

 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Warning Signs of Paresthesia
A 51-year-old lady has all of typical features easy for paresthesia to happen: 1. small mouth; 2. dental phobia; 3. periodontitis.
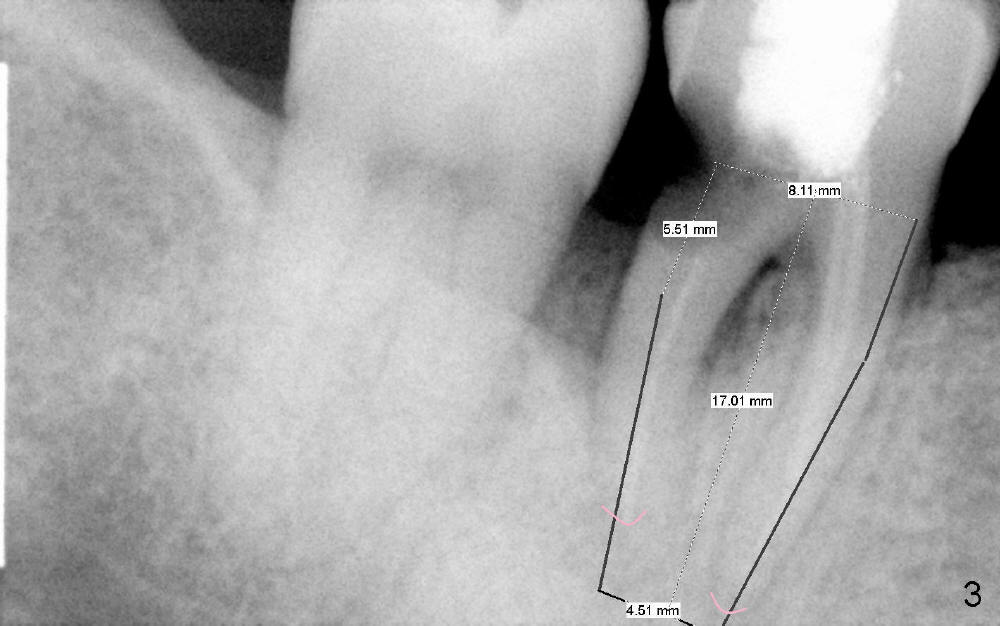
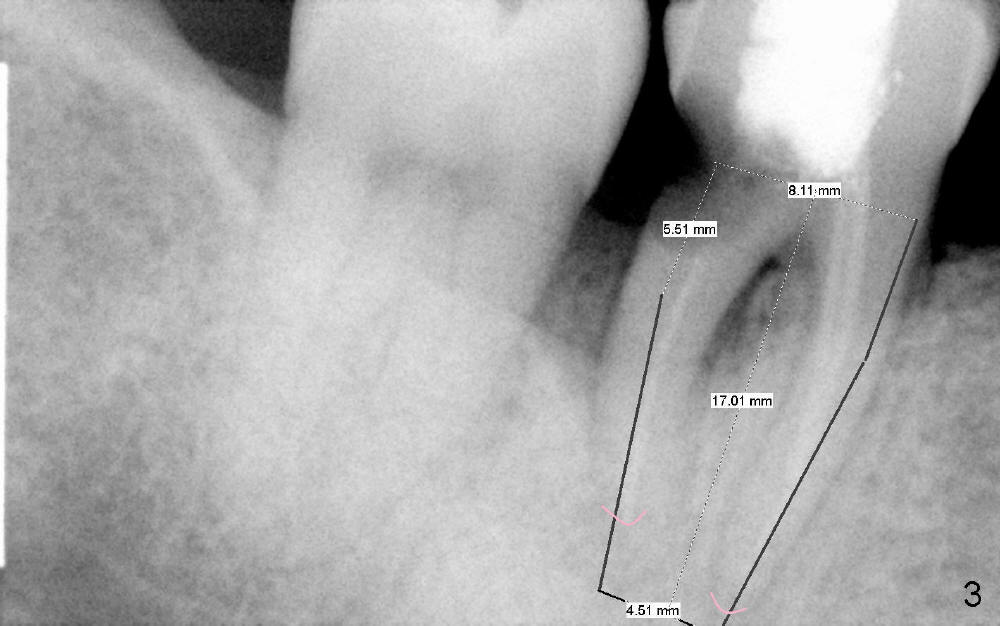
Small mouth does not allow us to use #2 sensor. The sensor #1 does not show the Inferior Alveolar Canal (IAC) apical to the affected tooth (#30 in Fig.1). The PA was taken 4.5 years ago. Fig.2 is taken immediately prior to extraction and immediate implant. Fig.3 is design of implant placement based on the previous X-ray. Retrospectively, a new PA or preferably CT should have been taken. Gingiva may have recessed in 4-5 years, particularly with periodontal patients. Soft tissue landmark may be not reliable.
