



 |
 |
 |
|||
 |
 |
 |
 |
 |
 |
 |
 |
 |
|||
 |
|||||
上颌第一双尖牙即刻植牙
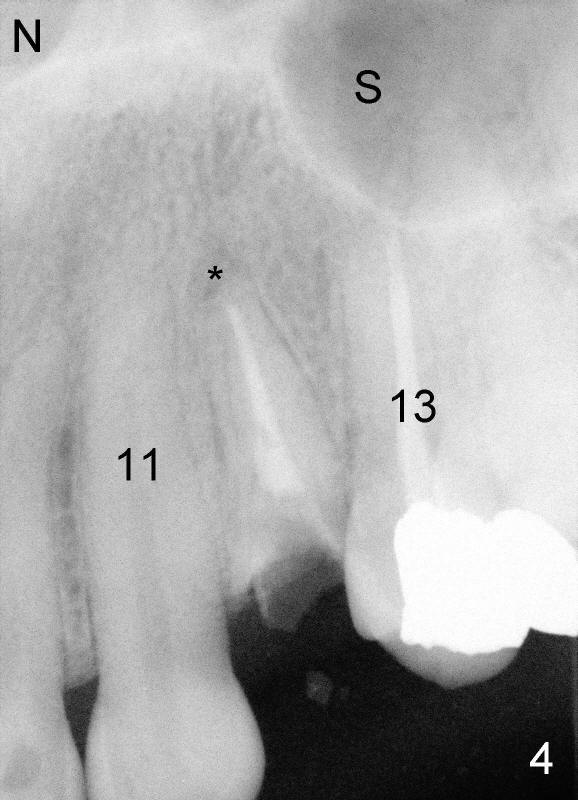
即刻植牙好像很深奥,其实并不是那样。植牙做几年后发现即刻植牙反而简单容易(1 2 3 4 5 6 7:为病人写的科普知识),拔牙和植牙一道做,省事,尤其那些害怕的病人,还可以少钻洞(osteotomy)。但是牙槽窝一般比植牙大,植牙后必须知道如何关闭伤口。另外必须有足够骨头取得植牙初步稳定,上颌第一前磨牙(图四:*)上方骨头比第二前磨牙长(图四:13,因为后者上方有上颌窦(S))。最后牙槽窝不应有感染,或者感染不严重。细菌容易在植牙表面生长,不容易被身体清除。
如果感染严重,最好先拔牙,四到六周才植牙,那时细菌被身体歼灭,牙槽窝口已关闭,造骨登峰造极(夸张些)。由于前牙以及双尖牙颊侧骨板薄,容易出现拔牙后骨质吸收,太难处理。所以现在本人观点(经过两三年摸索):即使感染严重,也应该立刻植牙(有些危险性,事先稍微给病人说明)。其实感染严重时,医生警惕性高,会认真刮治拔牙窝,除去肉芽组织,浸泡抗菌素,术后好像没有问题。植牙后感染往往是因为术前感染太隐蔽,拔牙后刮除不够仔细而致。
