







 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
 |
||
 |
 |
 |
||
 |
 |
 |
||
 |
 |
|||
Buccal Deviation of Septal Osteotomy of Lower Molar Immediate Implant
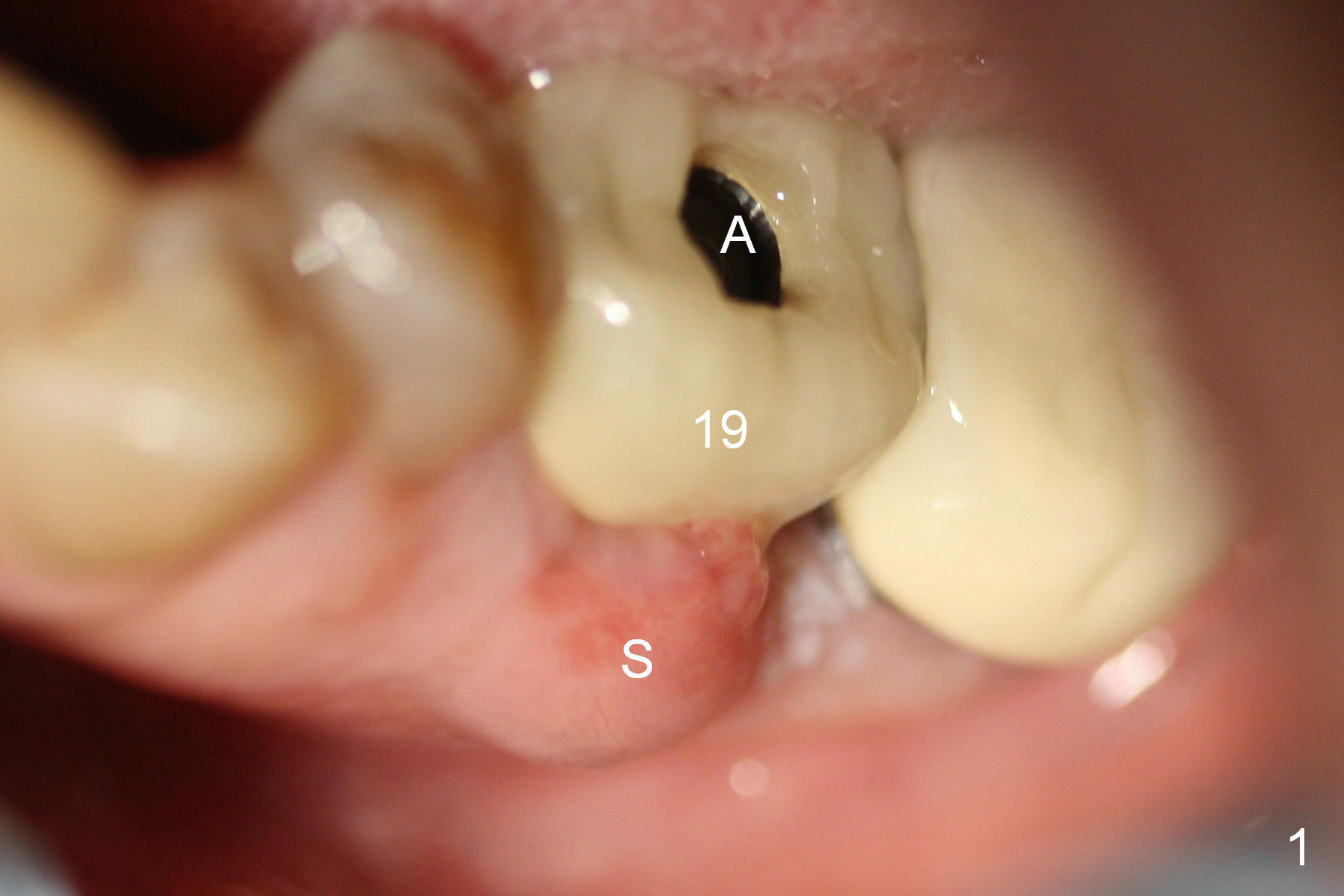
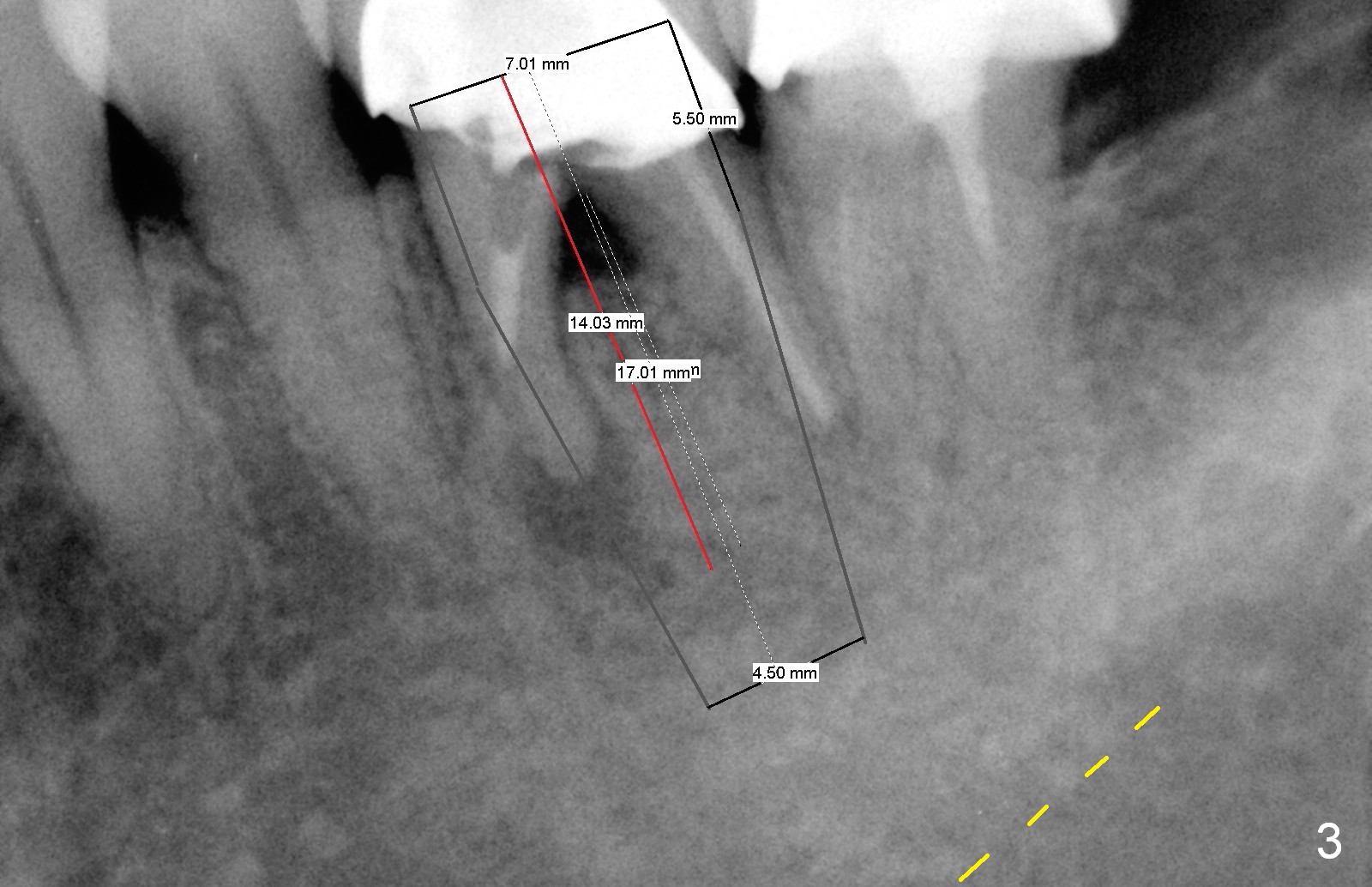
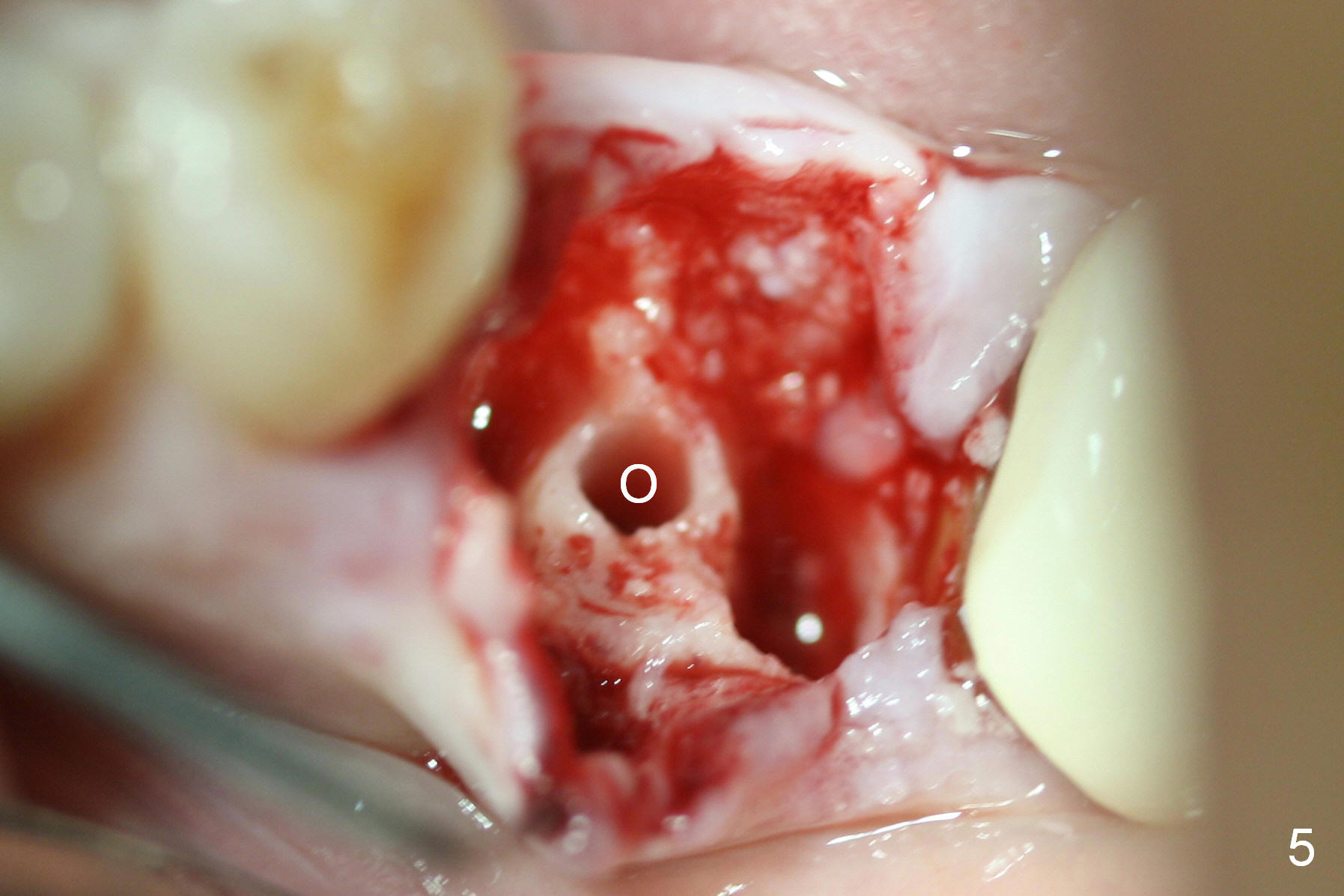
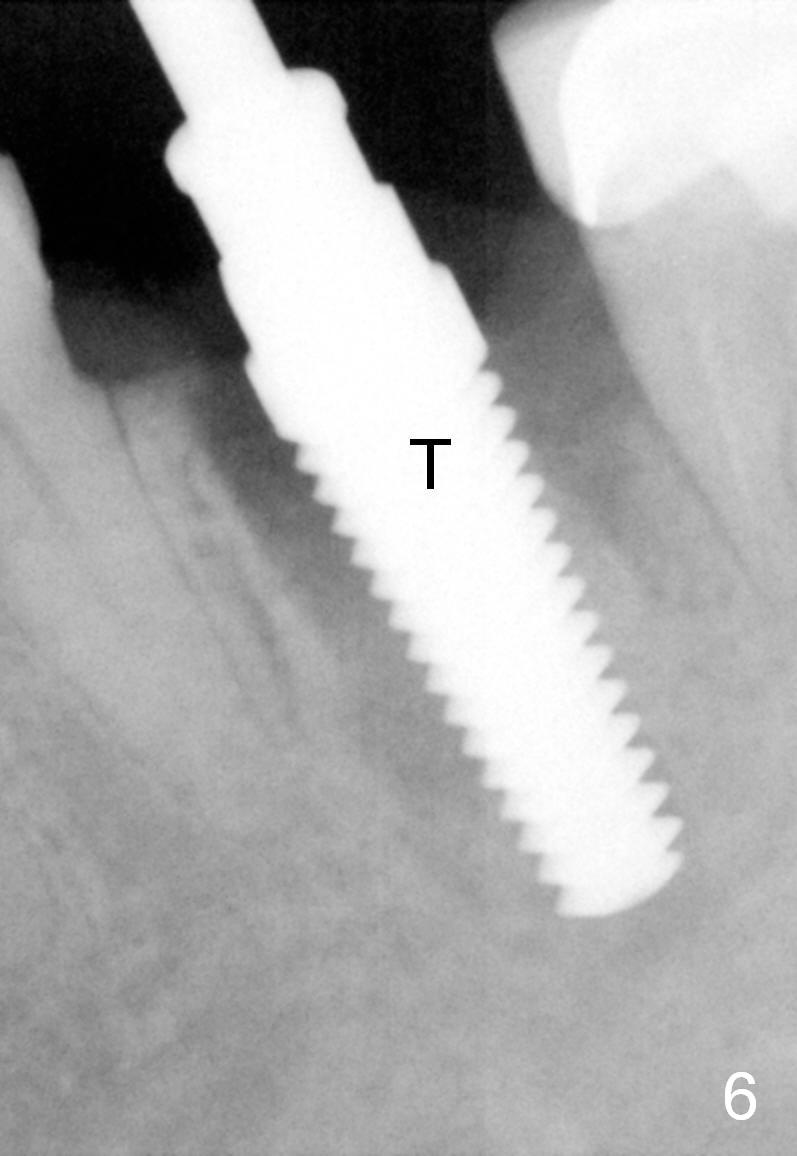
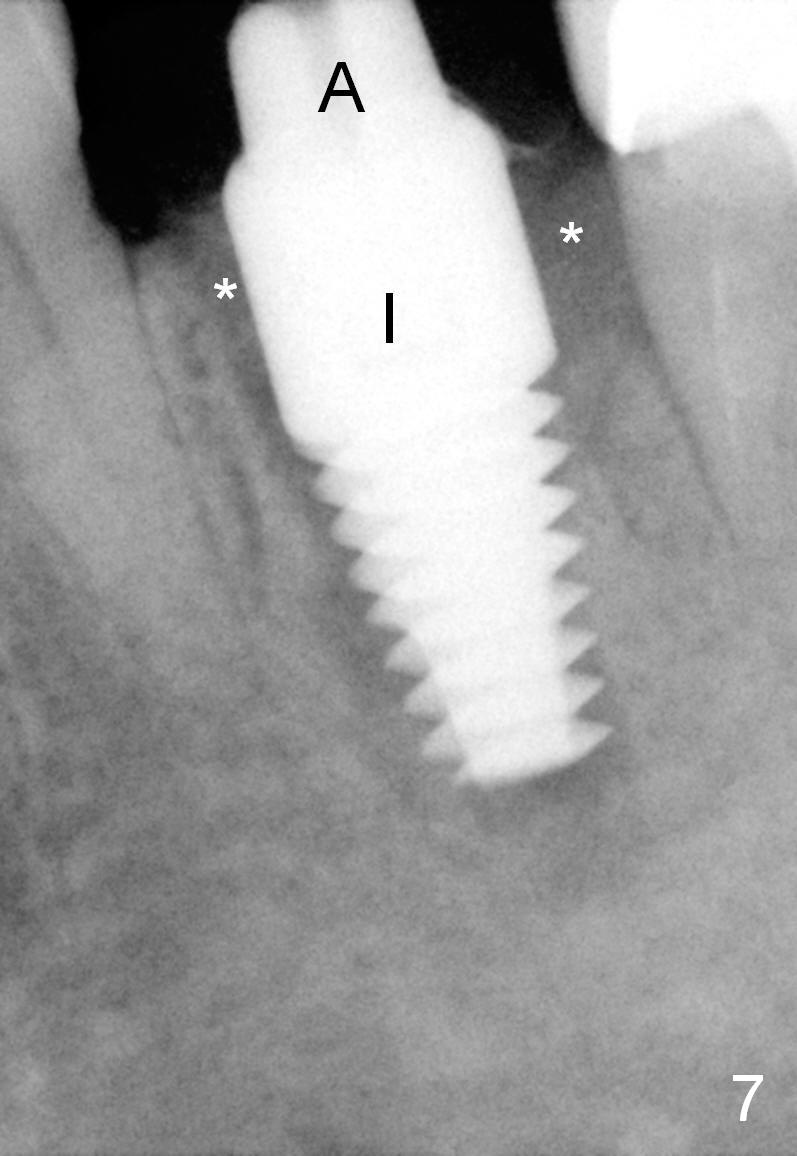
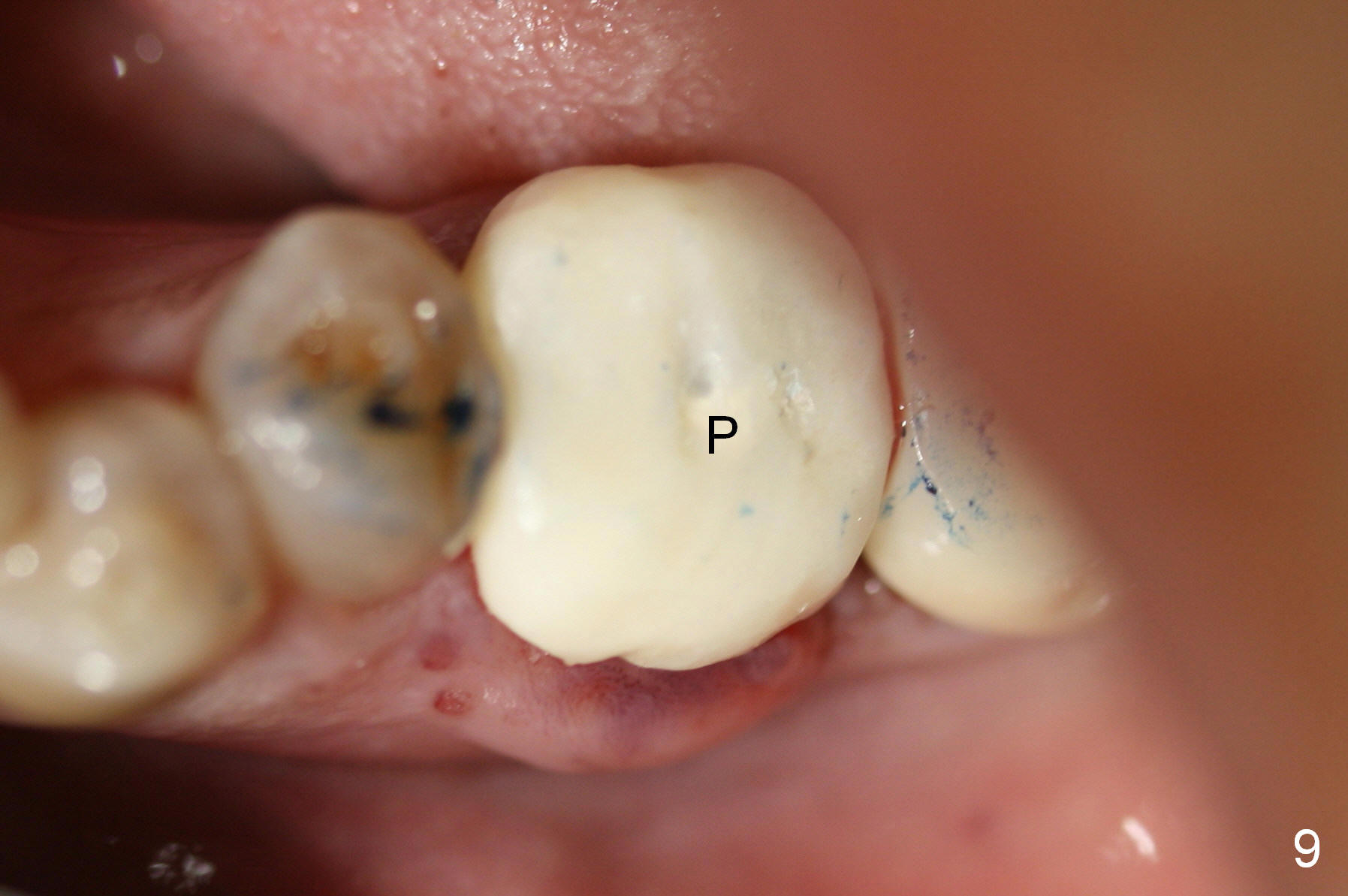
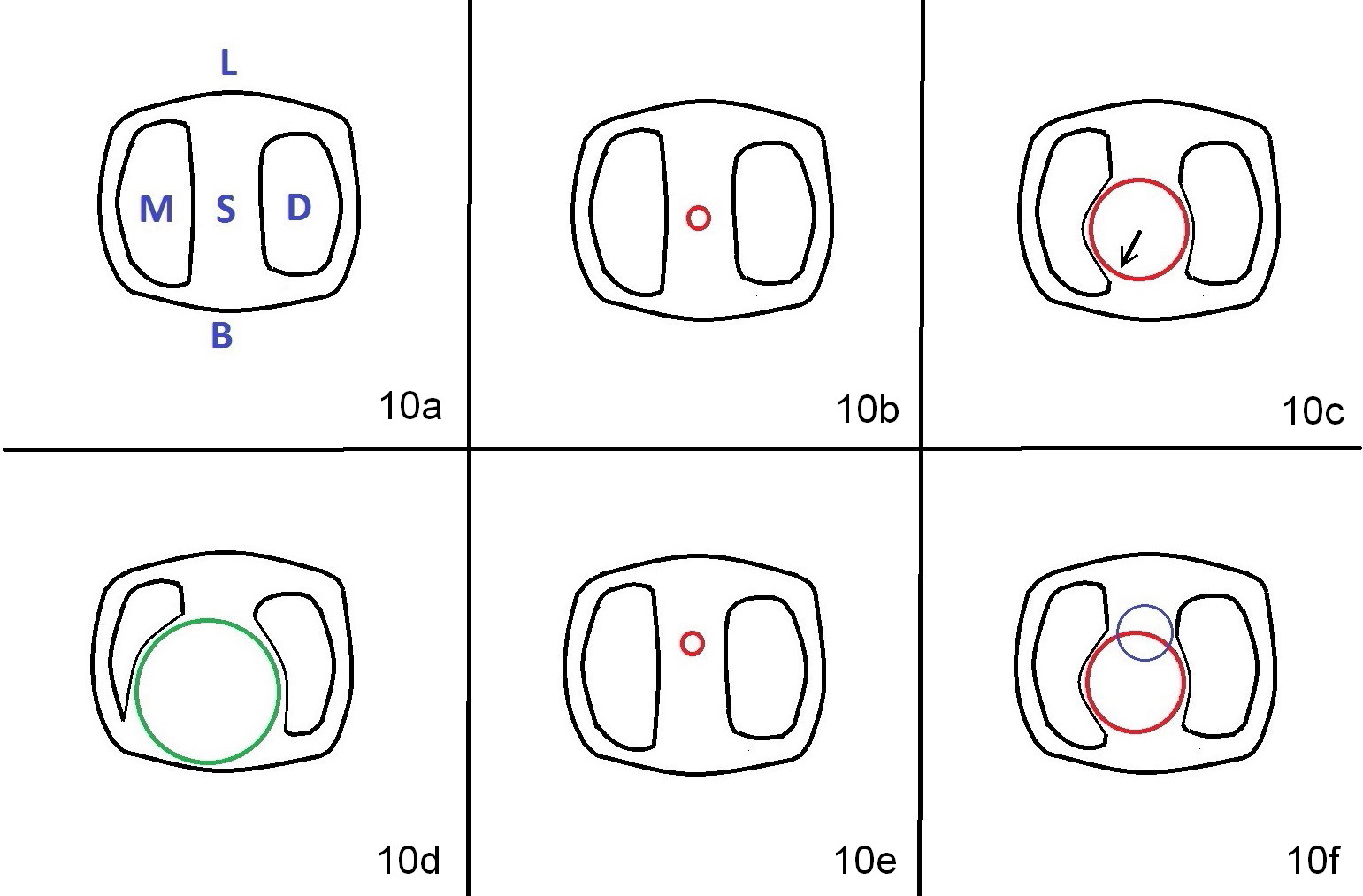
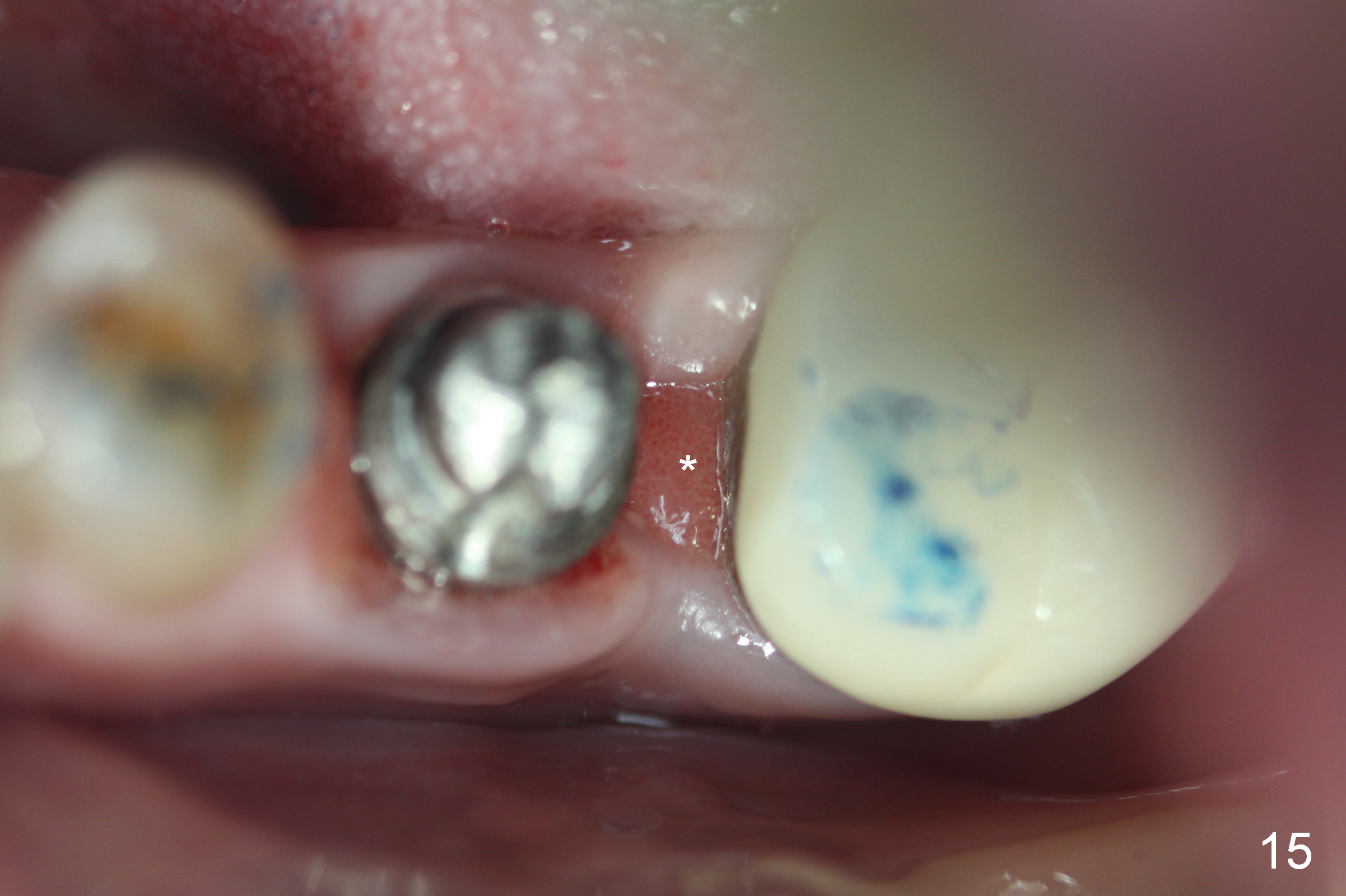