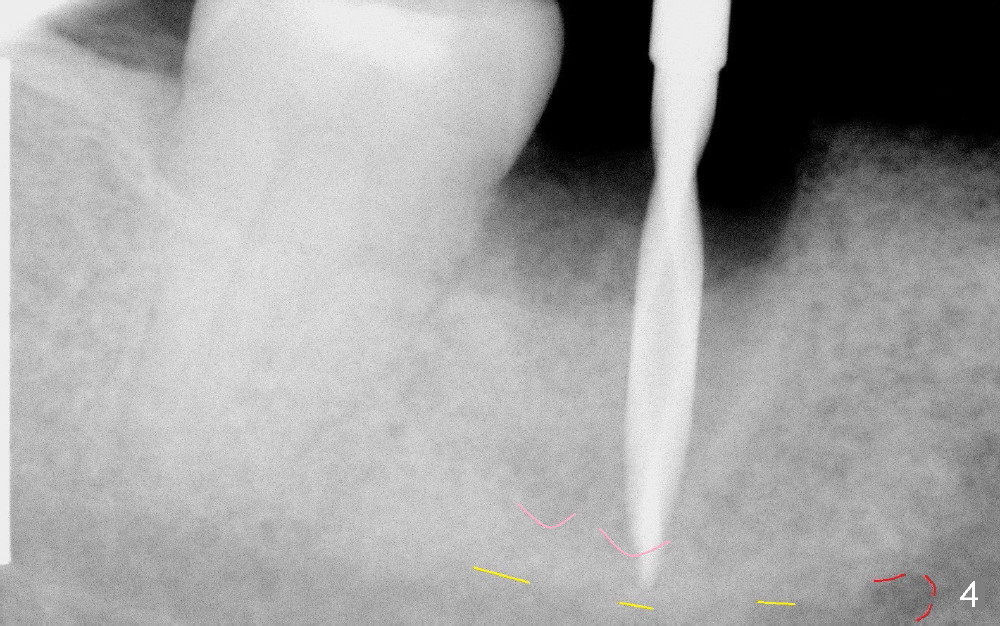
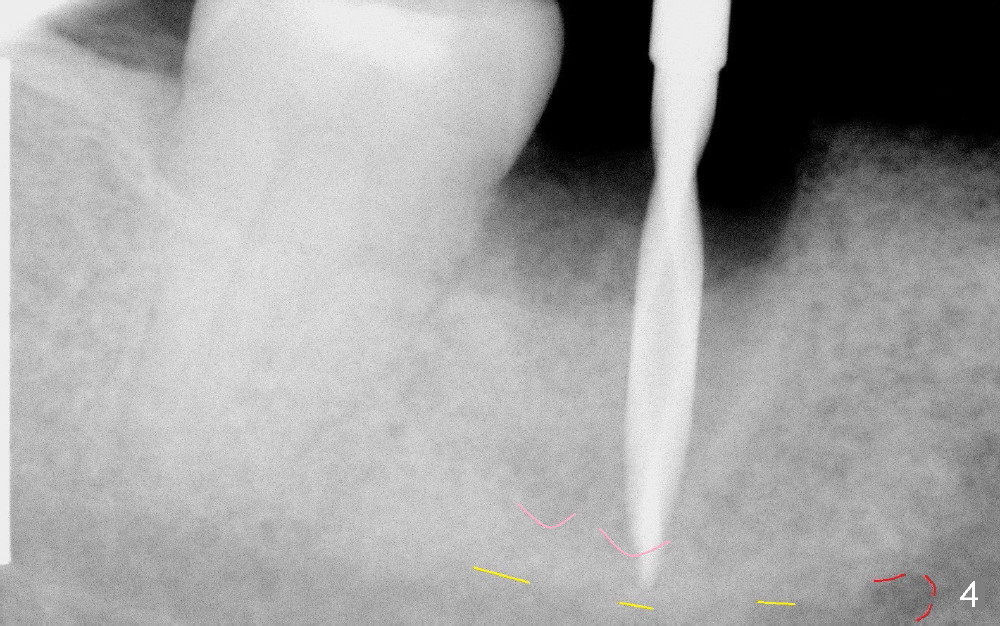
After extraction, a 2 mm pilot drill is placed 17 mm from the gingival margin, it looks close to IAC (Fig.4). At the time of surgery, it felt maybe alright if the depth is controlled tightly for further osteotomy. Taking intraop PA is not an easy task even with sensor 1. Several exposure has to be done for every step. This is a warning sign. Retrospectively, the osteotomy should be confined to the apex of the socket (pink).
Infiltration anesthesia was administered initially. When osteotomy increases in diameter, the patient experienced pain. Block anesthesia was added. Retrospectively, block anesthesia should not been done. Instead shorten osteotomy or perform socket preservation (2).
