
.jpg)

.jpg)
.jpg)

 |
 |
 |
|
 |
.jpg) |
 |
 |
 |
 |
.jpg) |
.jpg) |
 |
 |
 |
|
Osteotomy in Tripod Septum
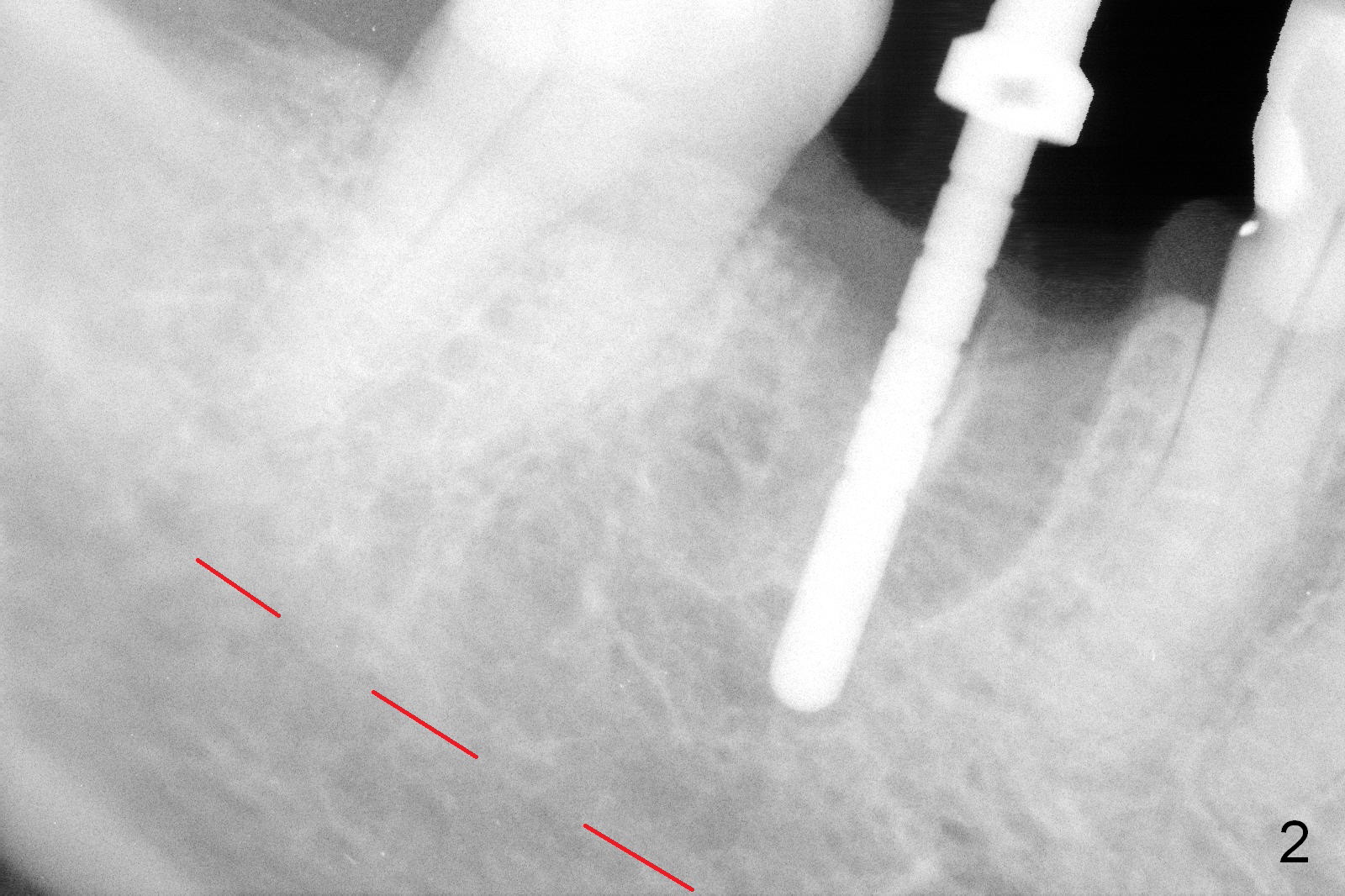
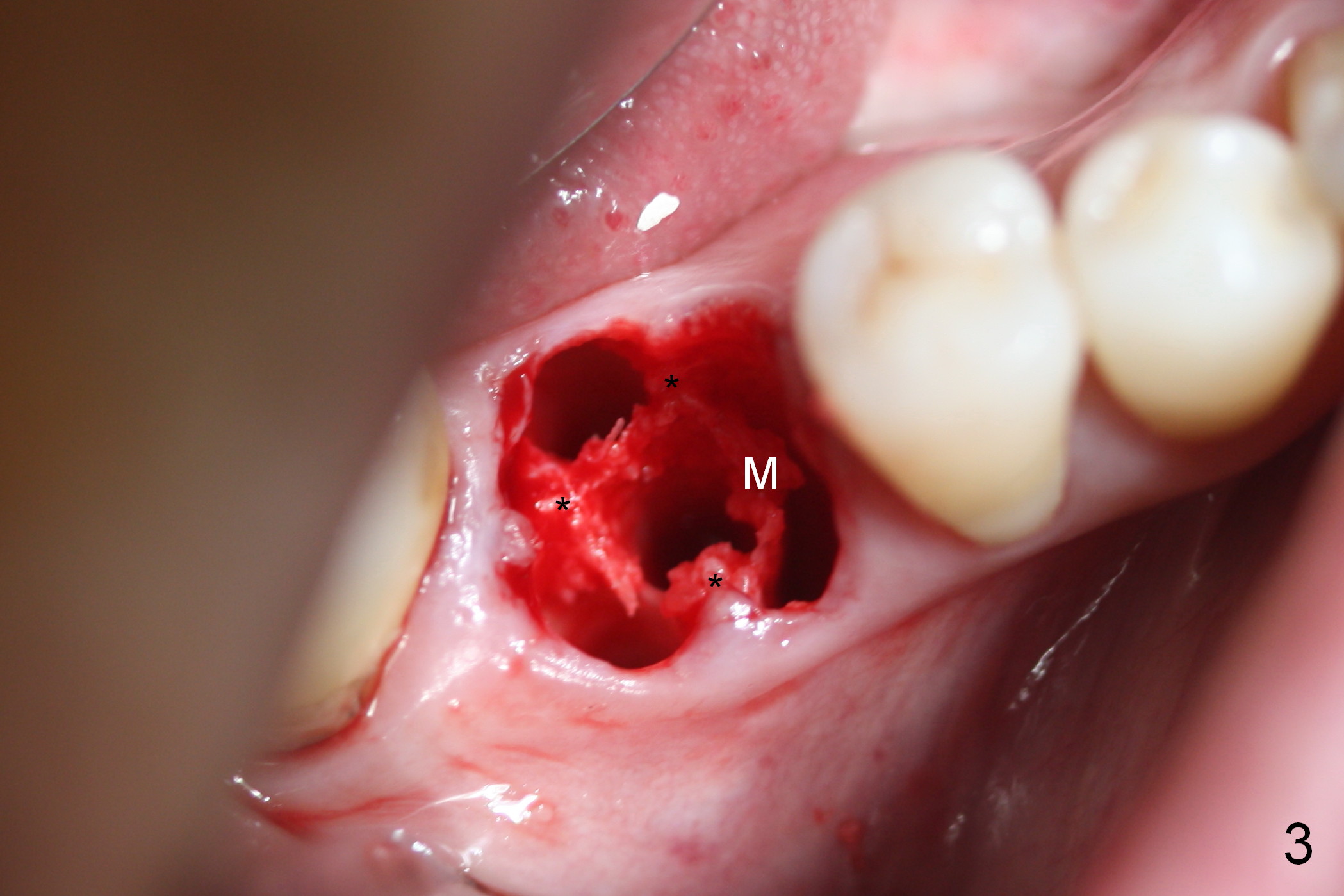
