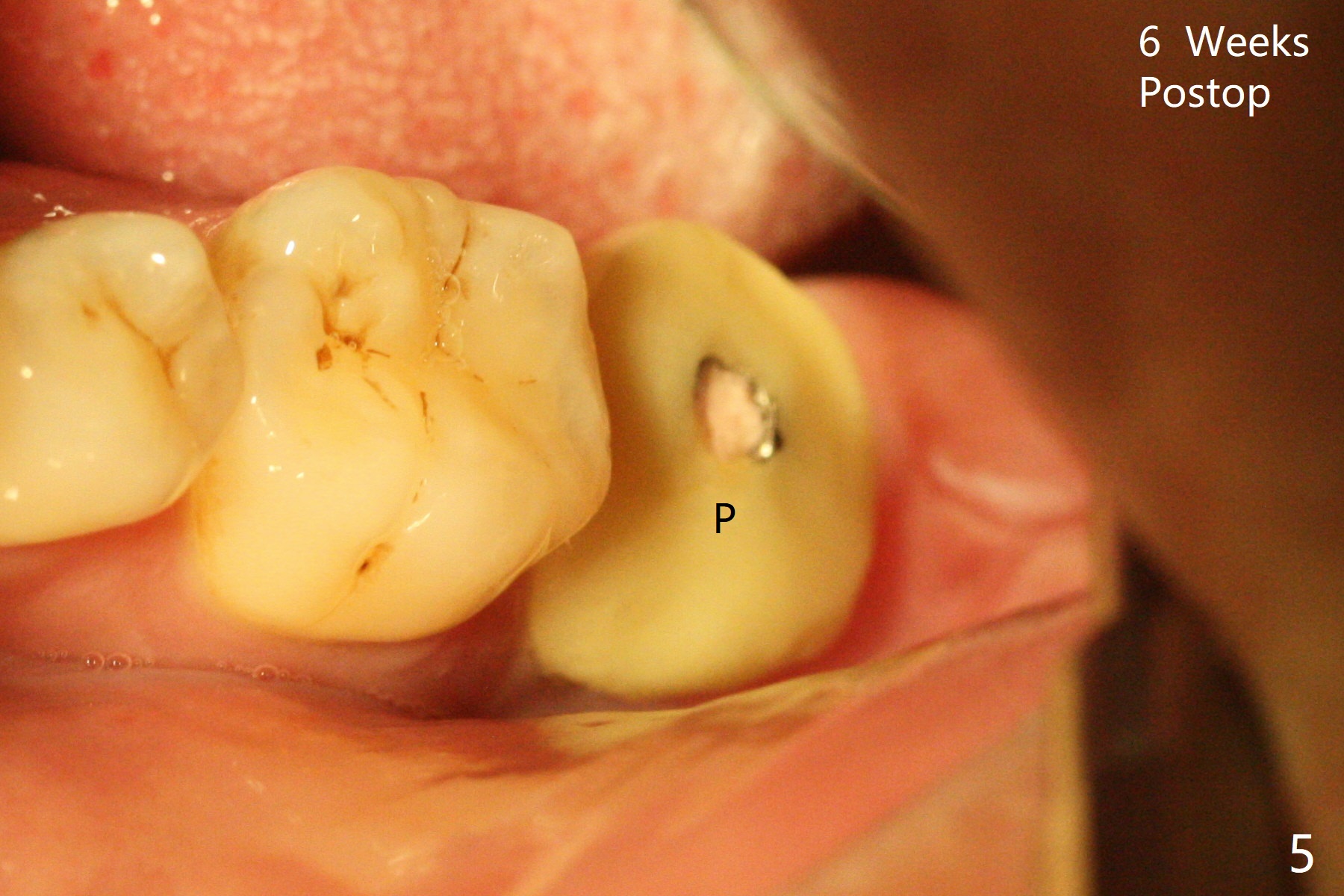
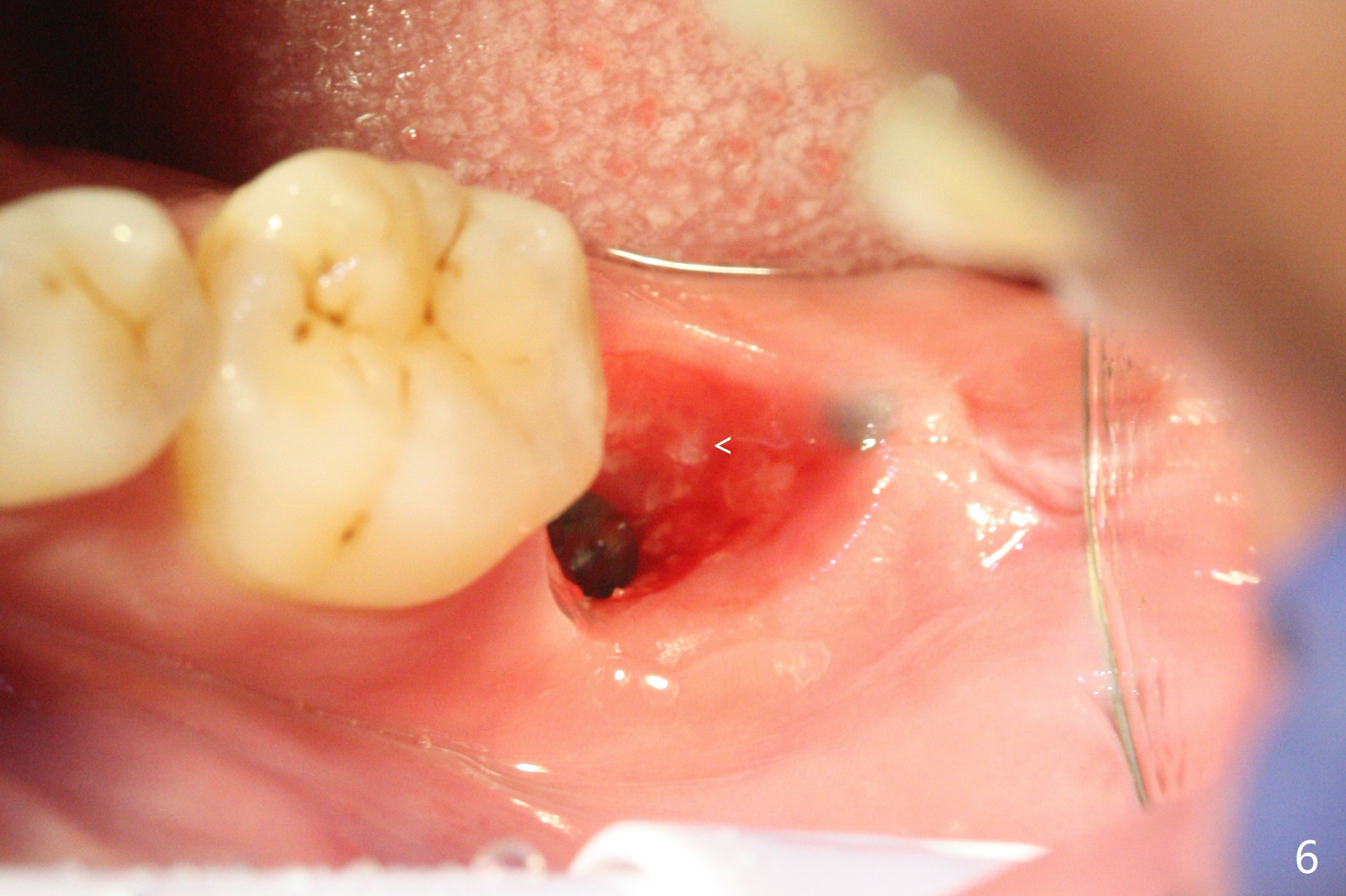
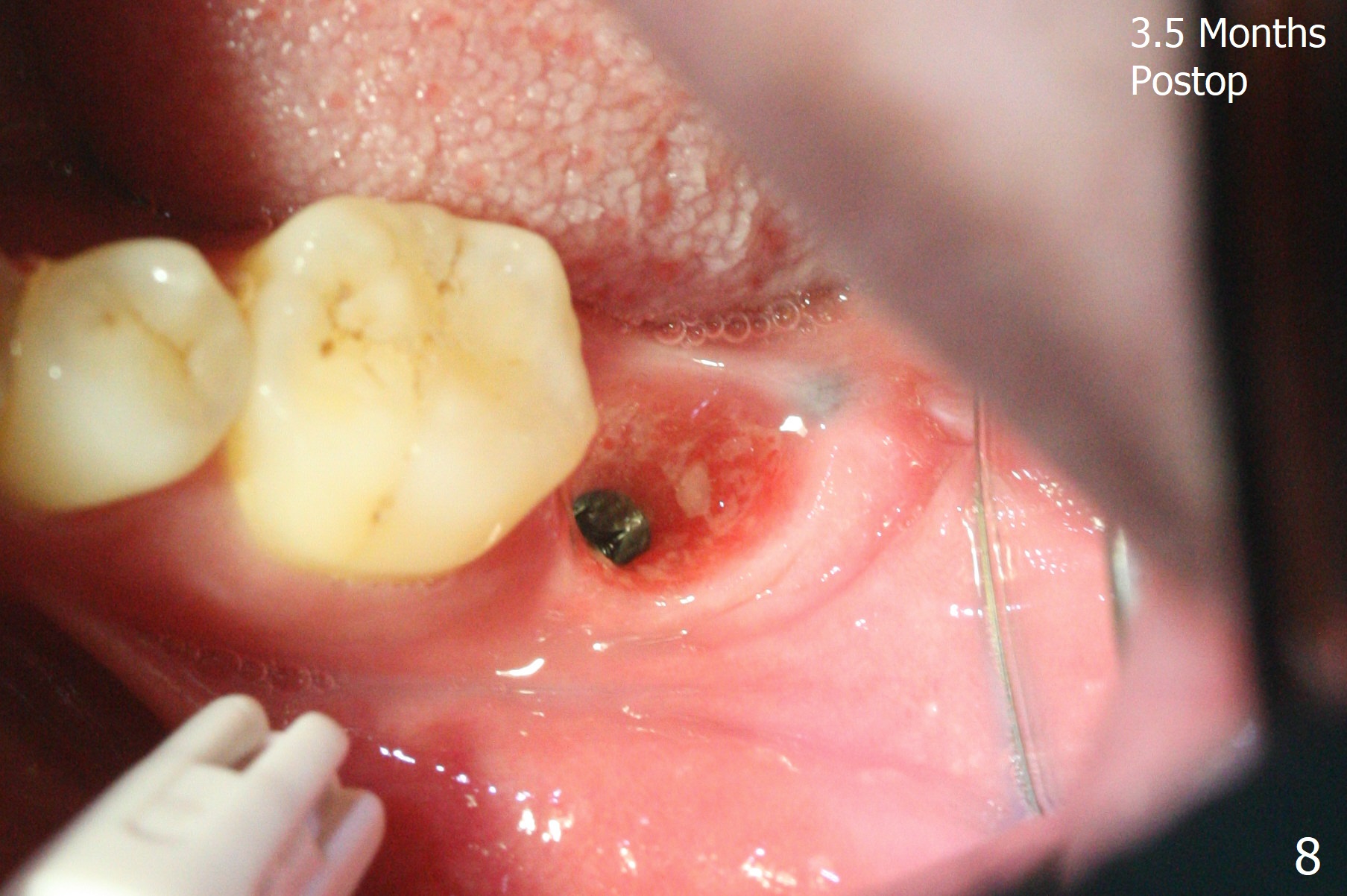
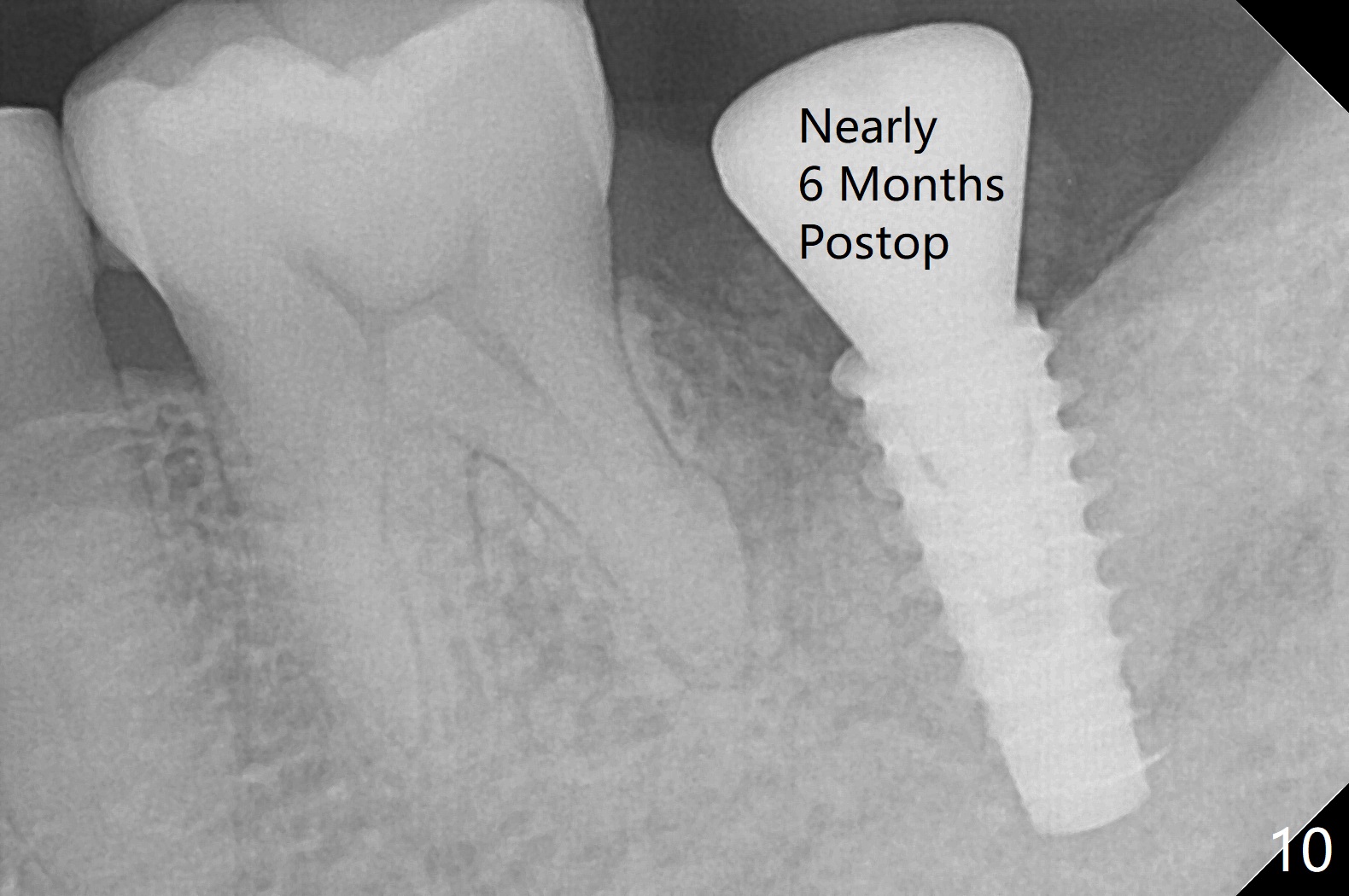
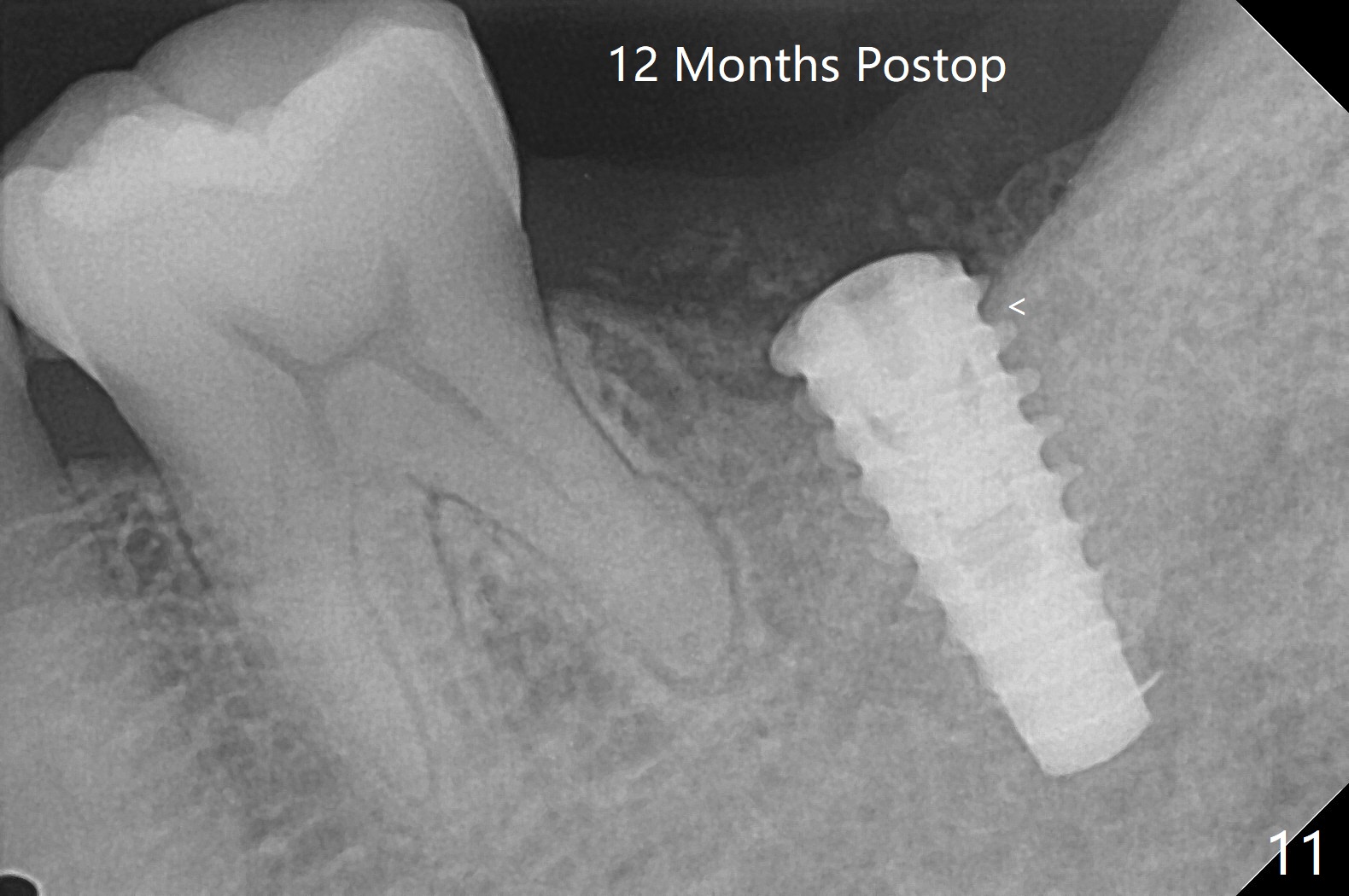
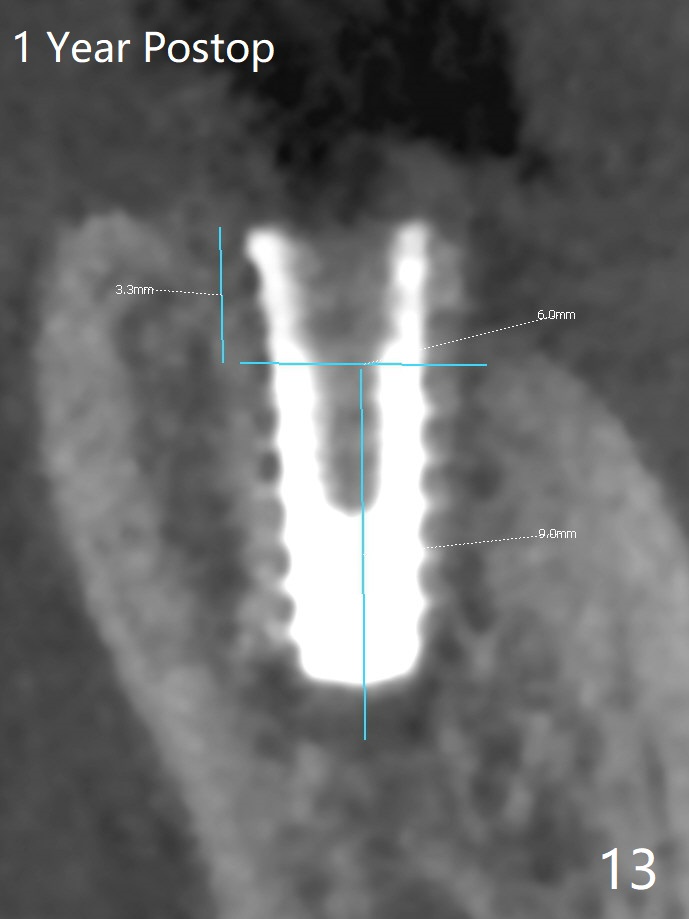
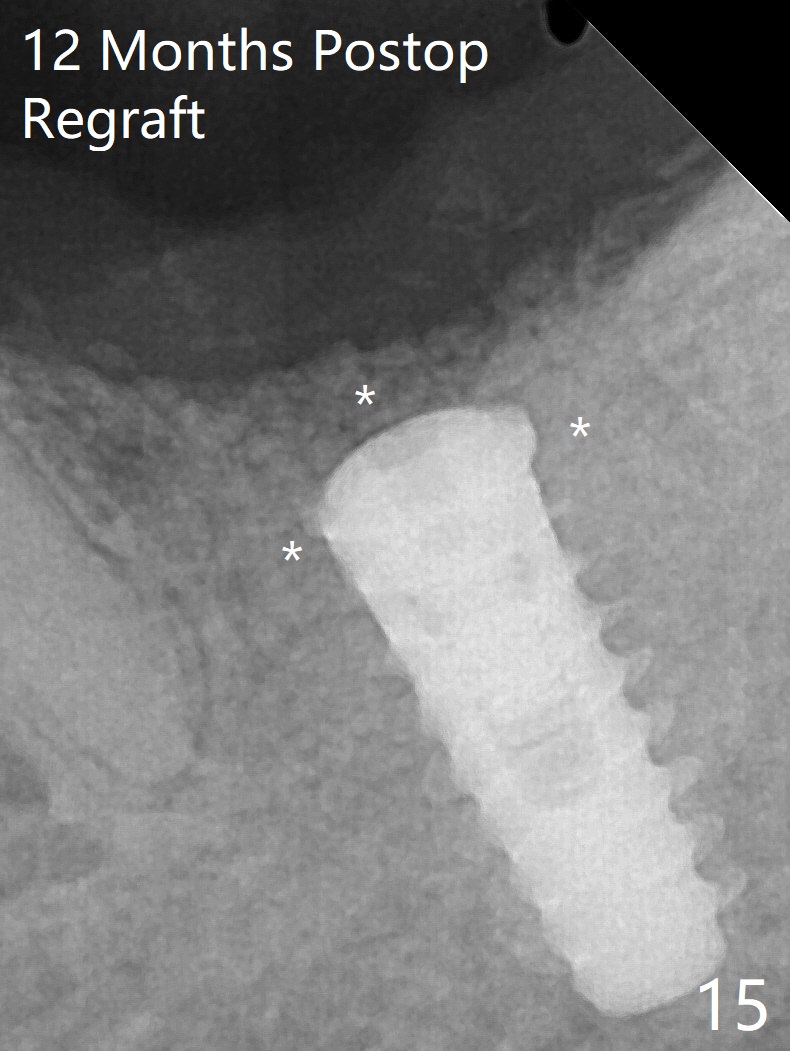
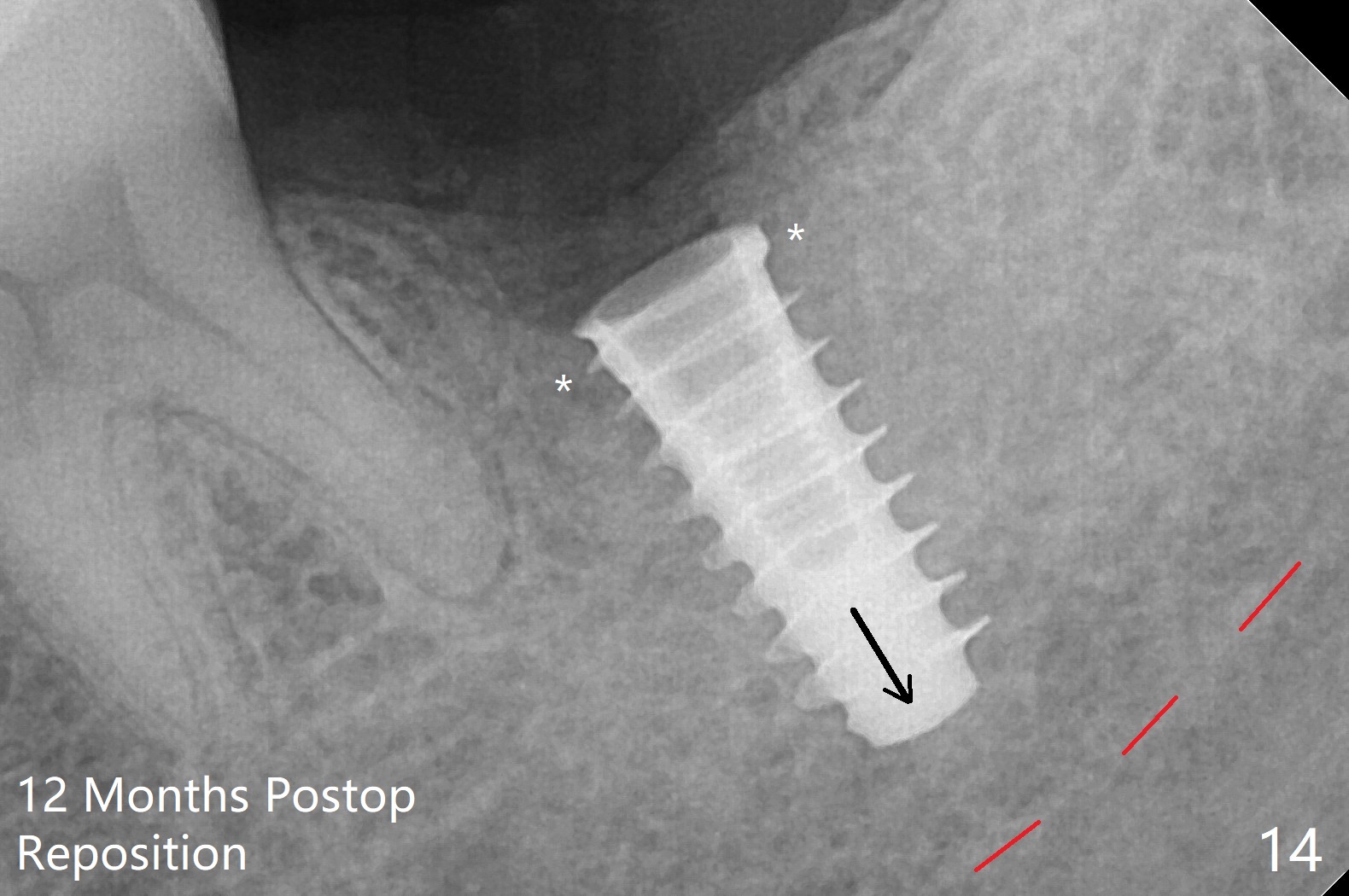
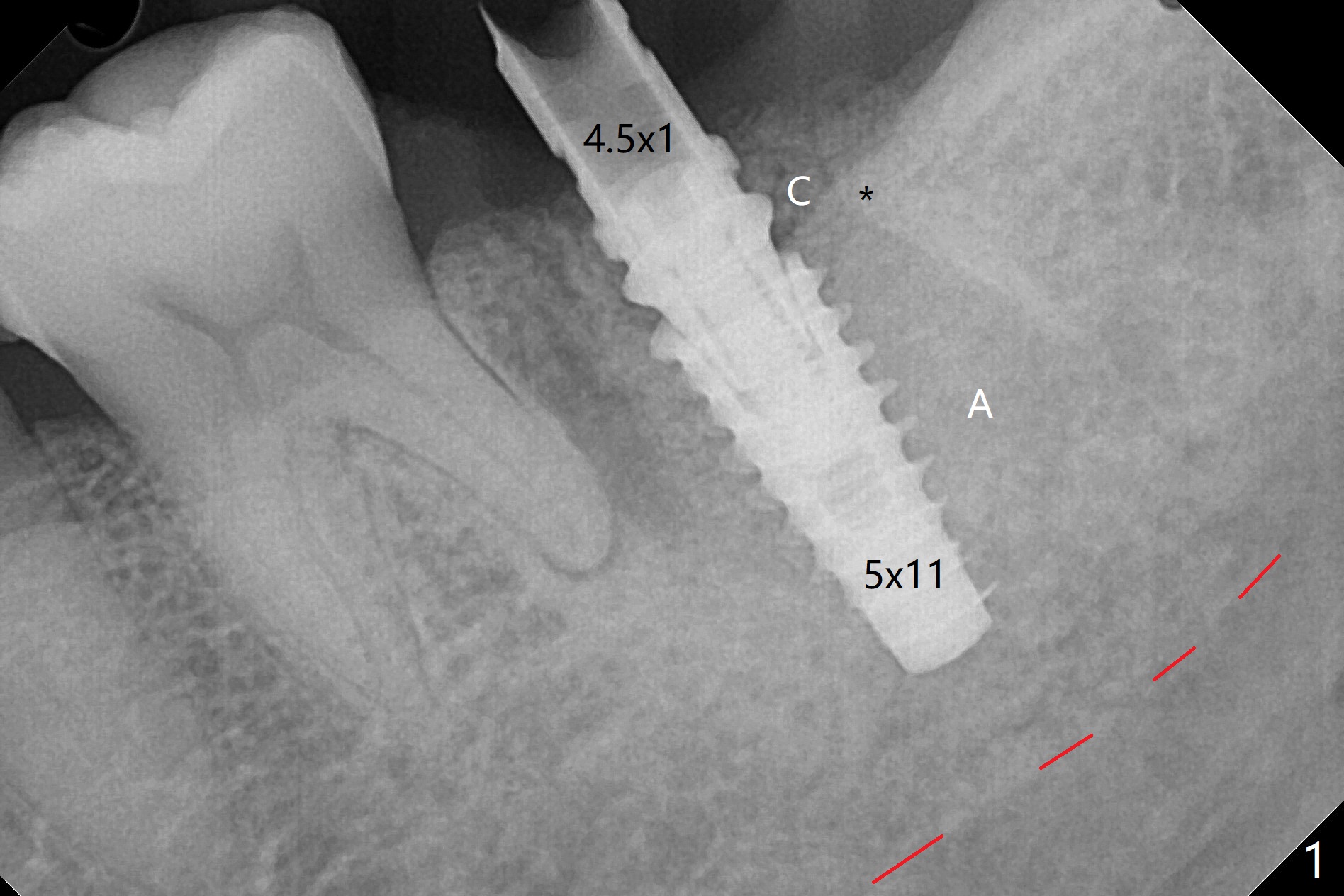
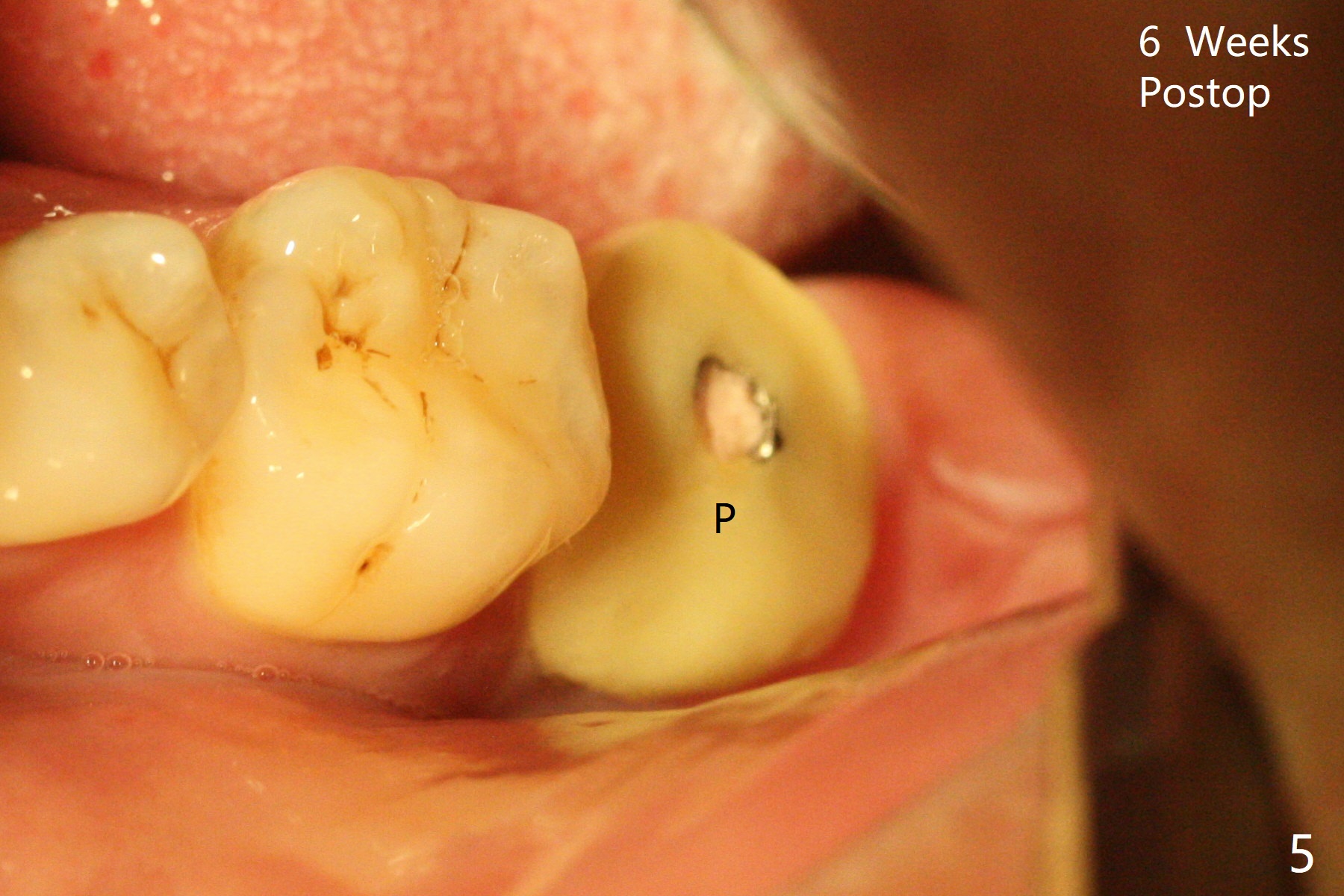
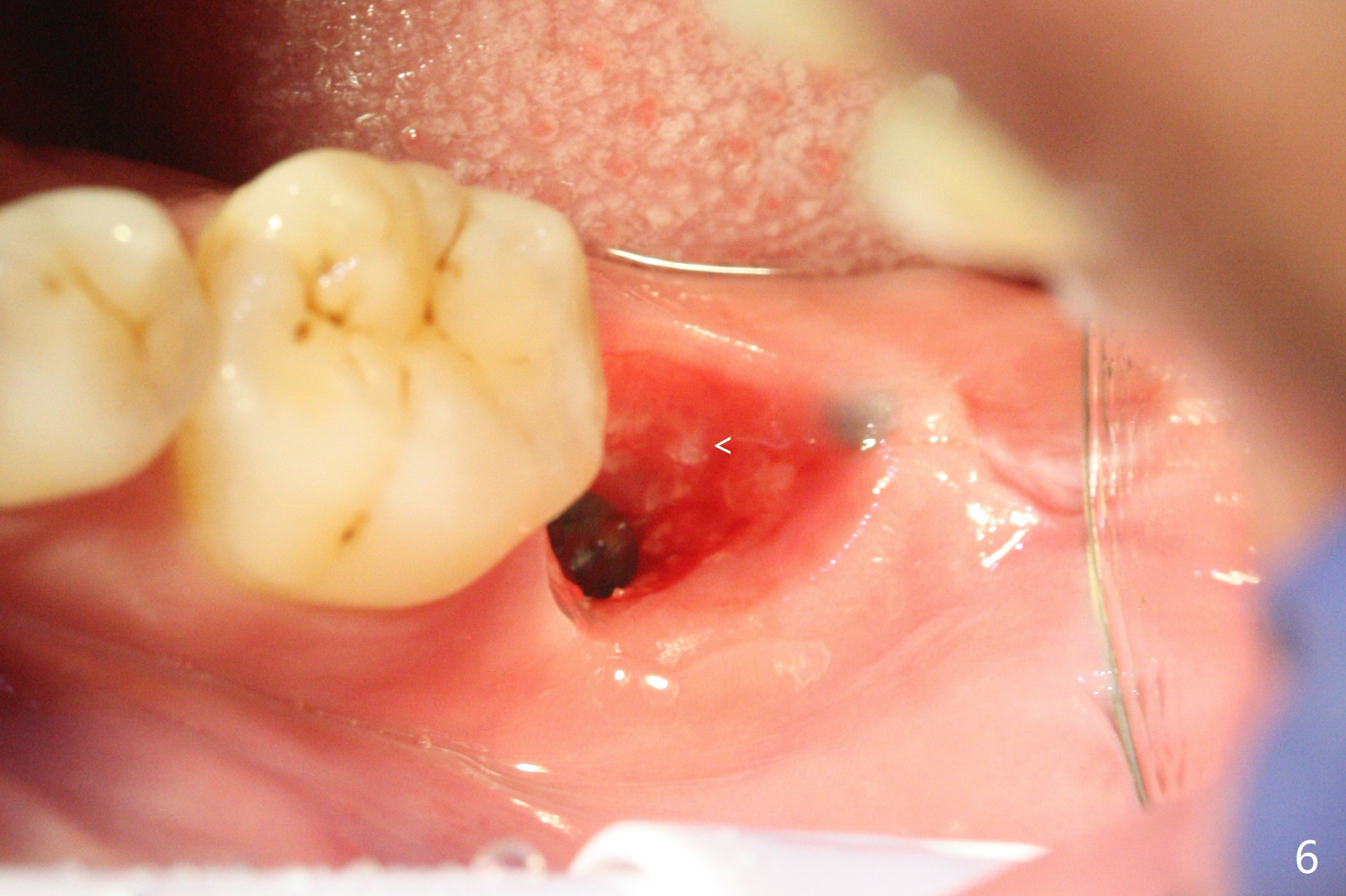