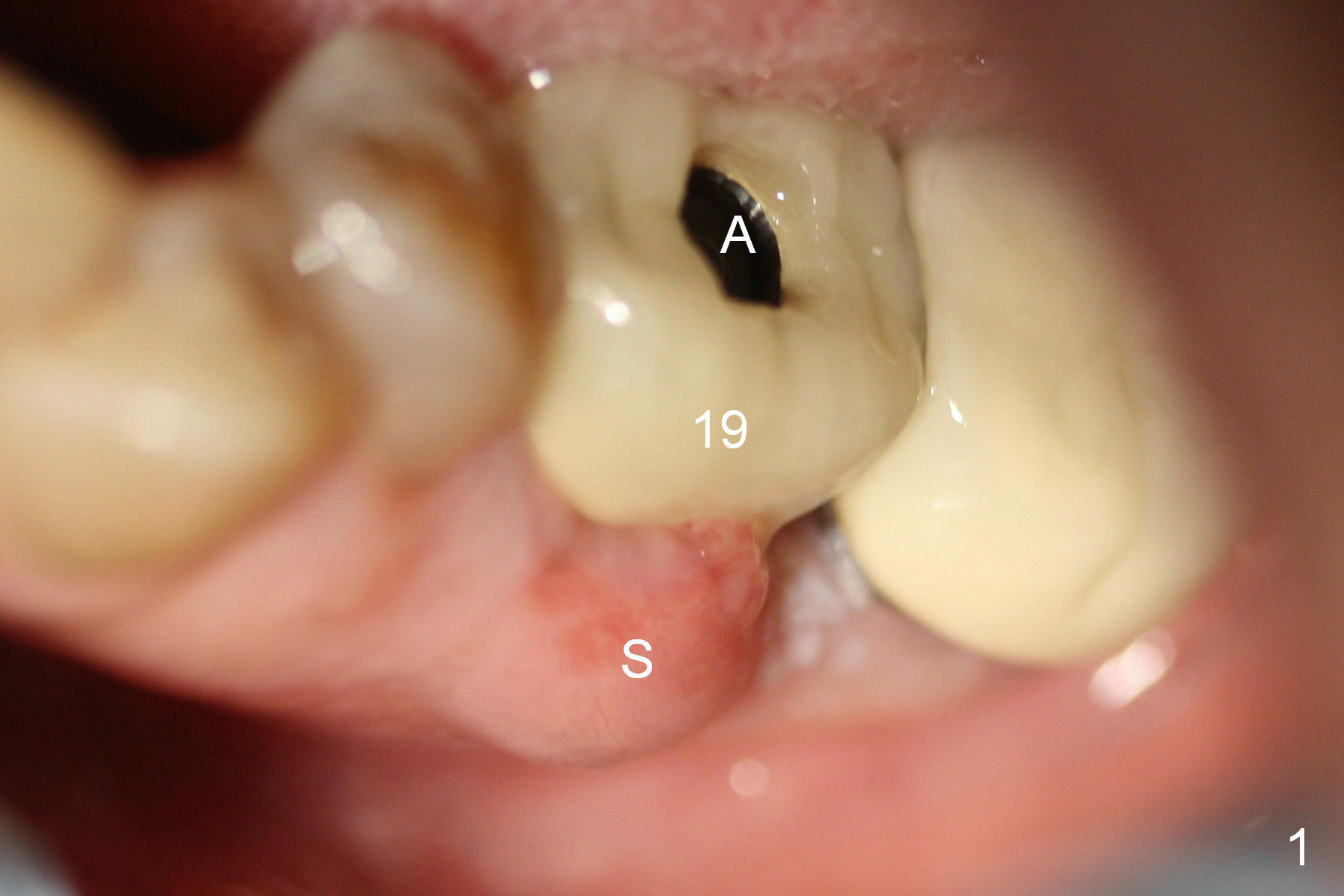
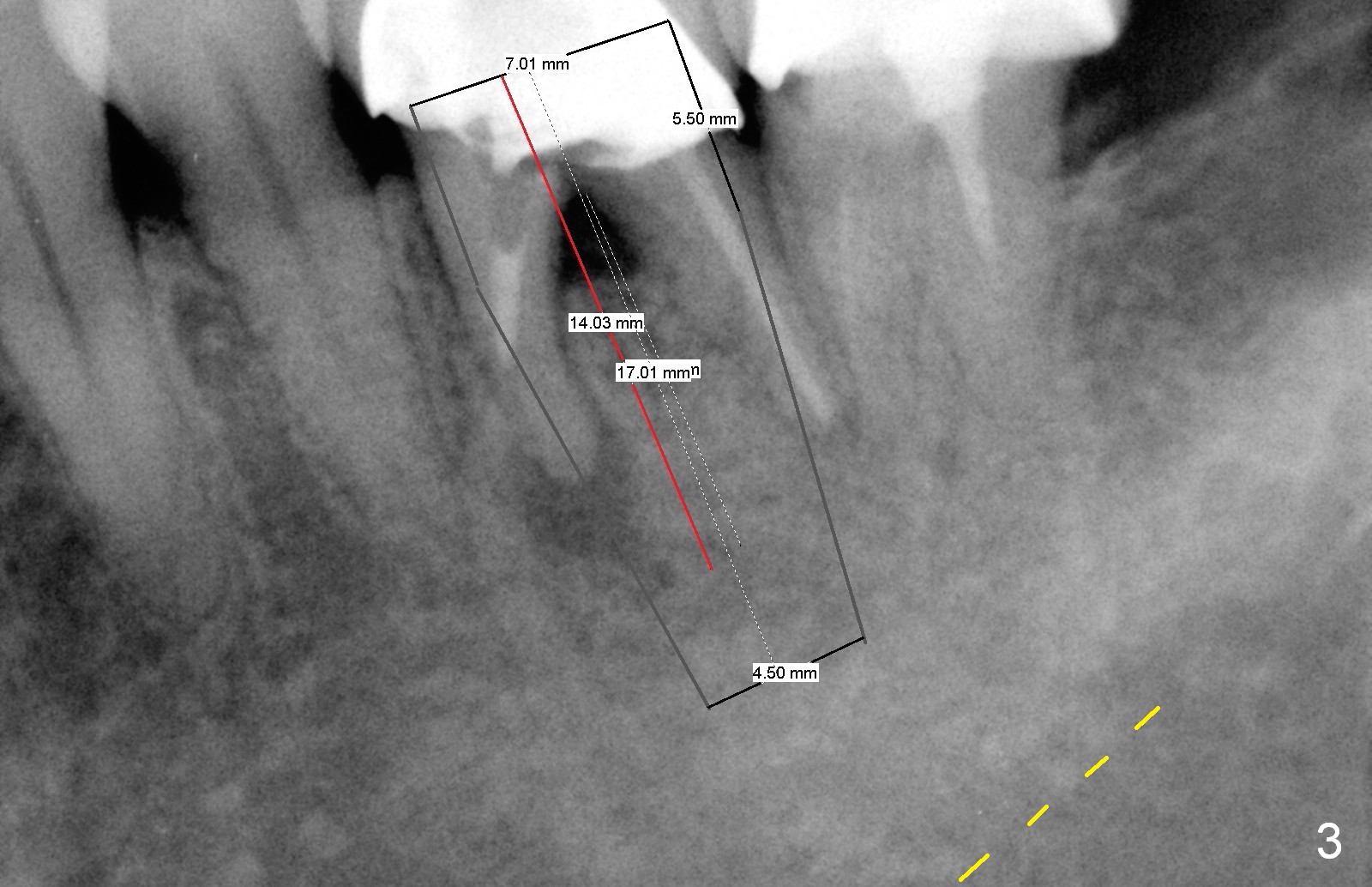
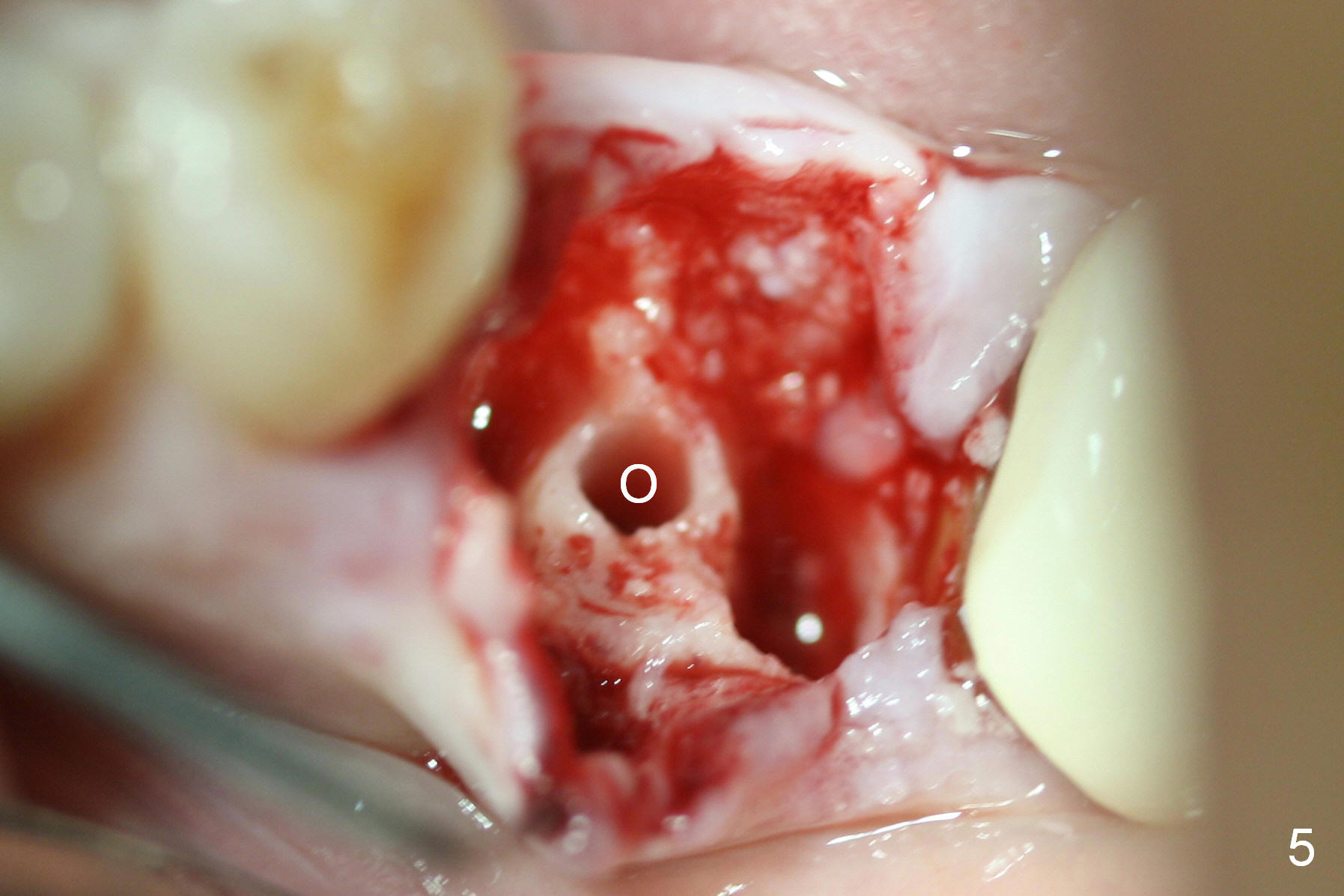
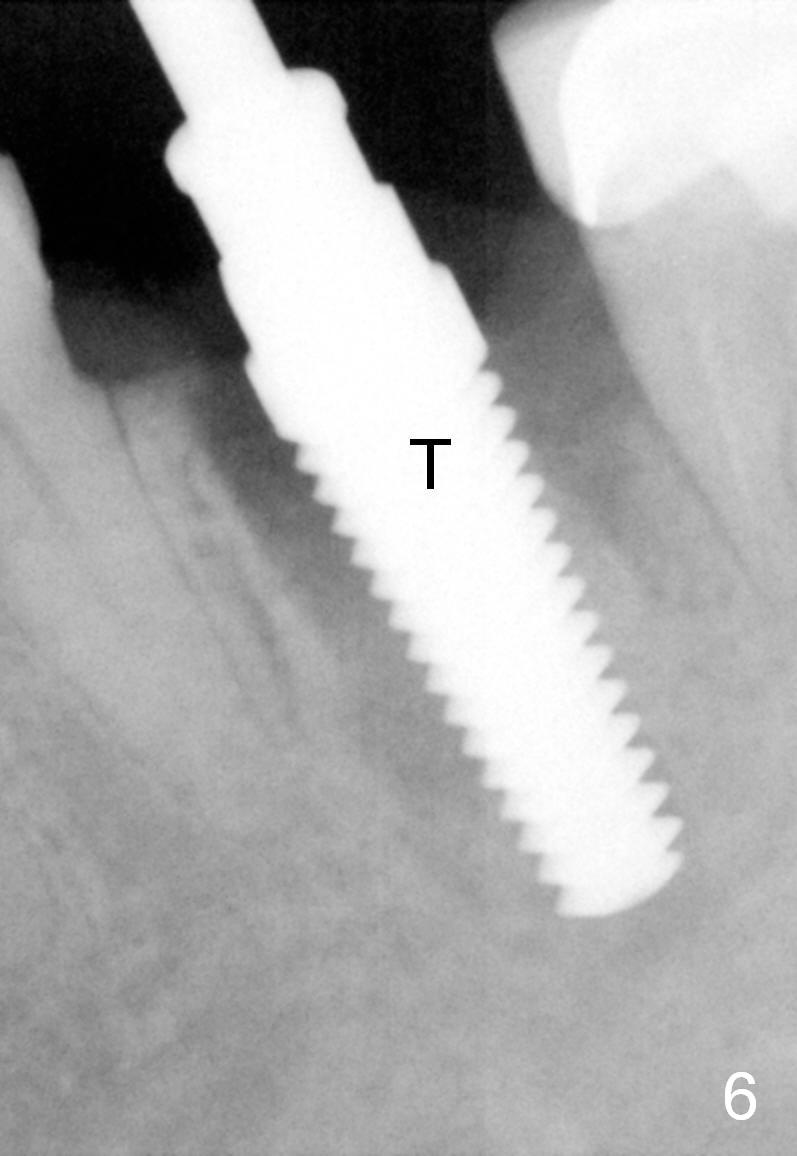
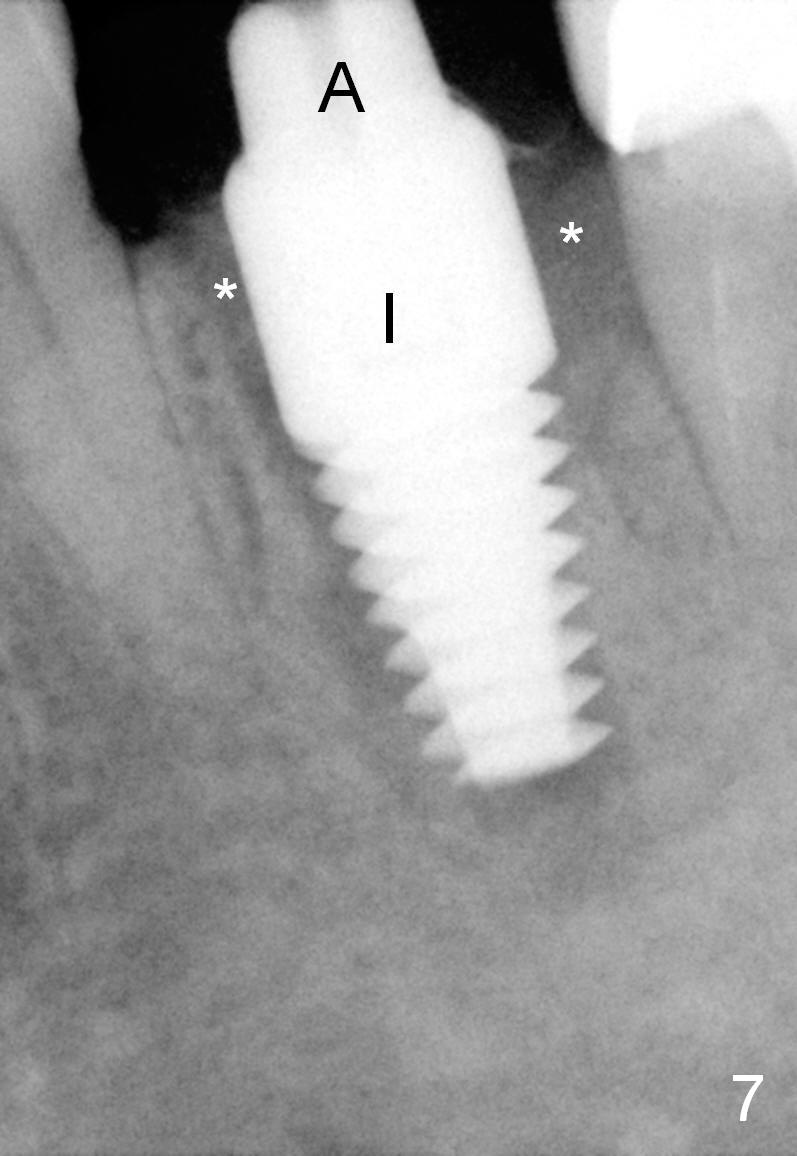
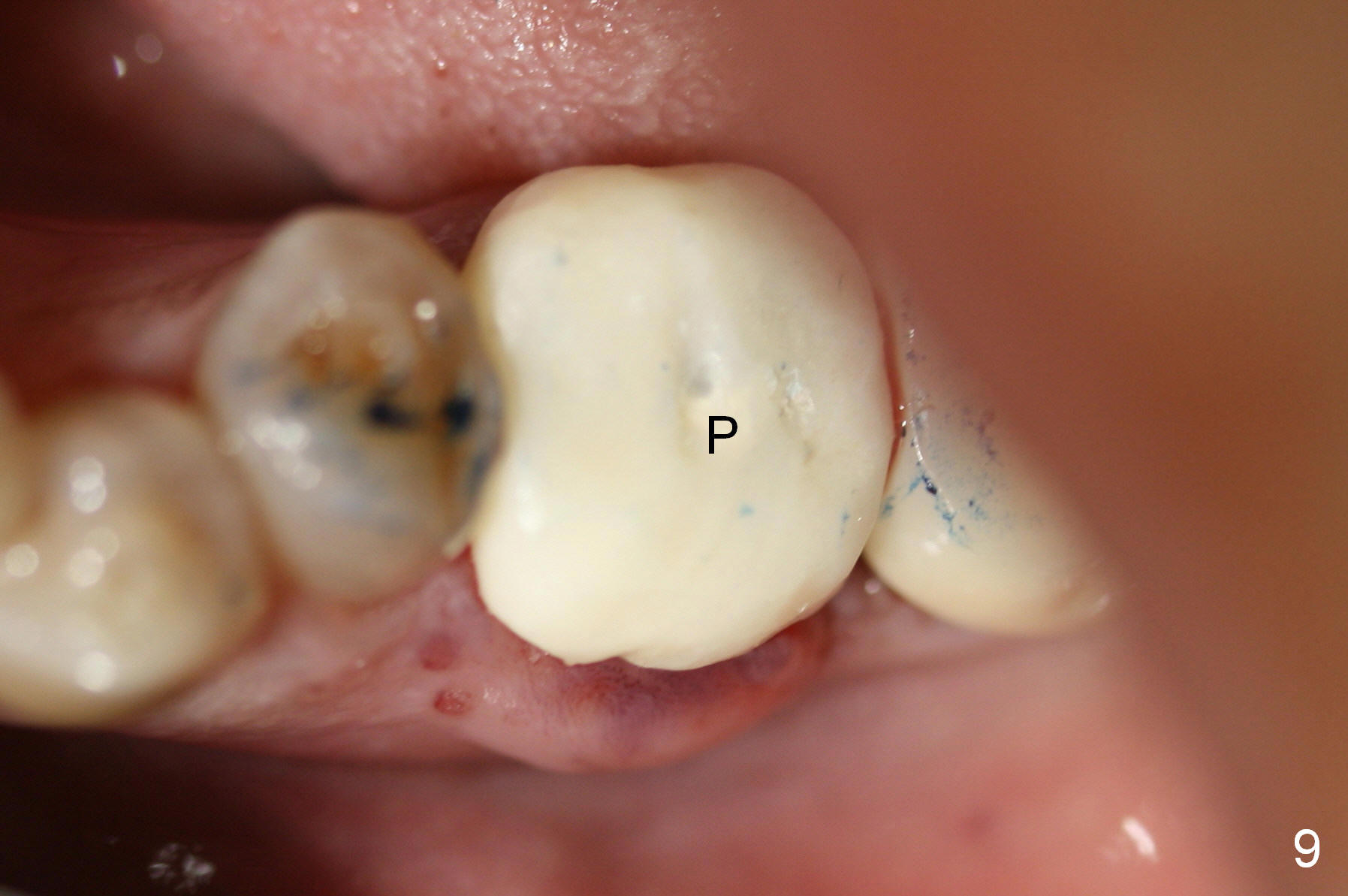
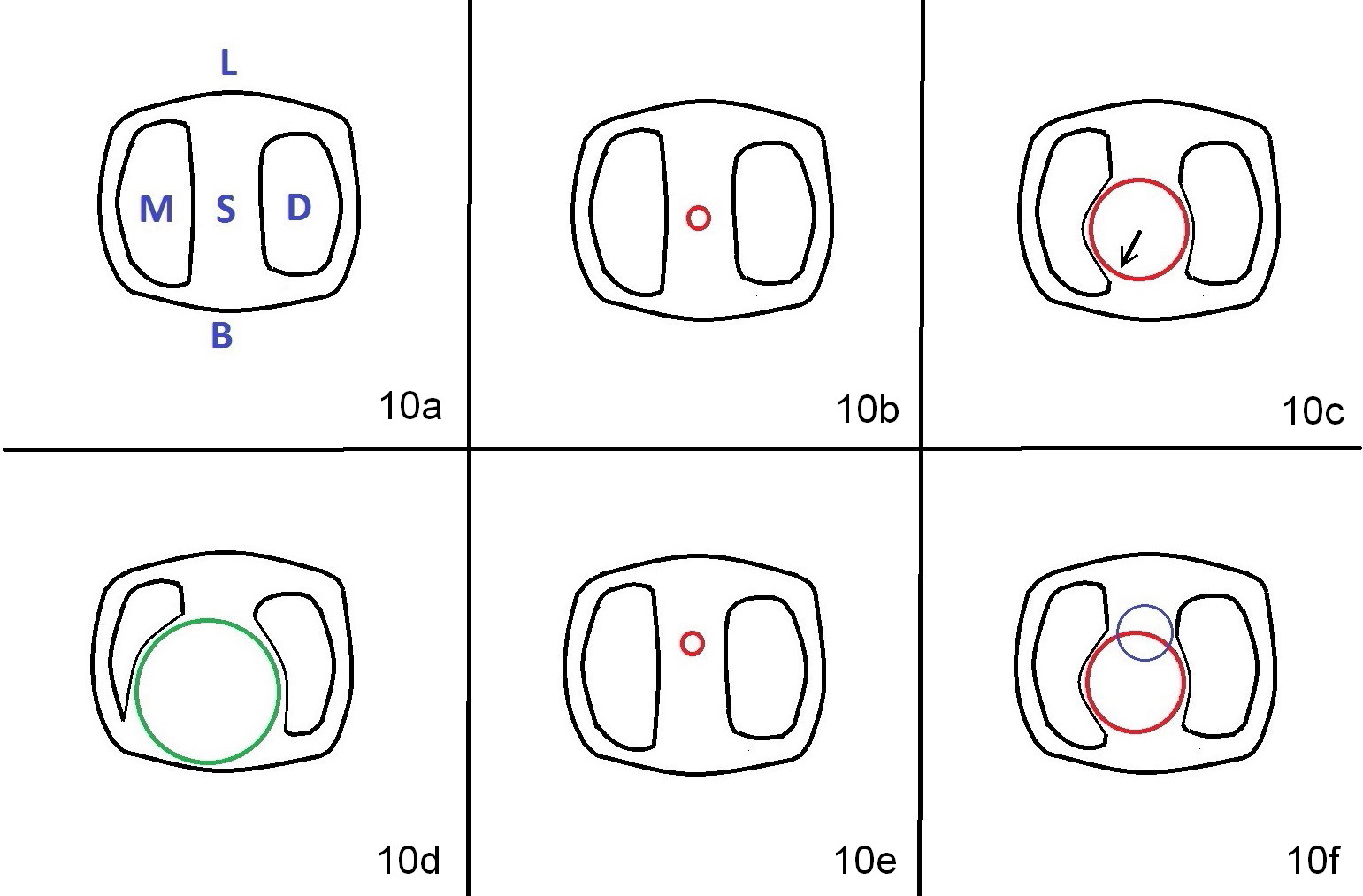
A 47-year-old lady lives out of town and presents to clinic with chief complaint "lower left back tooth easily bleeding with food impaction". Dental history and examination reveals failure of endo retreat