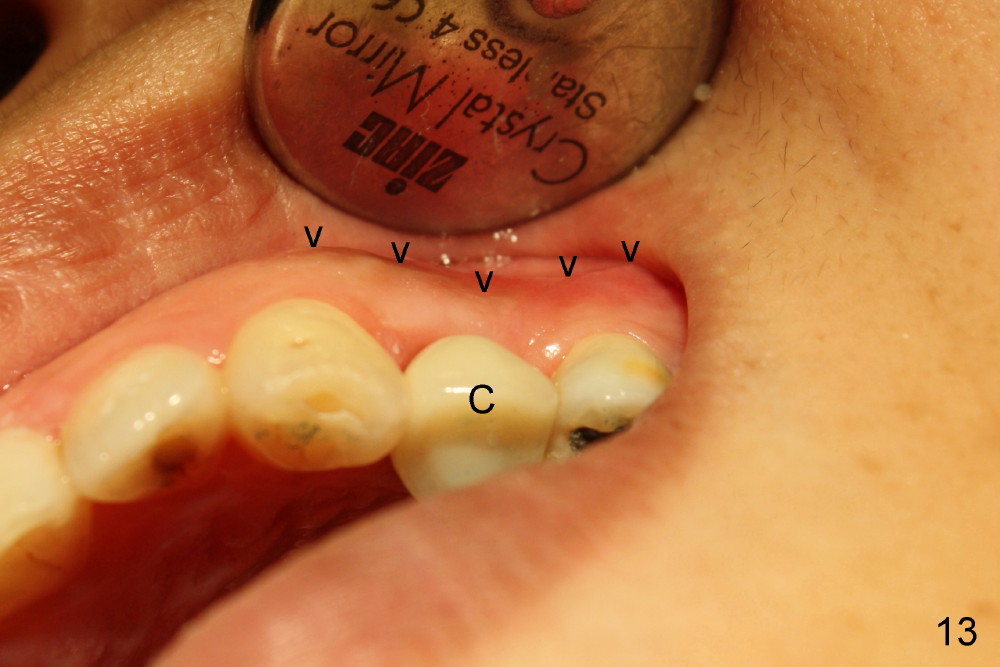
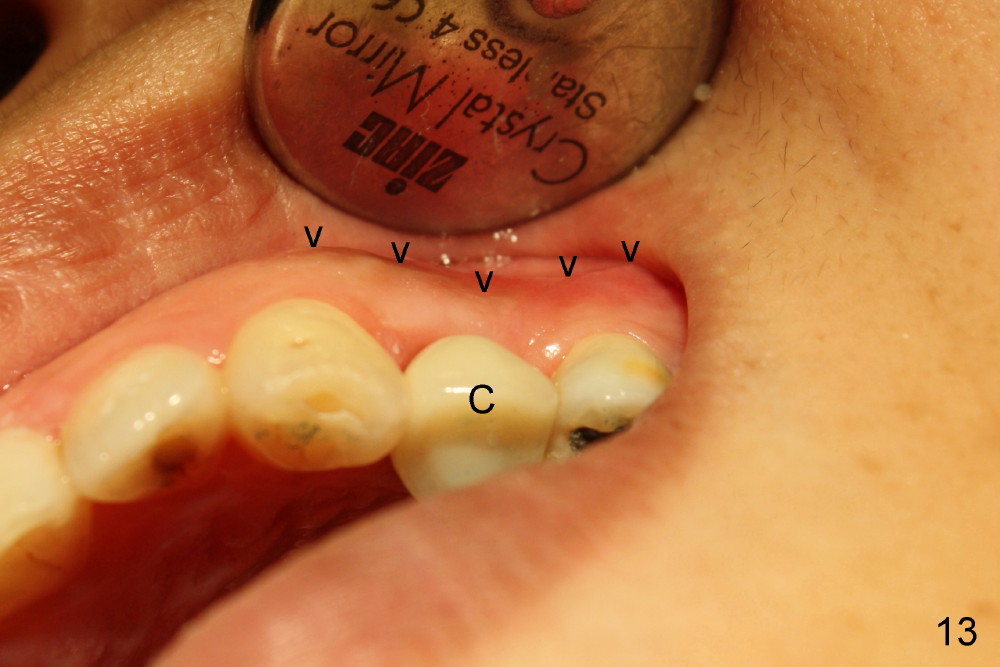
立刻植牙步骤见下面英文(图一至十一),让我们重点讨论为什么立刻植牙还不够完美。拖拖拉拉病人终于在五个半月时(由于害怕),装上牙冠(图十二,十三C),她不能发觉的是颊侧骨板仍无情地凹陷,无可奈何,但这时也不主要(图十三箭头),她和我共同之处:不喜欢牙龈退缩(图十二箭头),花了九牛二虎之力劝说她牙龈以后慢慢地会恢复正常,当时含糊其词说是她牙齿坏太久了,再次检查图一,我们可以发现术前牙龈已经不争气了,残根无法维持牙龈乳头。因此,美观区(包括前磨牙)不仅需要即刻植牙,而且需要立即修复。
Immediate Implant at the 1st Upper Premolar
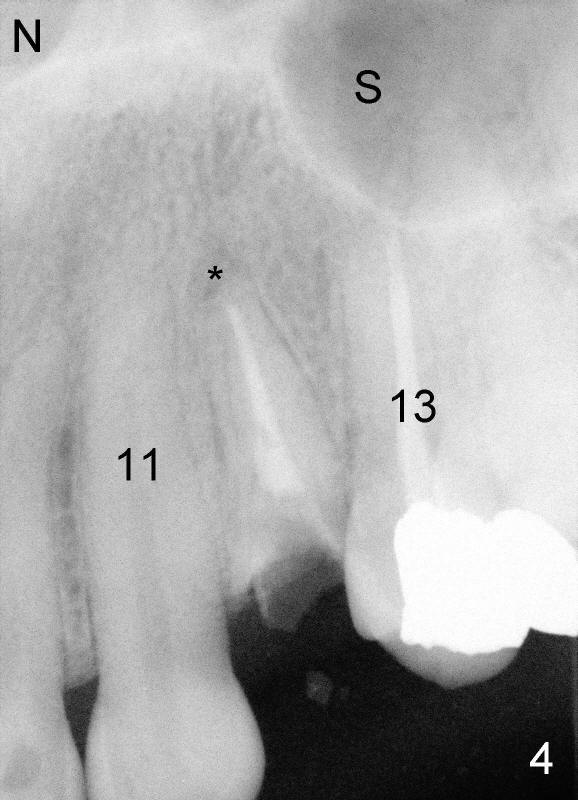
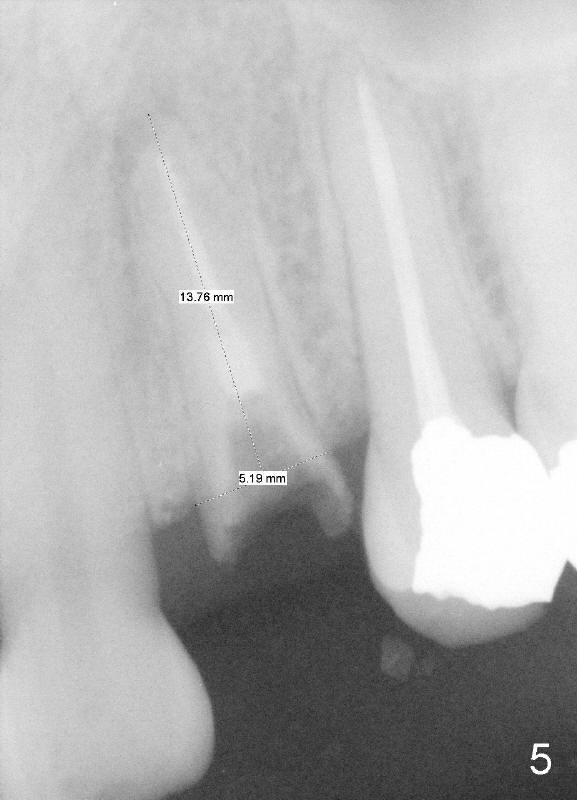
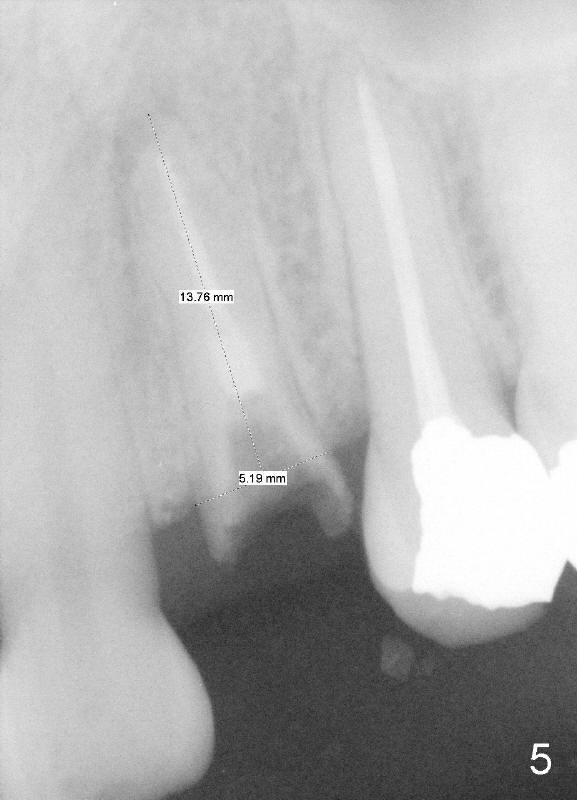
A 41-year-old lady has lost the crown of the upper left 1st premolar (Fig.1 (front view) *, Fig.2 (occlusal view)). An implant is planned to be placed immediately after extraction due to the fact that the patient is fearful of dentistry and that there is minimal periapical infection (Fig.4 *). There is plenty of bone between the apex and the nasal cavity (N) and the maxillary sinus (S). Preoperative measurement of the residual root reveals the length ~14 mm and the mesiodistal width 5 mm. An implant of 5x20 mm is prepared. At least 4 mm of osteotomy in new bone is required for initial implant stability.