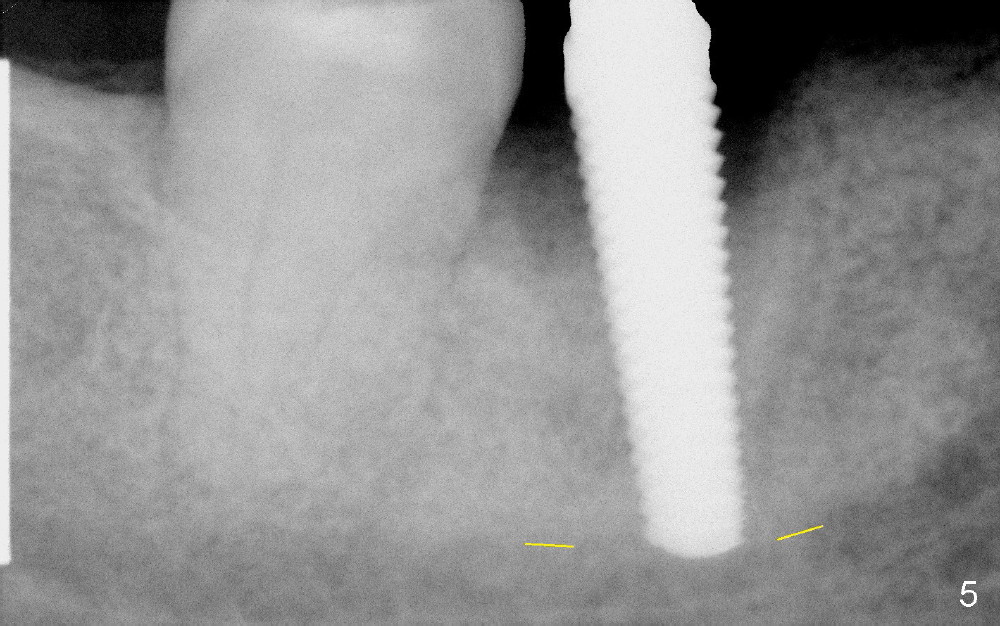
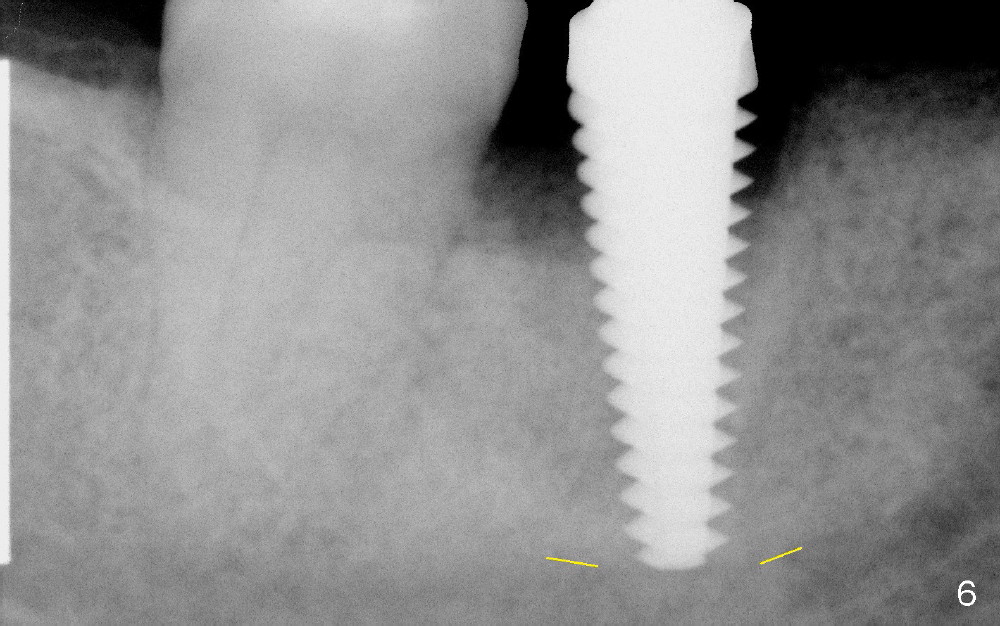
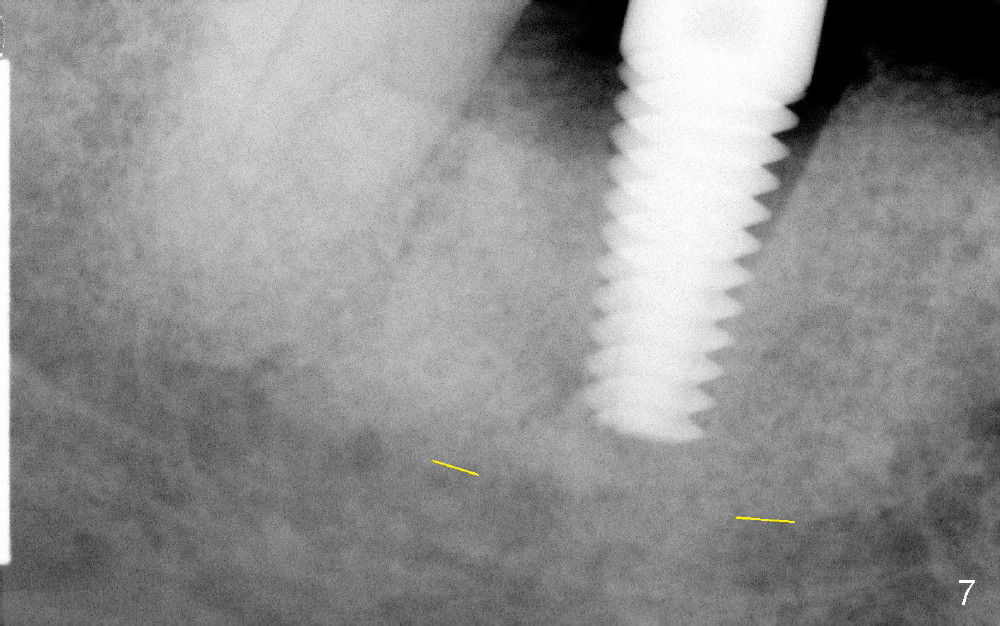
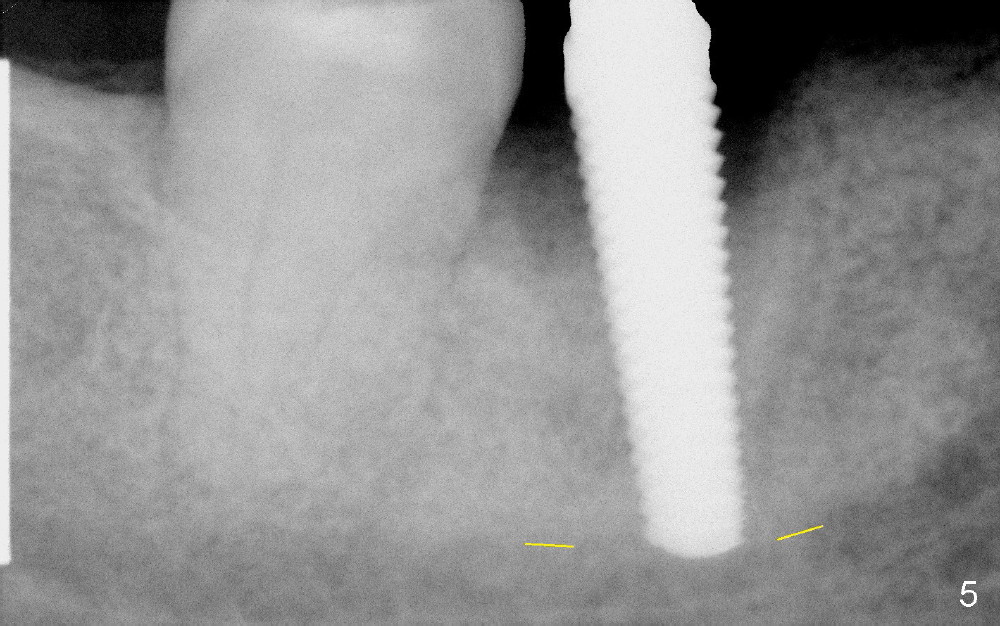
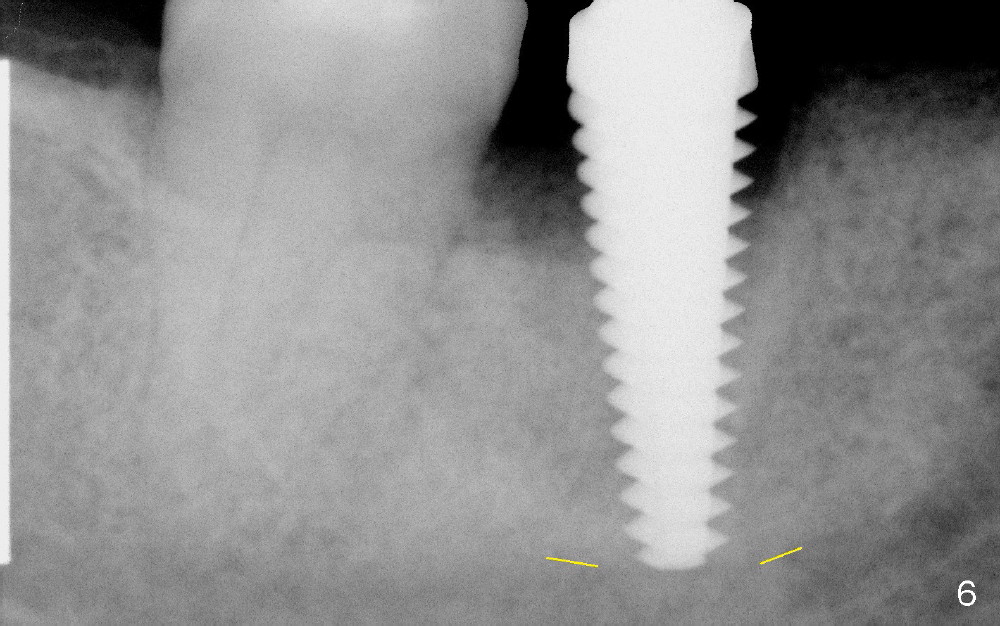
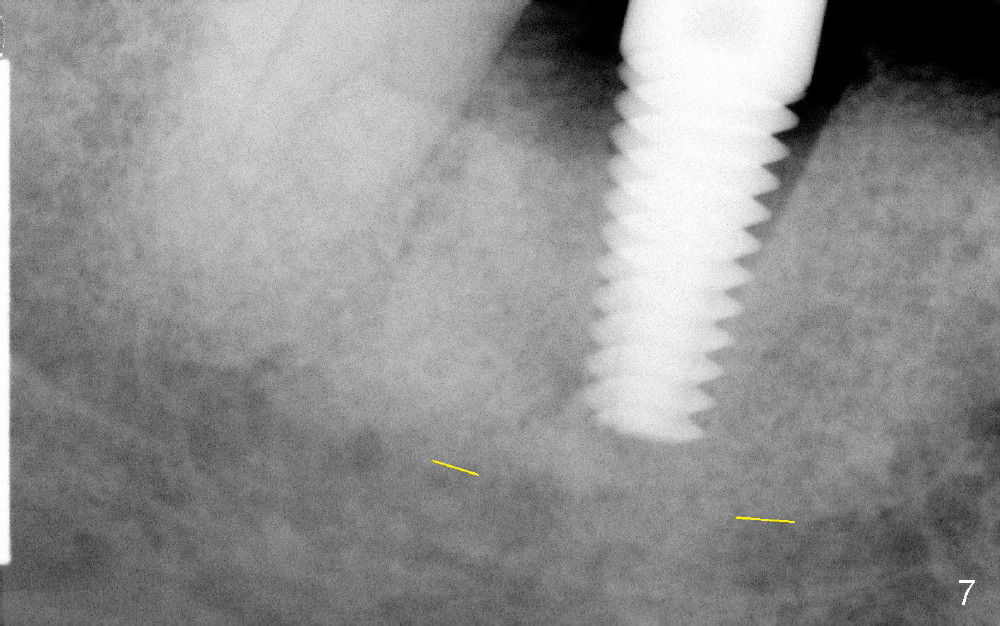
By the time of 5 and 6 mm taps are placed, they touch IAC (Fig.5,6, respectively). In fact, the finding was ignored at surgery. A 6x17 mm tissue-level implant (Fig.7) is not placed as deep as the corresponding tap (Fig.6), because of high torque and pressure felt by the patient. A short abutment is placed for immediate provisional to hold the existing partial in place.