of the tooth #19 (Fig.1), buccal gingival swelling (S), open access (A) and furcal and mesial periapical radiolucency (Fig.2 *). She is pleased to know availability of immediate implant and immediate provisional and accepts and receives the treatment at the same visit. The immediate implant (tissue-level) is designed to be as large as 7 mm and as long as 17 mm (Fig.3). To reduce paresthesia (yellow dashed line: the possible upper border of the Inferior Alveolar Canal)), a shorter implant (14 mm long in red line) is preferred. The tooth is extracted with sectioning. Granulation tissue is removed from the furca. The buccal plate appears to be intact. The septum is flat (Fig.4,10a S). Osteotomy starts in the middle of the septum with a 1.2 mm drill (Fig.10b red circle). As osteotomy increases in diameter (Fig.5 O), the apical end appears to be deviated mesiobuccally (Fig.10c large red circle). When a 6x17 mm tapered tap is being placed 14 mm deep (Fig.6 T), vibration of the buccal plate is seemingly felt at the apex (Fig.10d green circle). Further osteotomy may perforate the buccal plate. A 6x14 mm tissue-level implant is placed with >60 Ncm of insertion torque (Fig.7,8 I), followed by a 5x3 mm abutment (A) and bone graft (* in the remaining socket gap). An immediate provisional is cemented without occlusal contact (Fig.9 P).
Buccal gingival swelling and mesial periapical radiolucency suggests weakened buccal plate. Osteotomy in the septum should be initiated more lingually (Fig.10e). When the osteotomy starts being deviated, correct as early as possible with a Lindamann bur and preferably over-correct (Fig.10f blue circle). The final implant placement may not encroach the buccal plate (Fig.10f red circle). Three weeks postop, the buccal infection dissolves (Fig.11). What has not disappeared is the buccal undercut (*): the basis for potential buccal perforation. Buccolingual osteotomy trajectory should be adjusted intraoperatively accordingly.