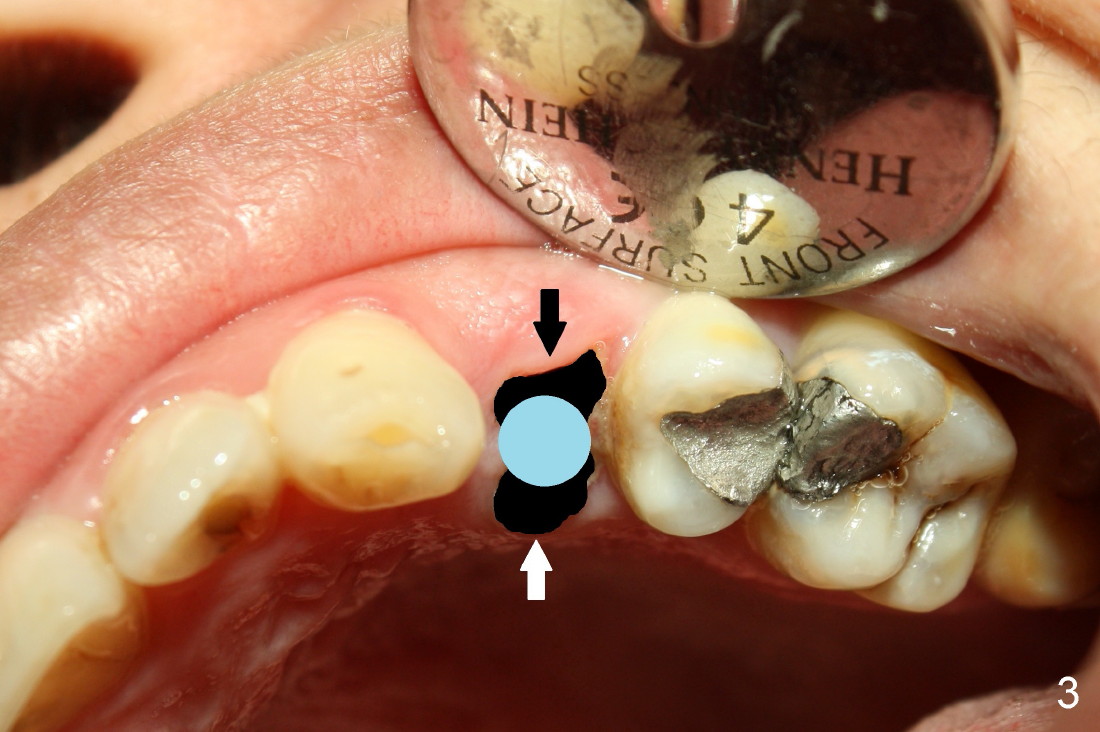
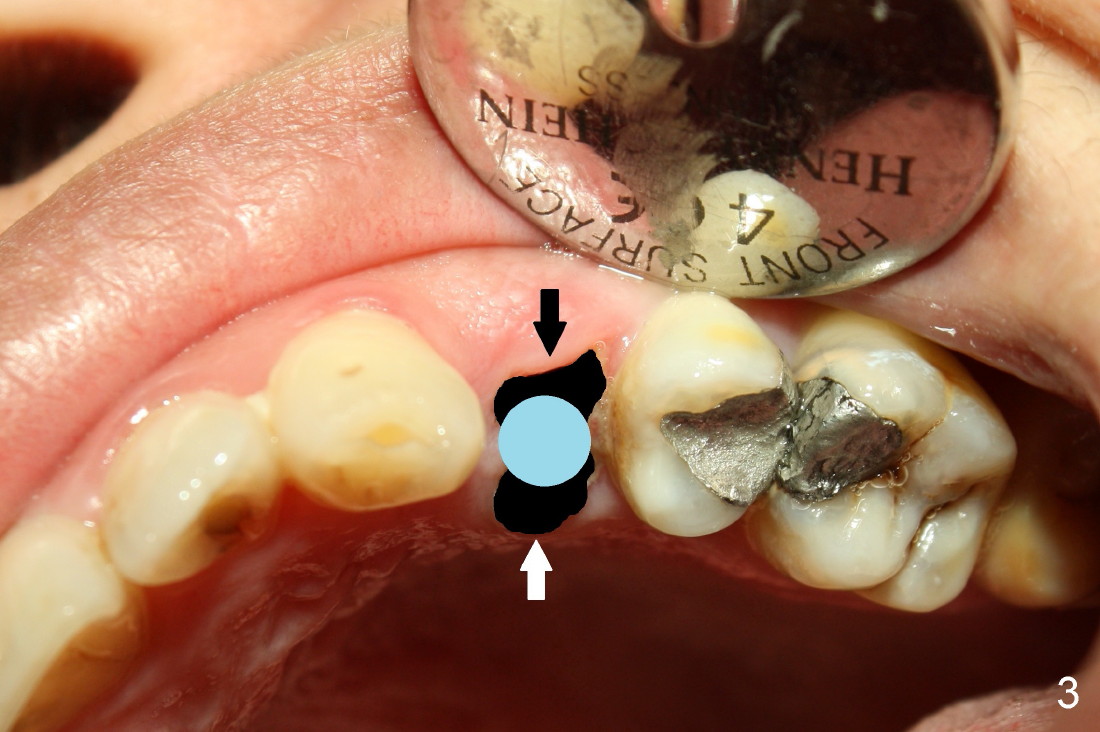
Fig.2 shows that buccopalatal dimension of the root stump (blue line) is larger than the mesiodistal one (orange line). The socket is oval after extraction (Fig.3 black area, whereas the implant (5 mm in diameter) is rounded (blue). There are spaces buccal and palatal to the implant. To prevent postop infection, the spaces should be