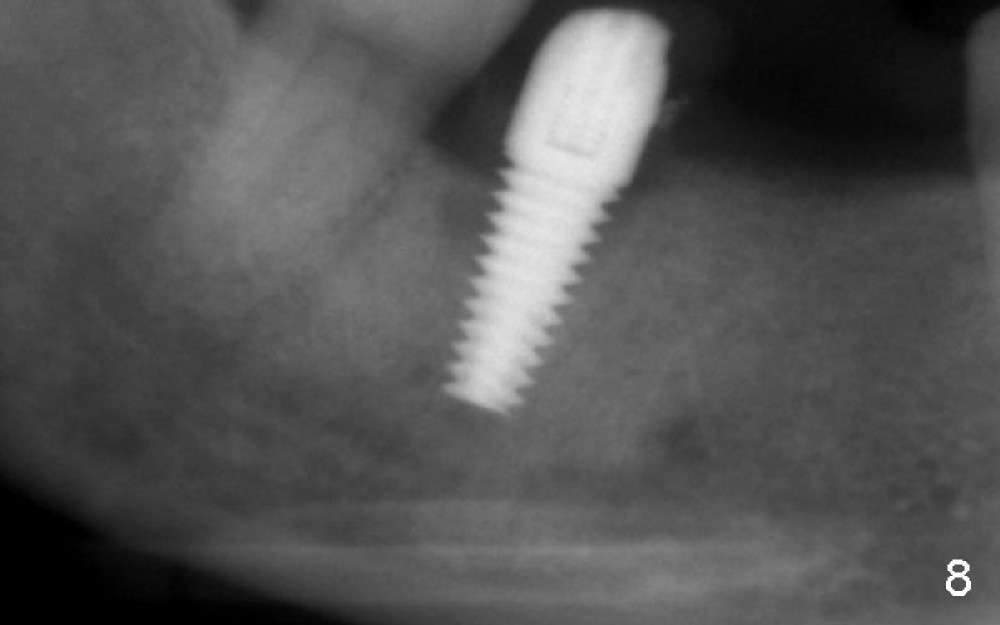
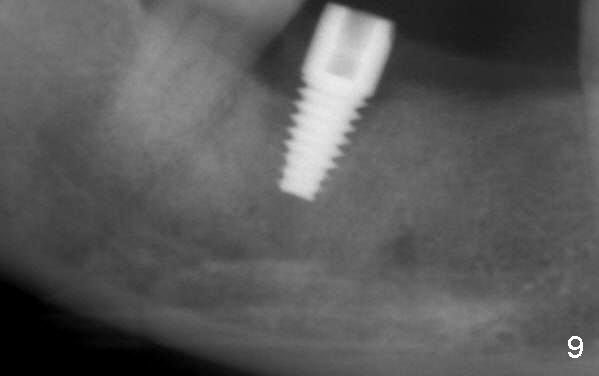
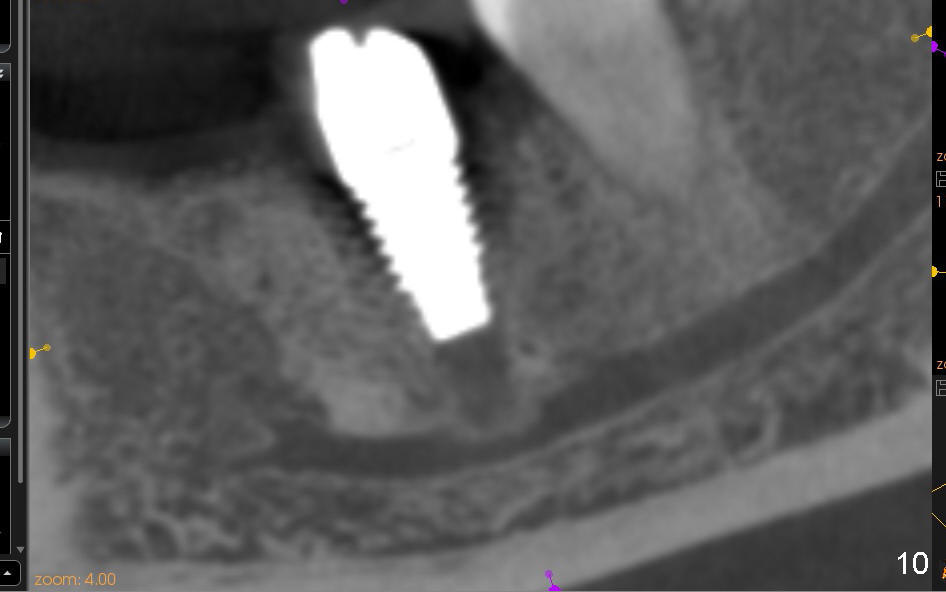
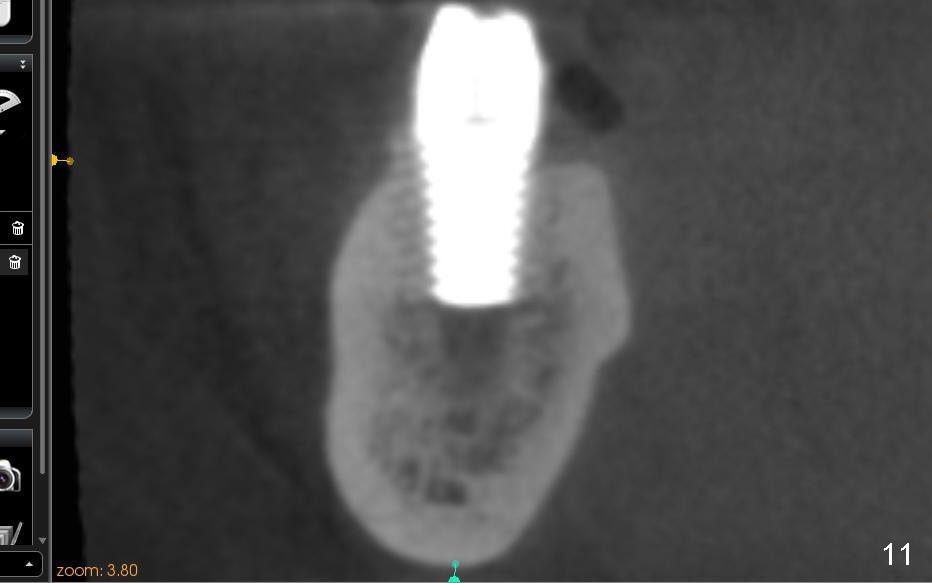
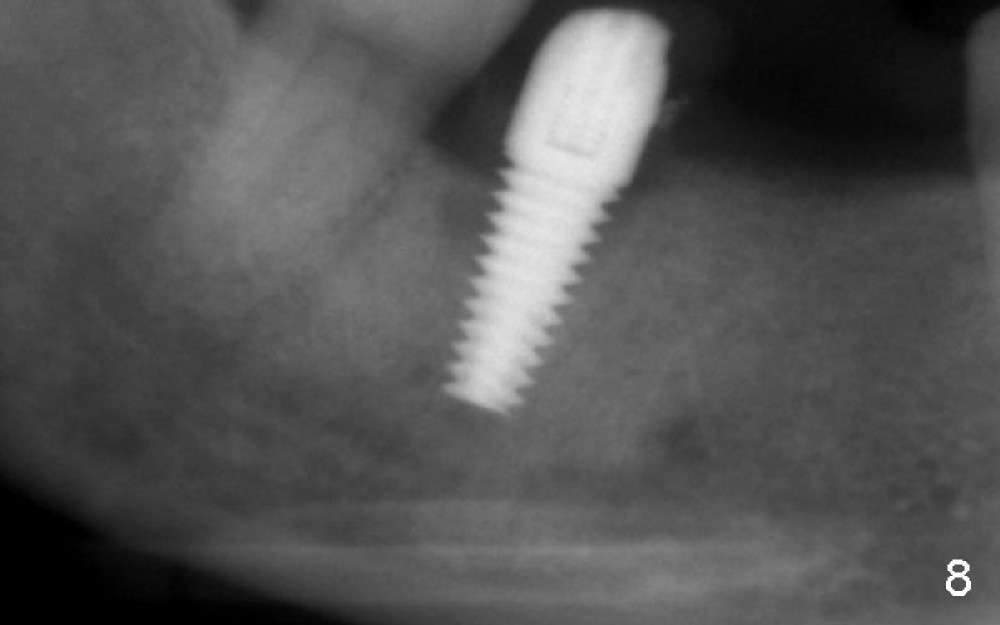
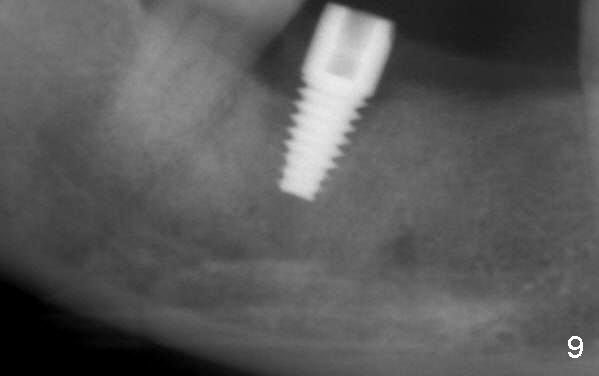
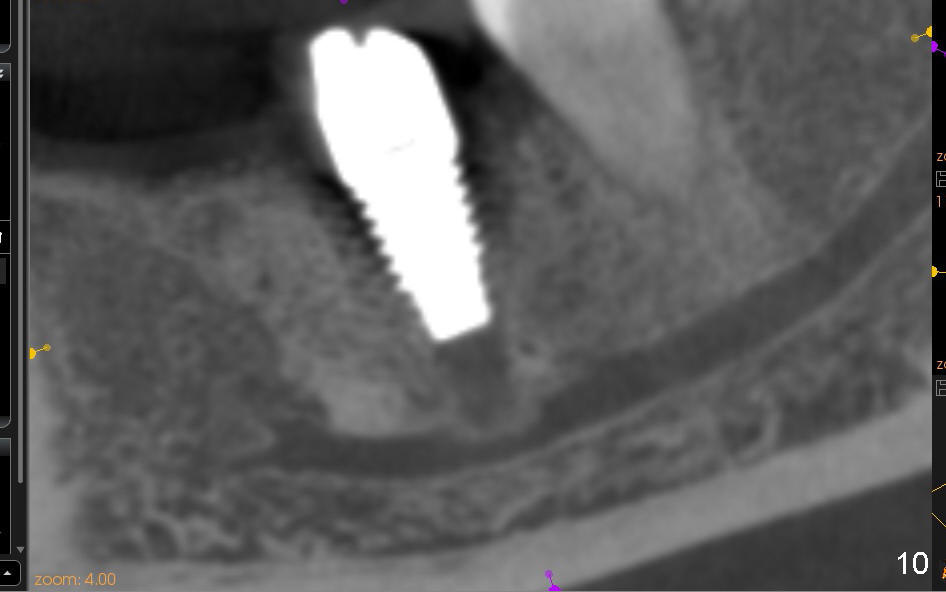
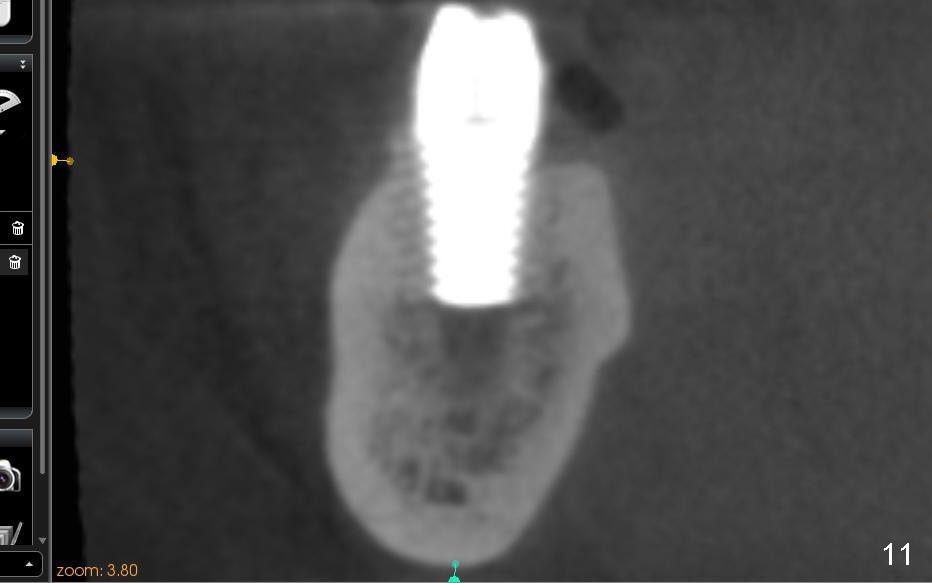