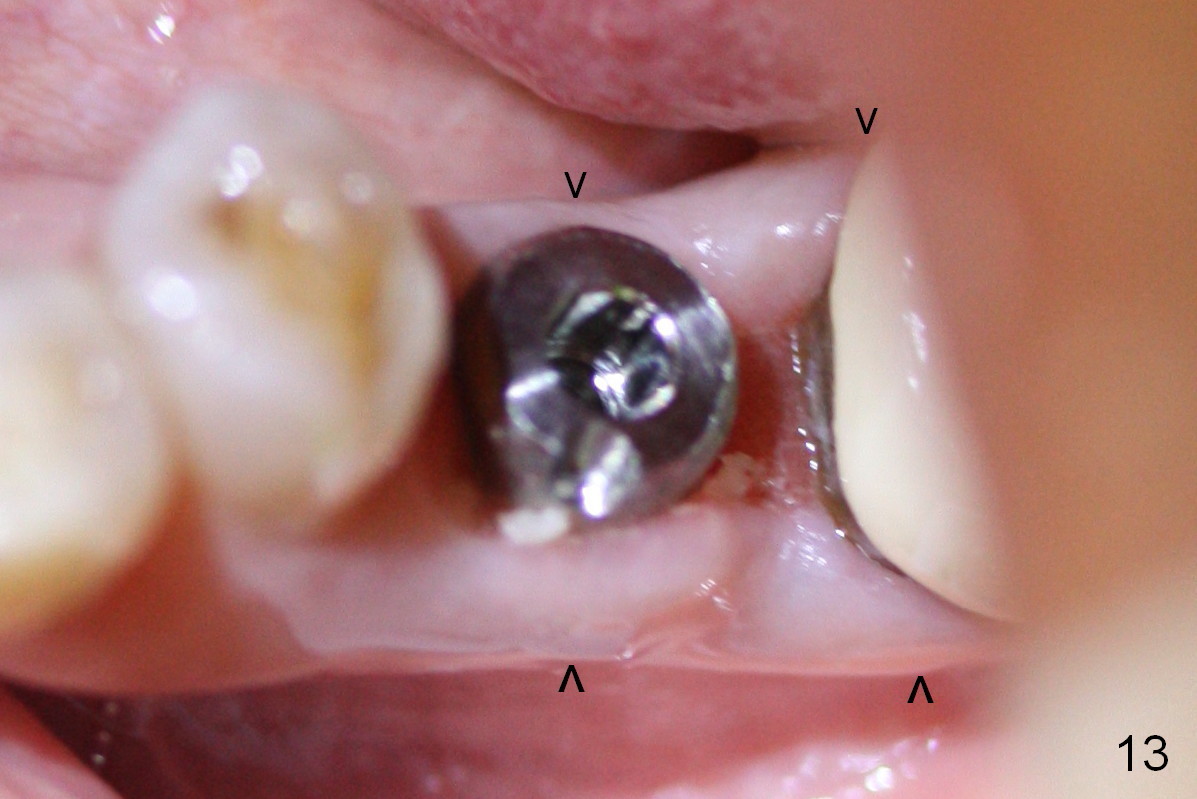
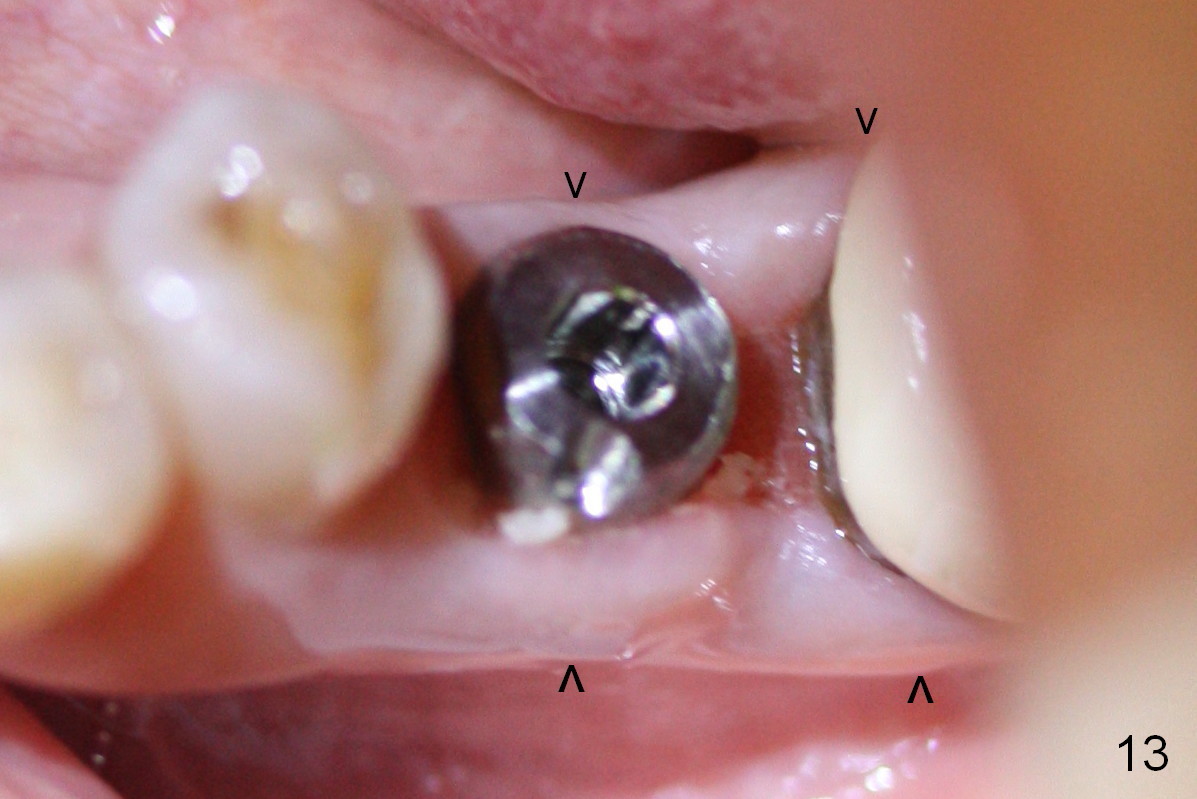
The patient returns for provisional recementation 1.5 months postop. The gingiva remains infection free (Fig.12), but the socket at the implant site has shrunk as compared to the 2nd molar site (Fig.13 arrowheads). Therefore, an implant should be placed before the socket shrinks post extraction, especially with preop lesion. Socket preservation does not prevent socket collapse. The implant is the best framework (tenting) for bone regrowth.
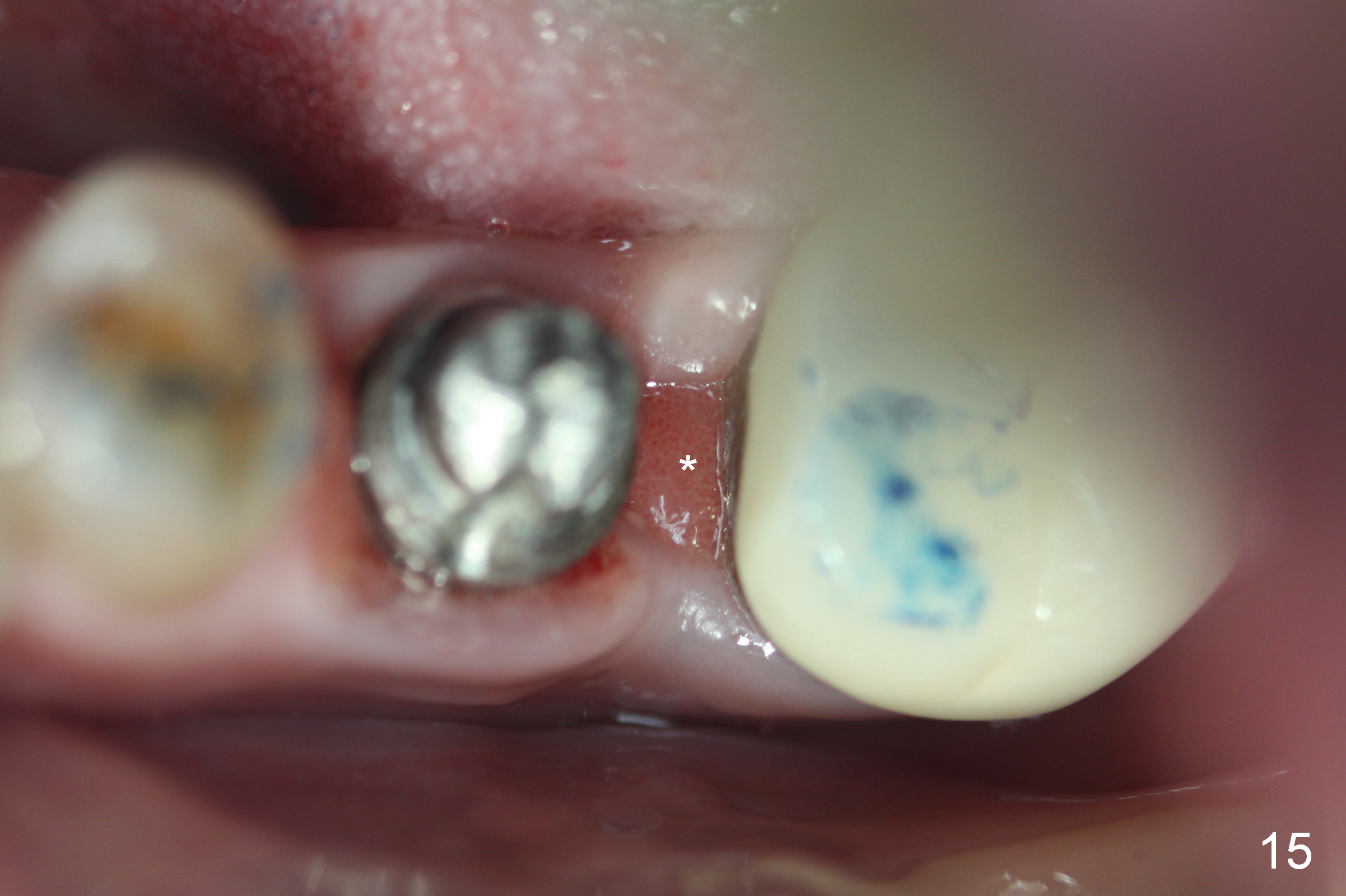
PA taken 3 months postop shows that the distal bone graft (Fig.14 *) appears to consolidate/sink down (arrow) to cover the implant threads. The distal gingiva remains to be fresh granulation tissue less than 4 months postop, immediately before crown cementation (Fig.15 *). The significance of the latter remains to be known. In fact, there is no problem in the distal embrasure. Two and a half months after cementation, the patient returns requesting remaking the crown, since food is easily impacted mesially with floss trauma, as shown by arrowhead in Fig.16.