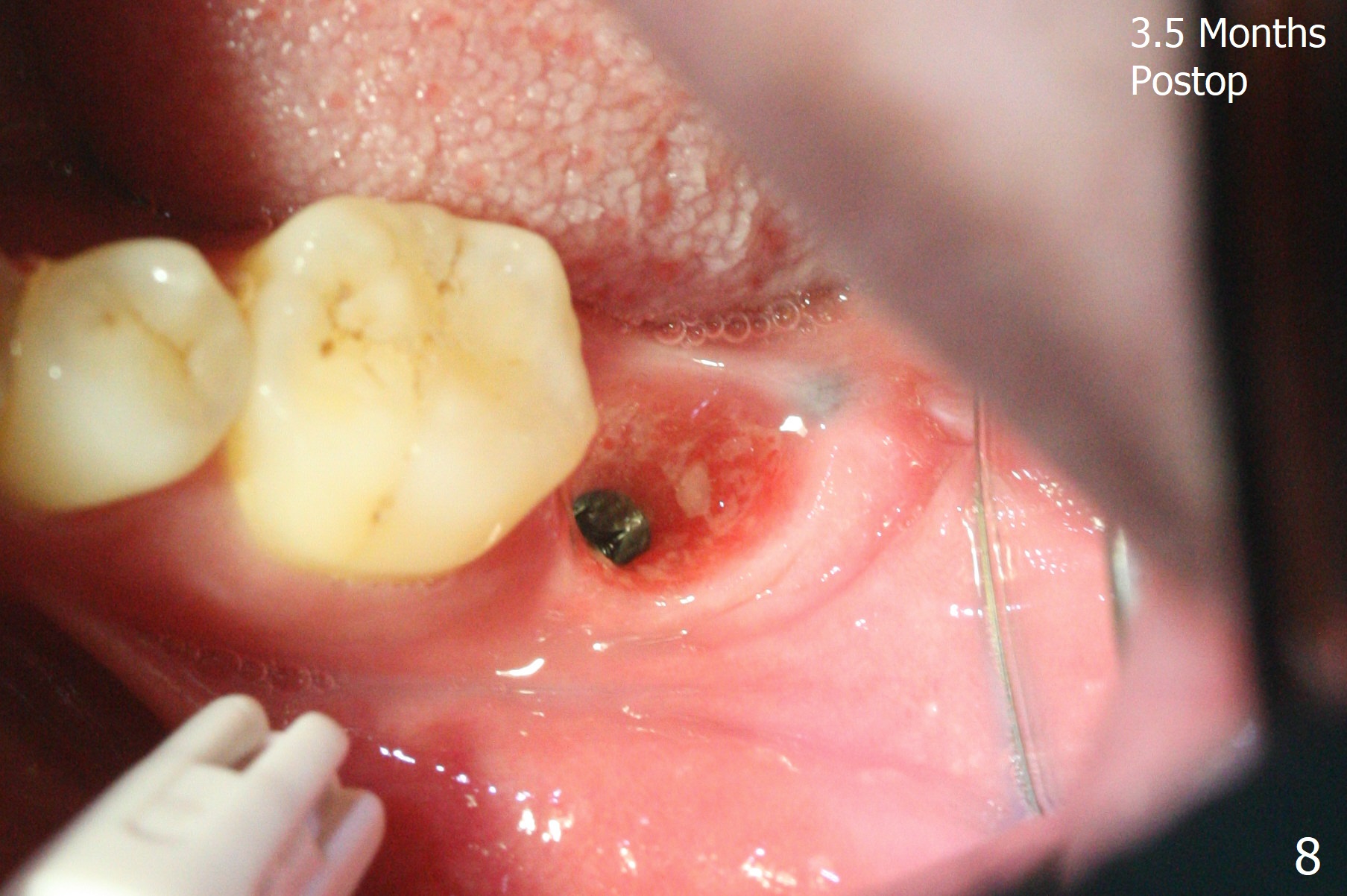
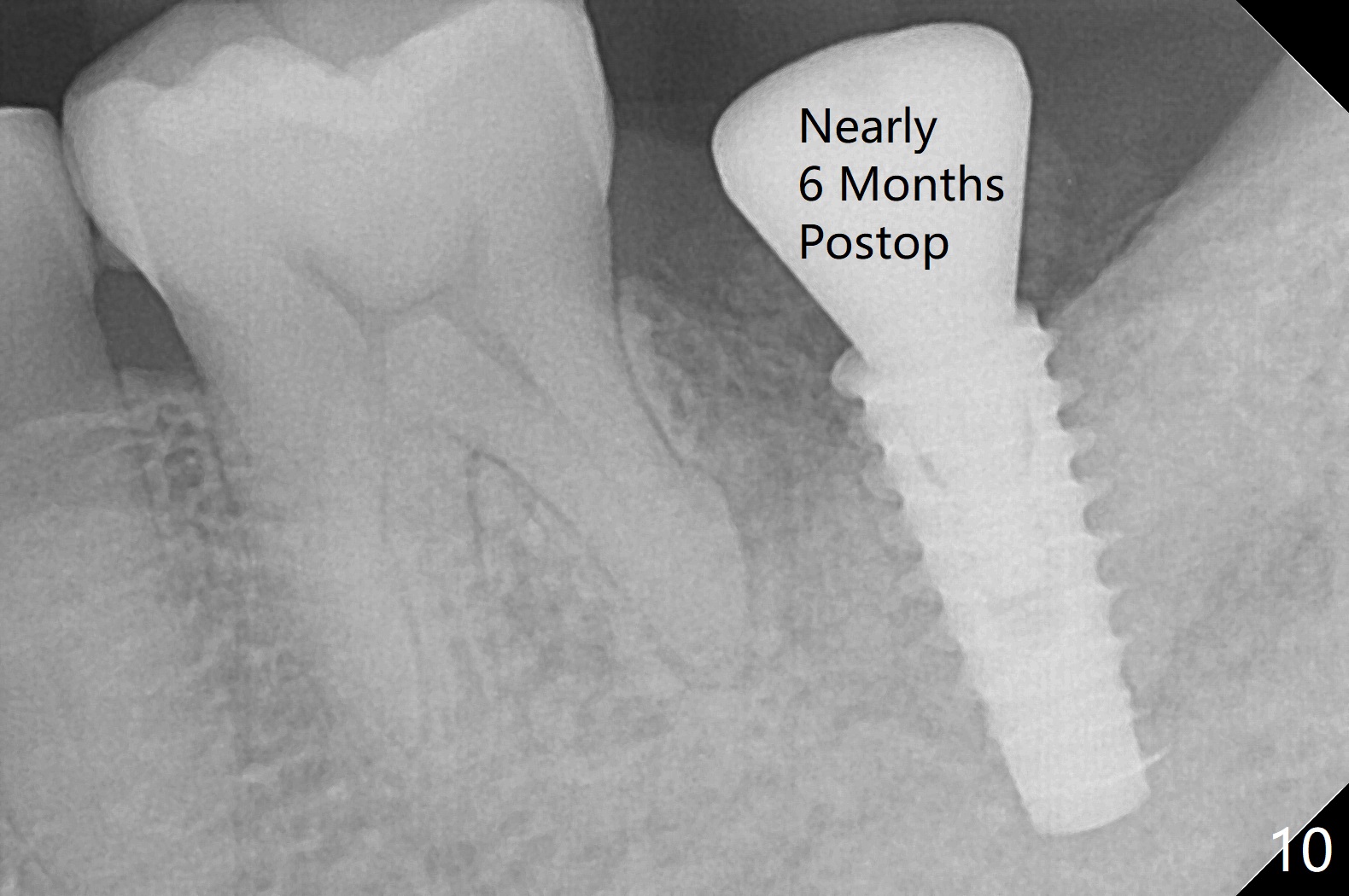
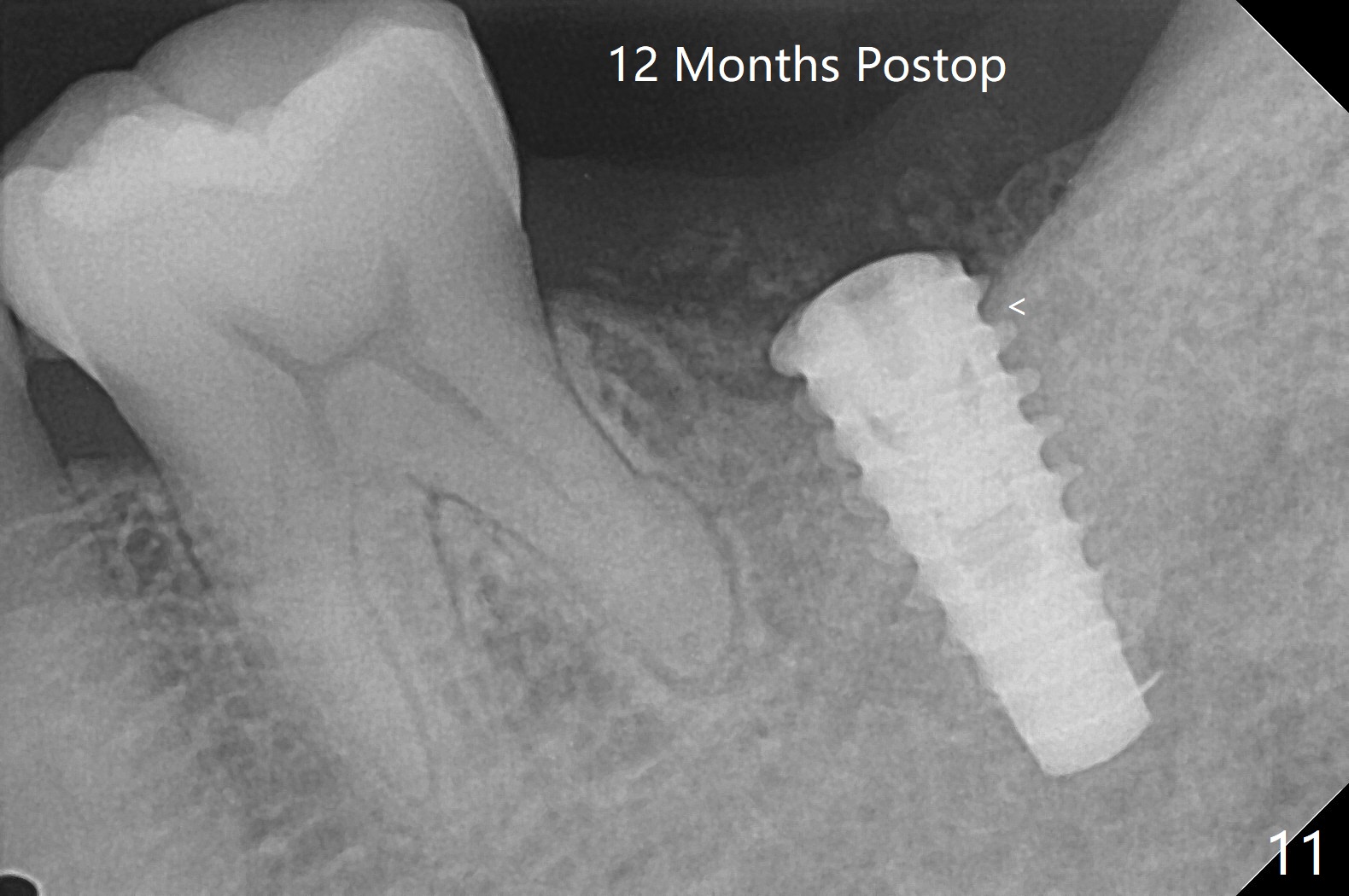
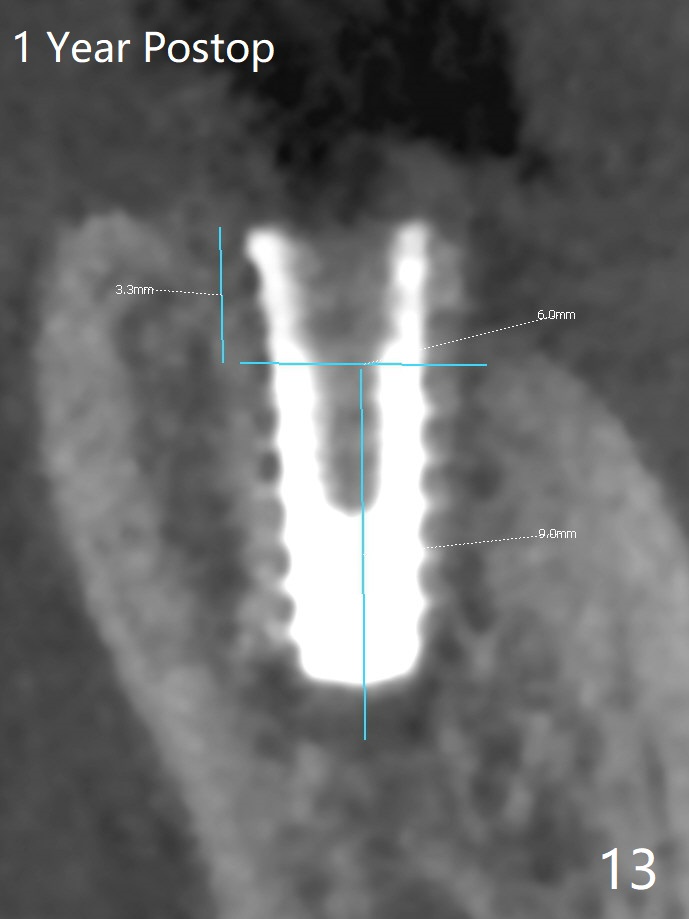
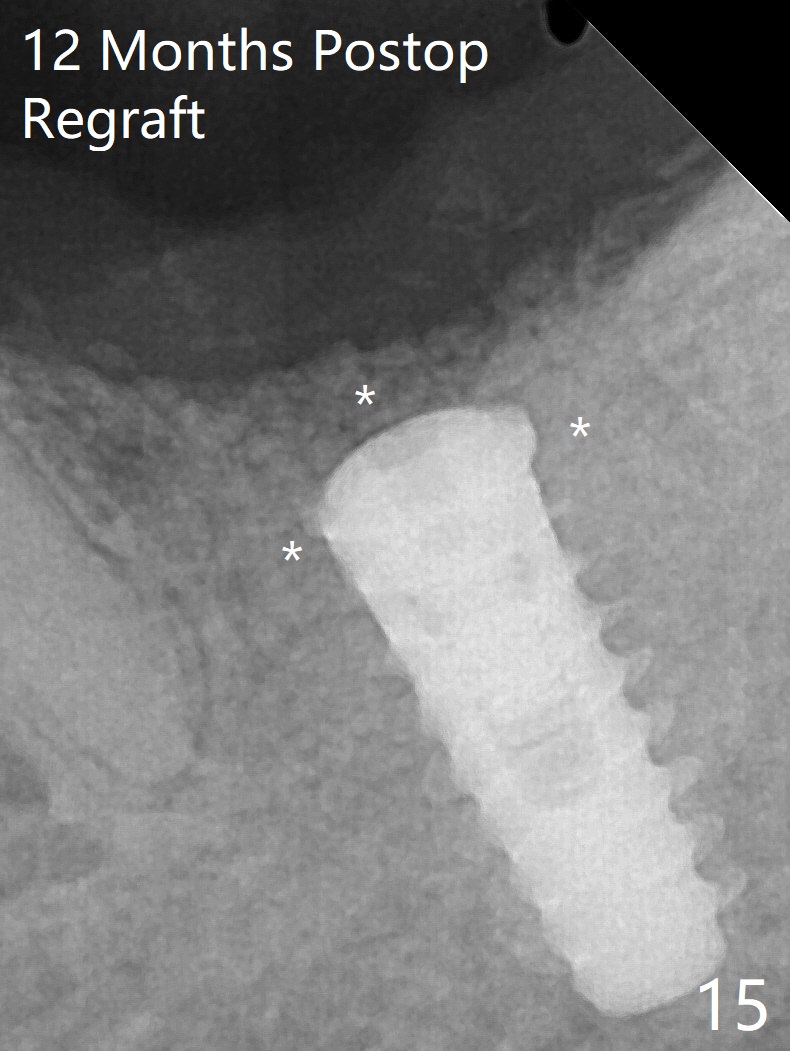
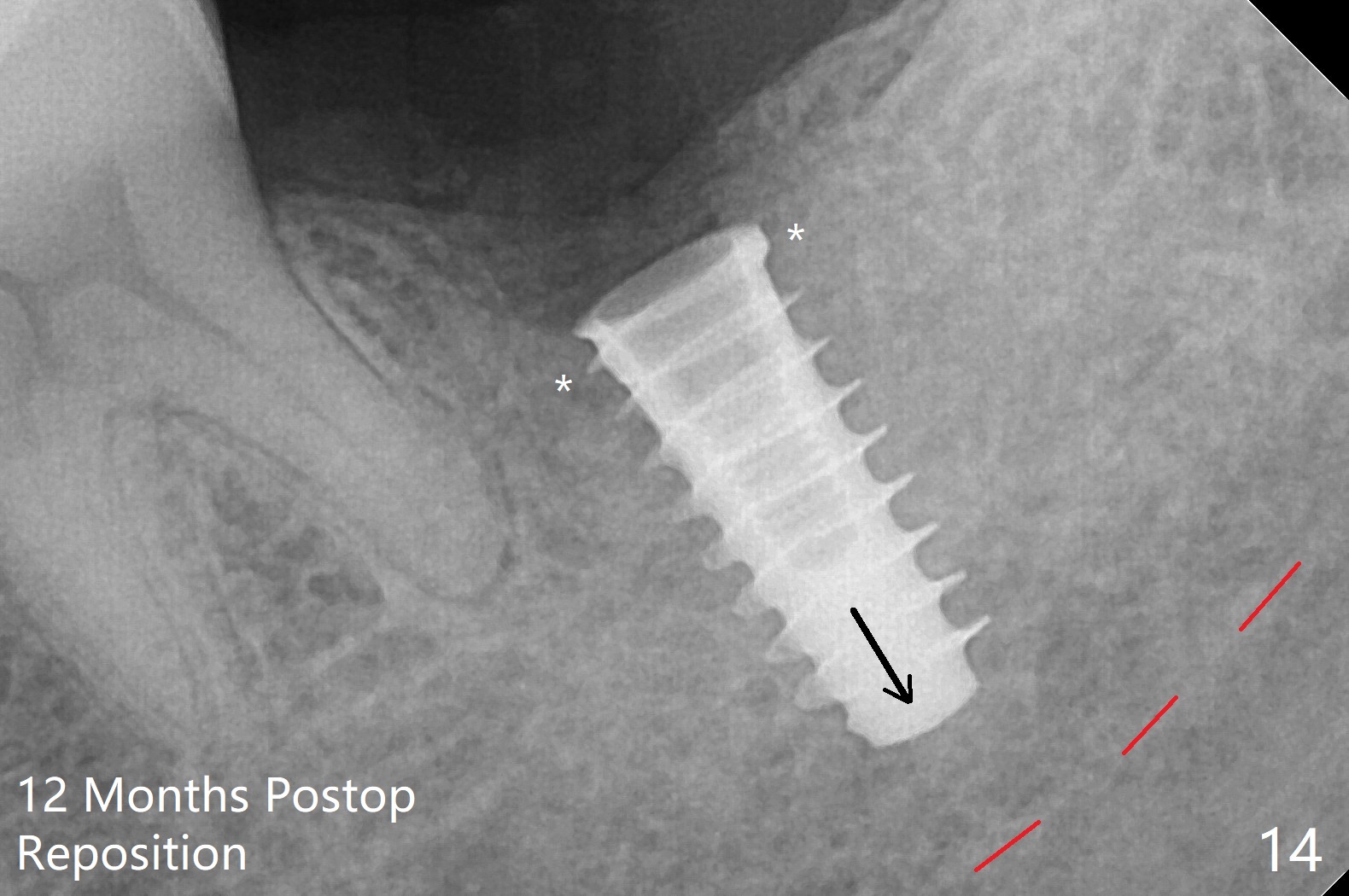
After placement of a 5x11 mm implant and cover screw at #18, allograft mixed with PRF (sticky bone) is placed in the peri-implant space, but it appears that bone density in the apical region (Fig.1 A) is lower than that in