closed by bone grafting and advancing the buccal and palatal gingival flaps (black and white arrows).
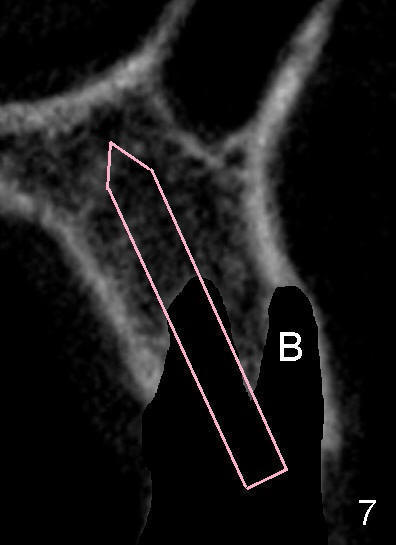
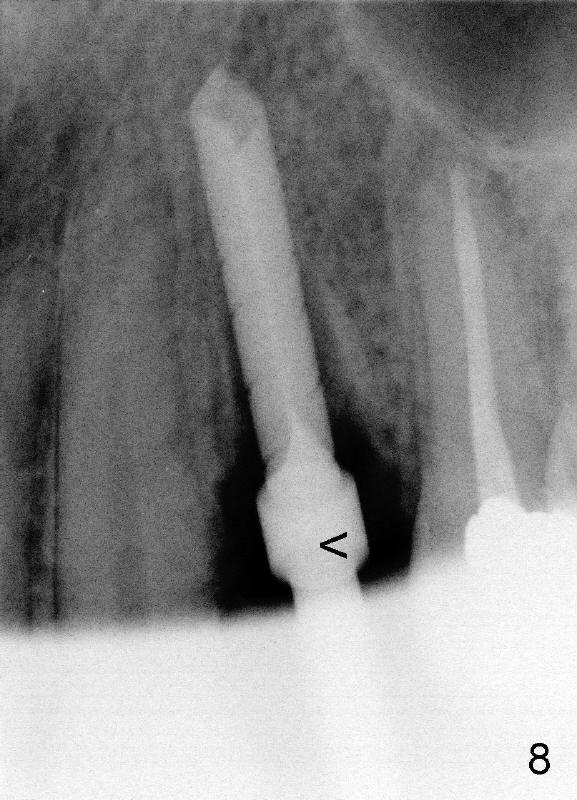
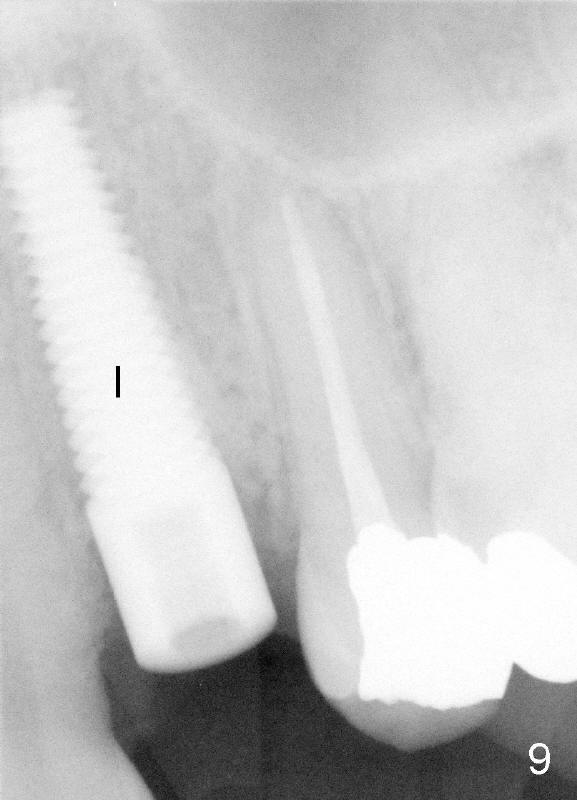
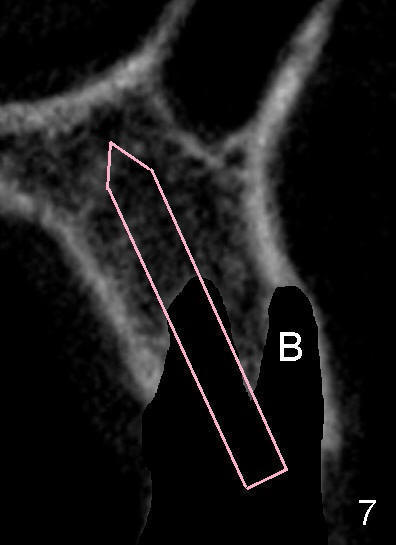
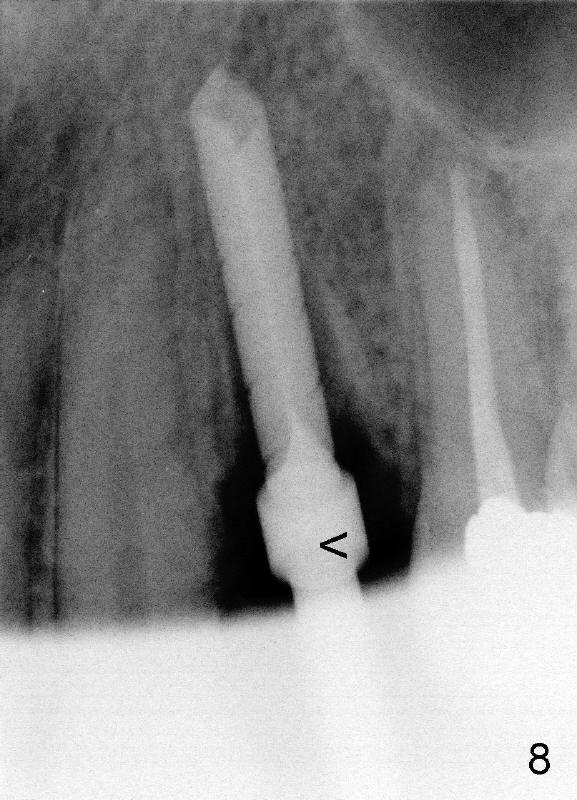
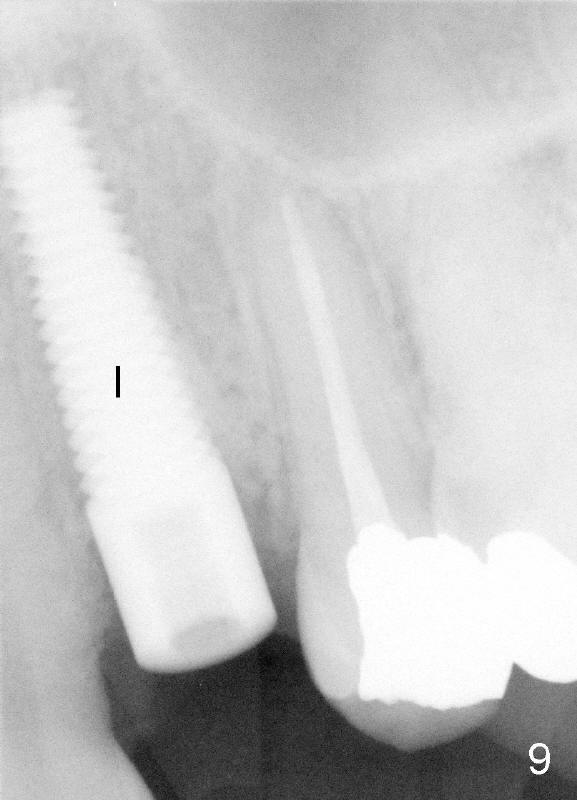
Extraction confirms that this tooth has two fused roots (buccal and