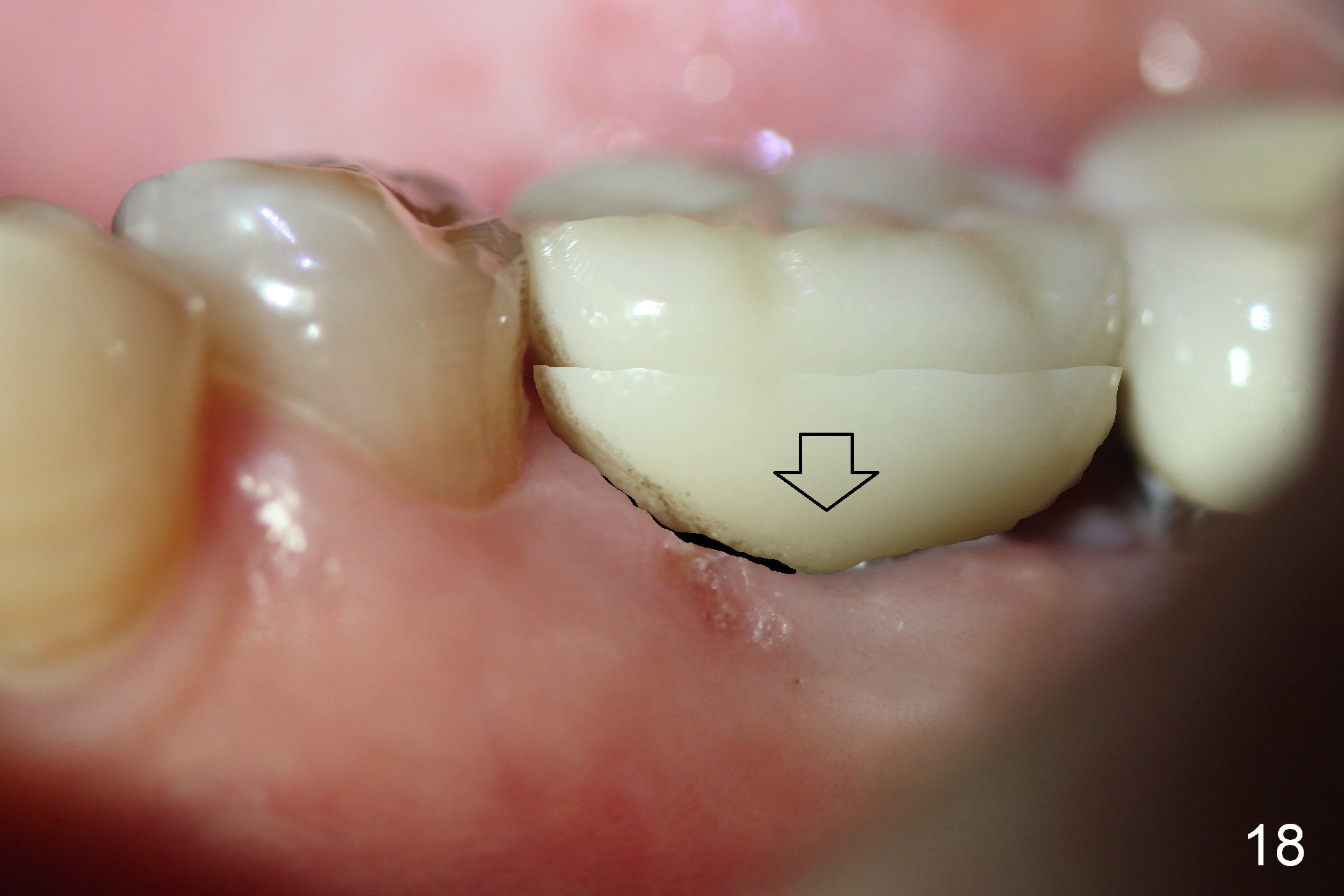
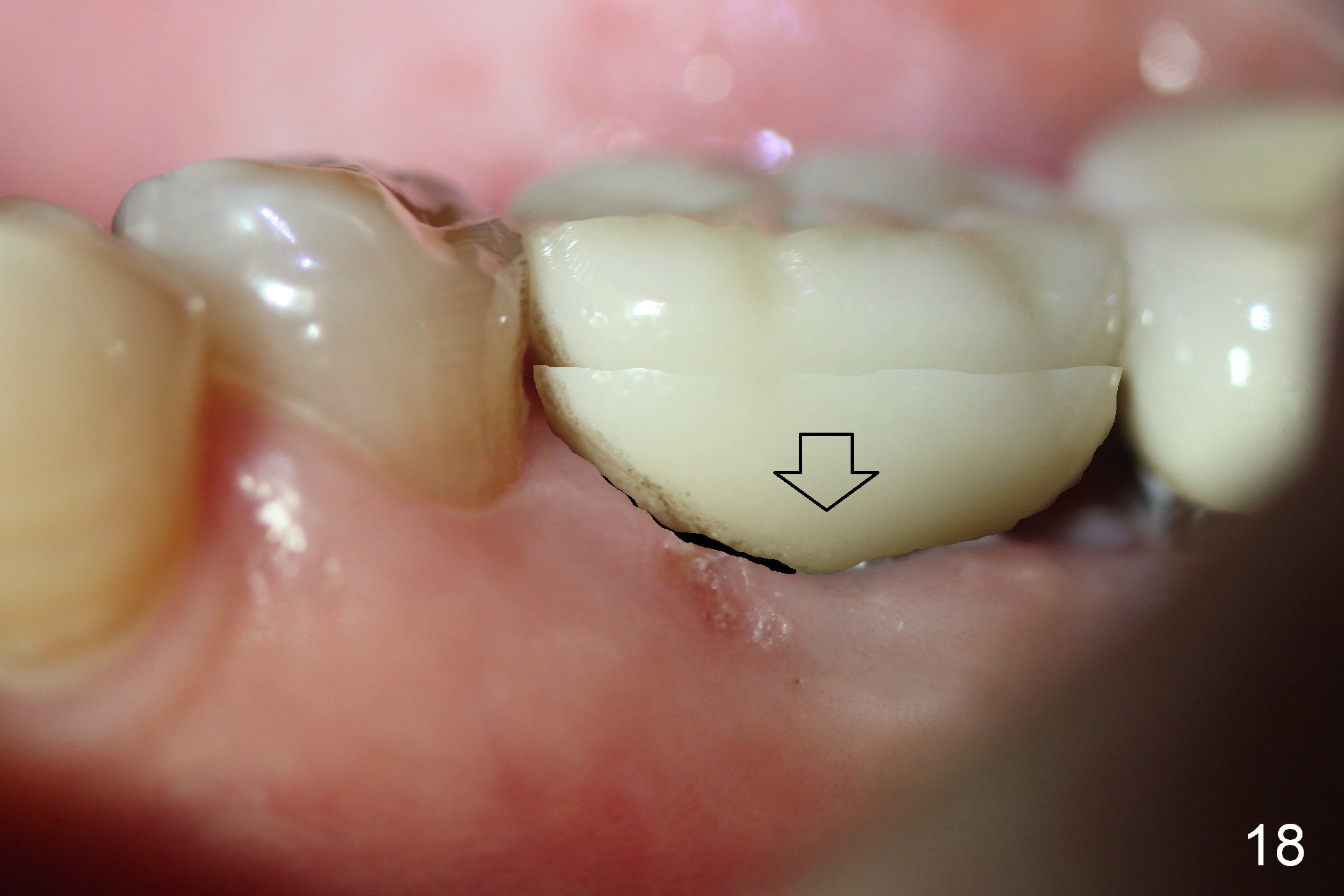
After removing the crown, the margin is lowered clinically. In the lab, the mesial gingiva in the model is to be trimmed ~1 mm (Fig.17 arrow (black area)) so that the mesial embrasure is closed as much as possible (Fig.18). The contact area is larger both buccolingually and apicocoronally. Clinically, the mesial margin of the temporary crown should be a little bit bulging to push the mesial papilla mesially so that there is enough space to clean cement for the permanent crown.
Return to Lower Molar Immediate Implant,
Posterior Immediate Provisional,
Technicians
Xin Wei, DDS, PhD, MS 1st edition 02/15/2015, last revision 01/19/2018