the coronal one (C) because of a constriction between the implant and the distal crest (*). Ideally the undercuts (Fig.2 *) of the extraction socket (black area) should be identified. Place bone graft in the undercuts (Fig.3 red circles) after osteotomy (white outlines) and before implant placement! A 4.5x1 mm temporary abutment is placed for an immediate provisional. The 2nd shortcoming of this case is that the implant is placed a little buccal. The papilla mesial to the immediate provisional (Fig.4 P) looks normal 4 days postop (no food impaction is expected when a final restoration is cemented). Additional acrylic (*) was placed to close a buccal gap when the provisional was seated with the temporary abutment. The patient reports loss of a piece of material in 4 days. It must be the additional acrylic, since it is absent 6 weeks postop (Fig.5). The provisional (Fig.5 P) looks wide, probably related to post-extraction gingiva and bone atrophy (Fig.6, 7 *). Bone graft (Fig.6 <) becomes a component of the gingival cuff. The provisional is re-trimmed for better oral hygiene. The gingival cuff is basically healthy 3.5 months postop, although the temporary abutment is loose and the implant is tender to rewinding and winding (Fig.8). The implant seems to remain non-osteointegrated 3.5 months postop (Fig.9). Although the bone density around the implant increases nearly 6 months postop (Fig.10), the implant remains tender when a 5x4(4) mm pair abutment is tightened. The healing abutment is reused. The bone density around the implant increases 11 months postop (Fig.11). Uncover is done with 5.5 mm profile drill. One month post uncover (12 months postop), the implant remains unstable (Fig.12). Prepare sticky bone x1. Make incision for exploration, including retightening the implant after Titanium brush and H2O2 Q-tip rubbing. If needed, a larger and shorter UF implant is a replacement (Fig.13). The implant is removed, cleaned with Titanium brushes and H2O2 in vitro and repositioned 12 months postop (Fig.14: arrow (gaps: post granulation tissue removal)). The gaps are regrafted with sticky bone and covered with PRF membrane and Cytoplast. Although the patient complains of severe pain the first 2-3 postop, the wound is apparently healing 12 days postop. The Cytoplast is exposed asymptomatic 5 weeks postop (Fig.16) and removed (Fig.17). The wound appears to have healed without loss of the bone graft (Fig.18).术后四个月伤口愈合,骨粉几乎没有丢失,有骨小梁形态(图十九:*)。切开,刮匙去骨,有一定硬度,即刻放置修复基台,完全就位(图二十),制备临时牙冠,牙周敷料固定组织瓣(没有缝线)。
Return to Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table) Trajectory II Prevent Screw Loosening Socket Shield Graft 1st to repair buccal apical defect 开场白
Xin Wei, DDS, PhD, MS 1st edition 11/21/2019, last revision 03/18/2021