Four to 5 hours postop, the patient reports paresthesia. The following day, she returns. Panoramic X-ray is taken (Fig.8), which is consistent with Fig.7. In order to achieve the best possible outcome, the implant is removed, cut short ~ 3 mm and placed back (Fig.9). CT shows that bone has been pushed to IAC (Fig.10 (sagittal), 11 (coronal)).
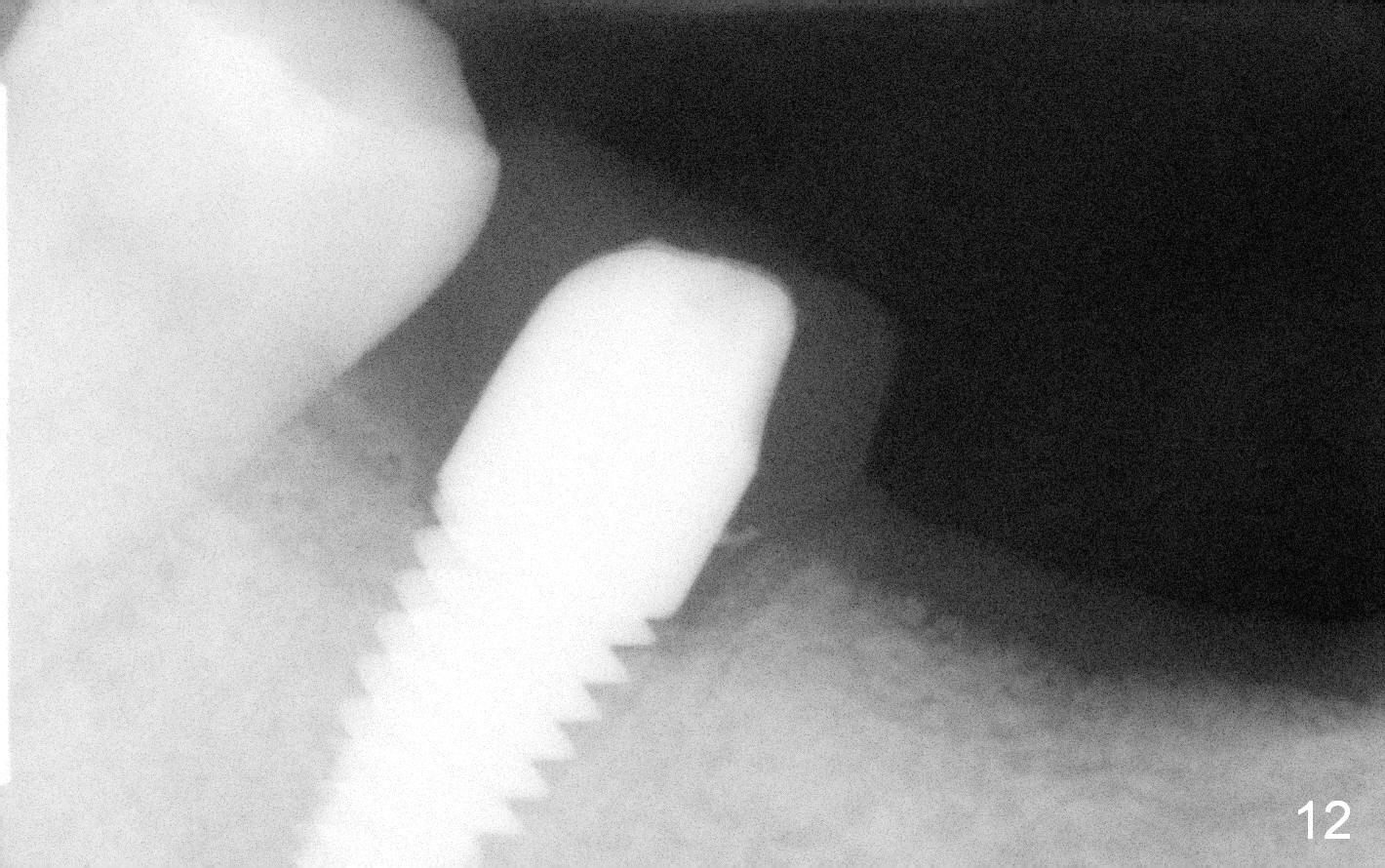
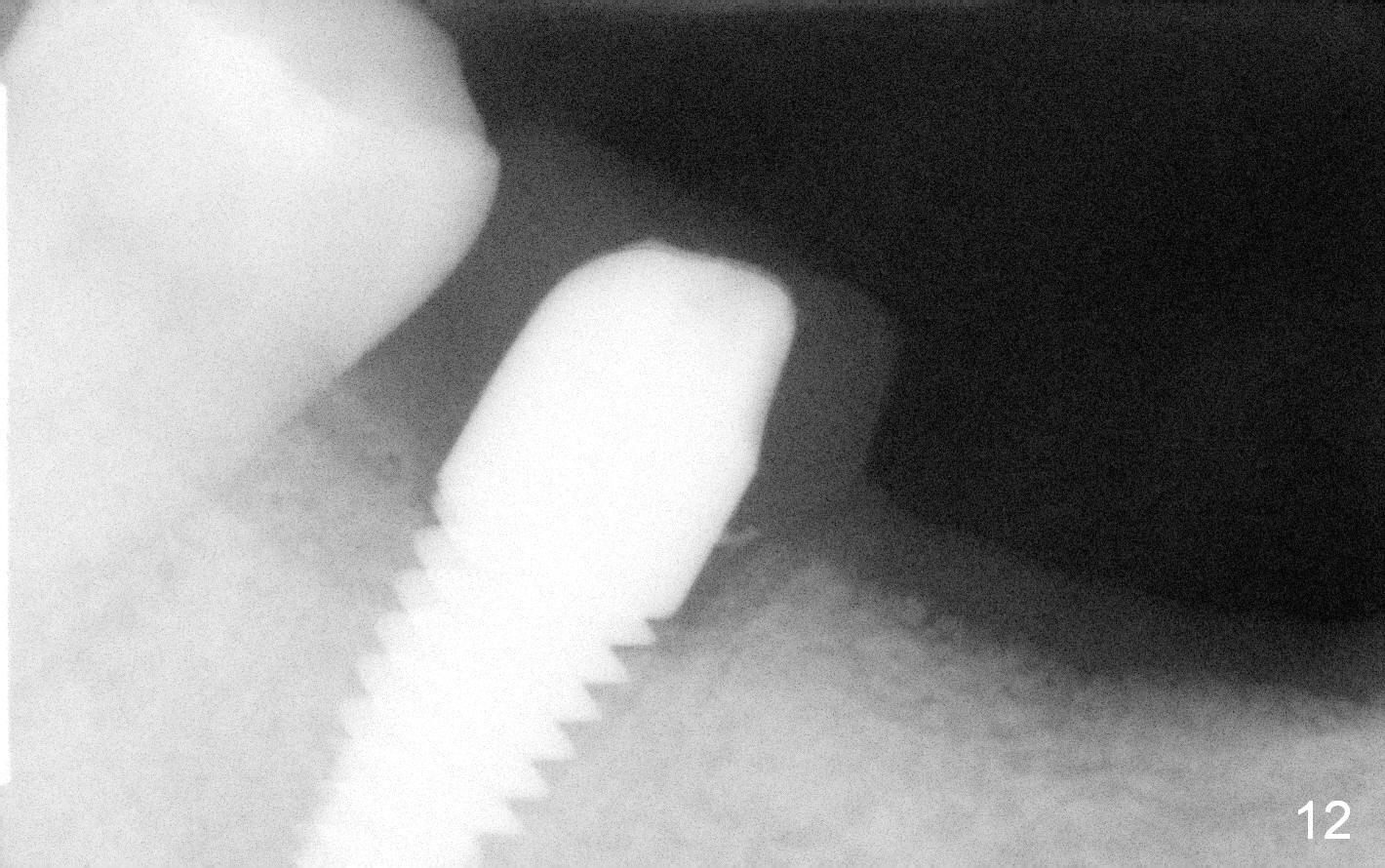
The patient returns for restoration 4.5 months postop. Anesthesia has long gone. It is still difficult to place No.1. sensor deep (Fig.12). On April 1, 2015, the permanent crown is cemented; the lower partial denture is seated smoothly.
Six months post cementation at #3, the patient plans to convert the lower RPD into implant restoration (#20, 25, 26, 28, 29).
Return to Professionals,
Lower Molar Immediate Implant,
Dr. Wu
Xin Wei, DDS, PhD, MS 1st edition 11/22/2014, last revision 08/19/2016