palatal (B, P), similar to Fig.6 cross section of CT scan (different case)). Since the palatal root is in the center of the bone, initial osteotomy is created (Fig.7 (illustration) pink) in the palatal (not buccal, B) socket after extraction. Fig.8 shows intraoperative periapical X-ray of 2.5 mm drill (reamer at 50 rpm (rotation per minute) at the depth of 20 mm (from arrowhead to the tip of the drill). It appears that there is no perforation toward the sinus or the nasal cavity. A tapered implant (5x20 mm) is shown immediately postoperative (Fig.9 I).
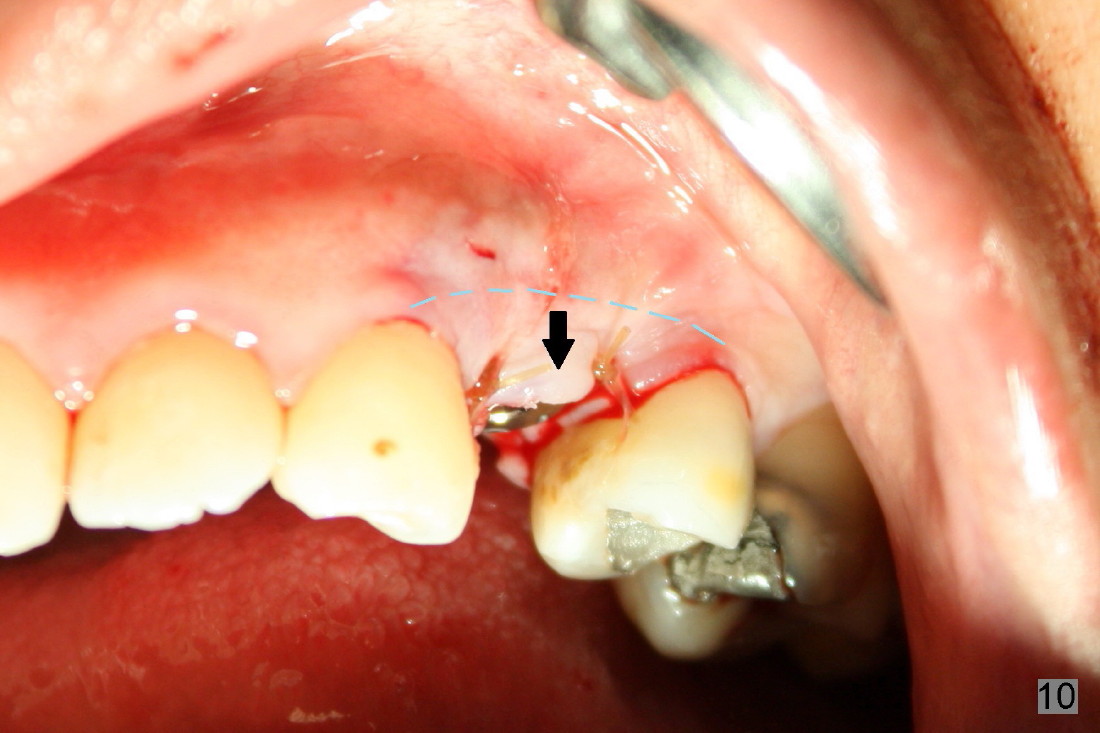
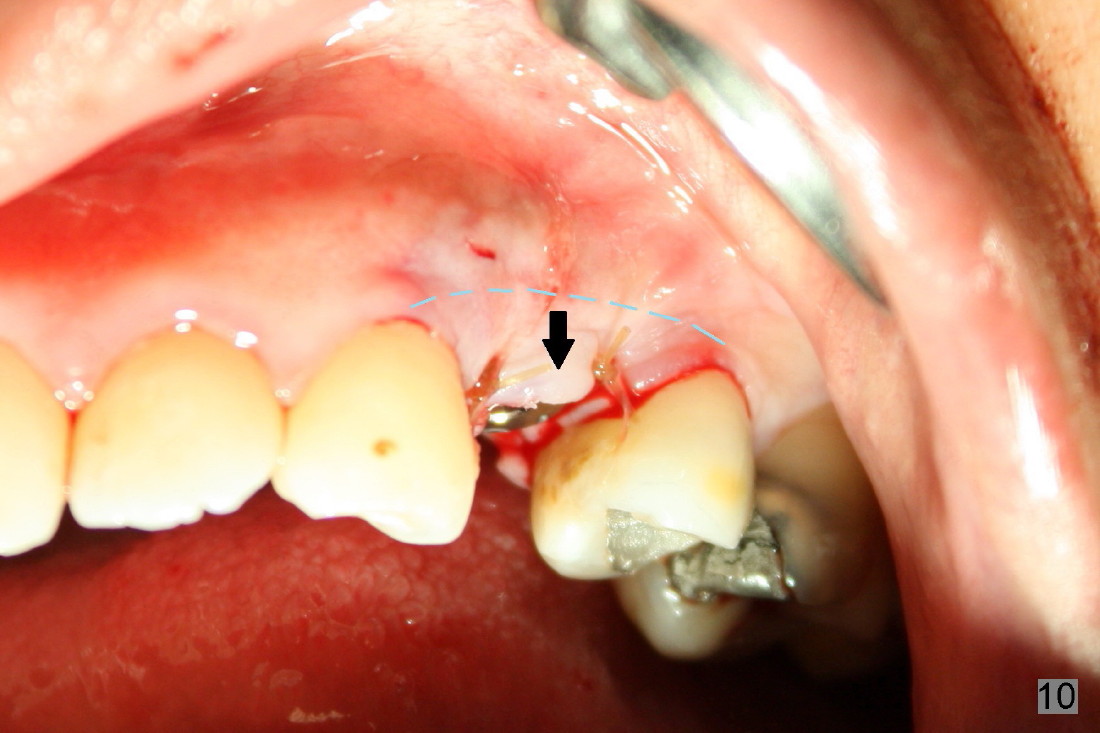
Bone harvested from the reamers for osteotomy is used to fill the gaps between the buccal and palatal walls and the implant (Fig.2, 2' and 4 in Prevent Post-Implant Infection). Then the gaps are closed by advancing buccal and palatal flaps with sutures. The buccal flap is advanced (Fig.10 arrow) after its periosteum is underscored (dashed line). For the advancement of the palatal flap (Fig.11 white arrow) , two release incisions are made (black arrowheads) in addition to the periosteum being underscored (dashed line). Return to Classmates
Xin Wei, DDS, PhD, MS 1st edition 12/02/2012, last revision 10/20/2013