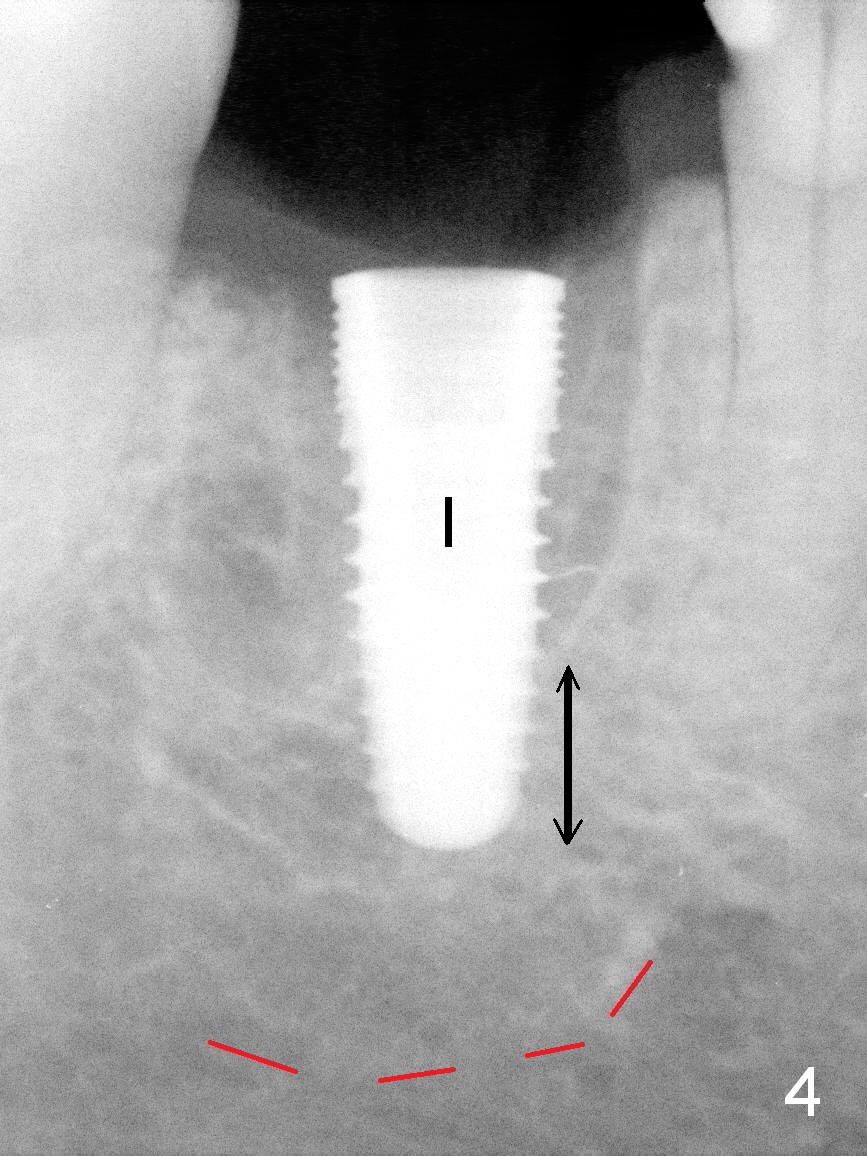
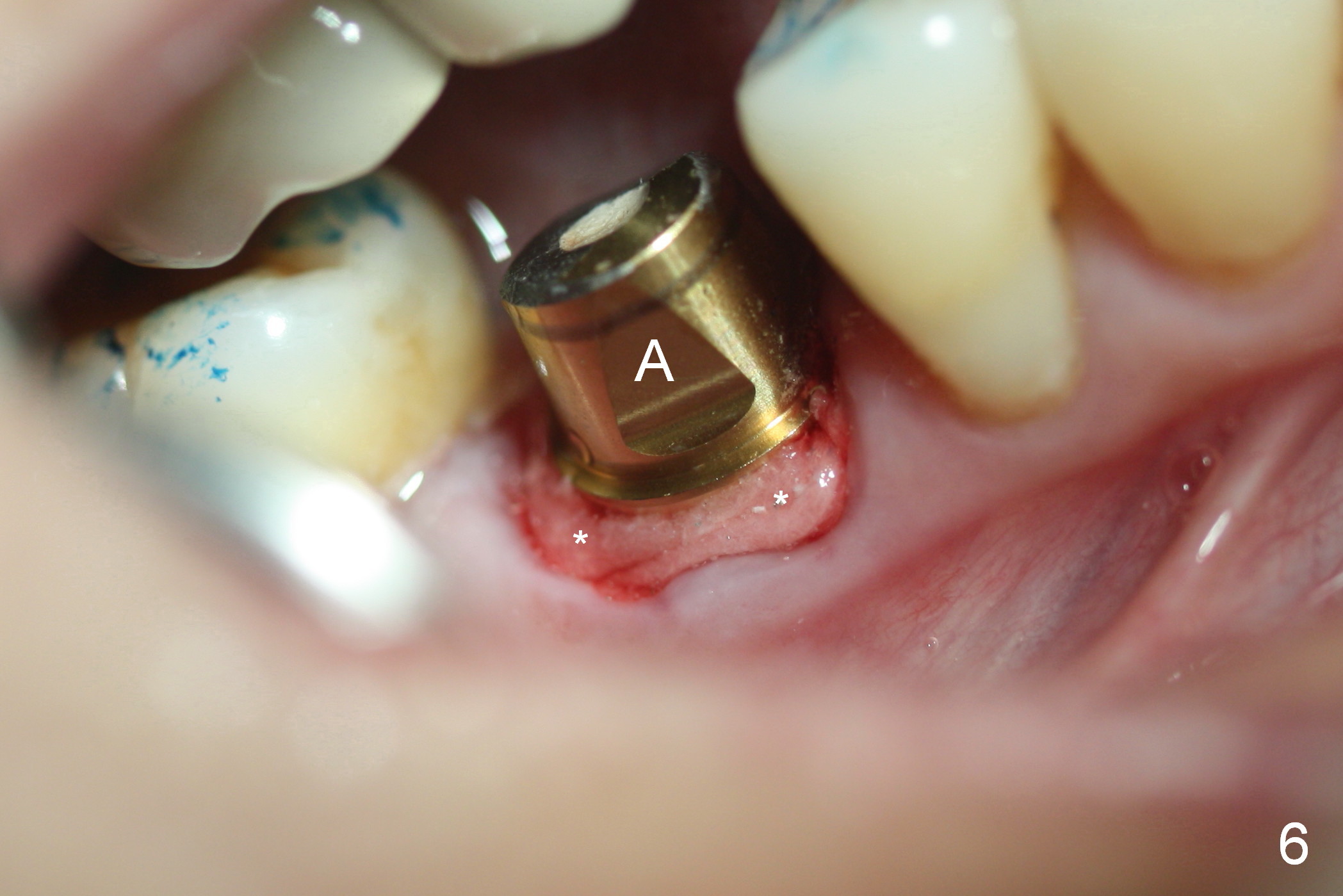
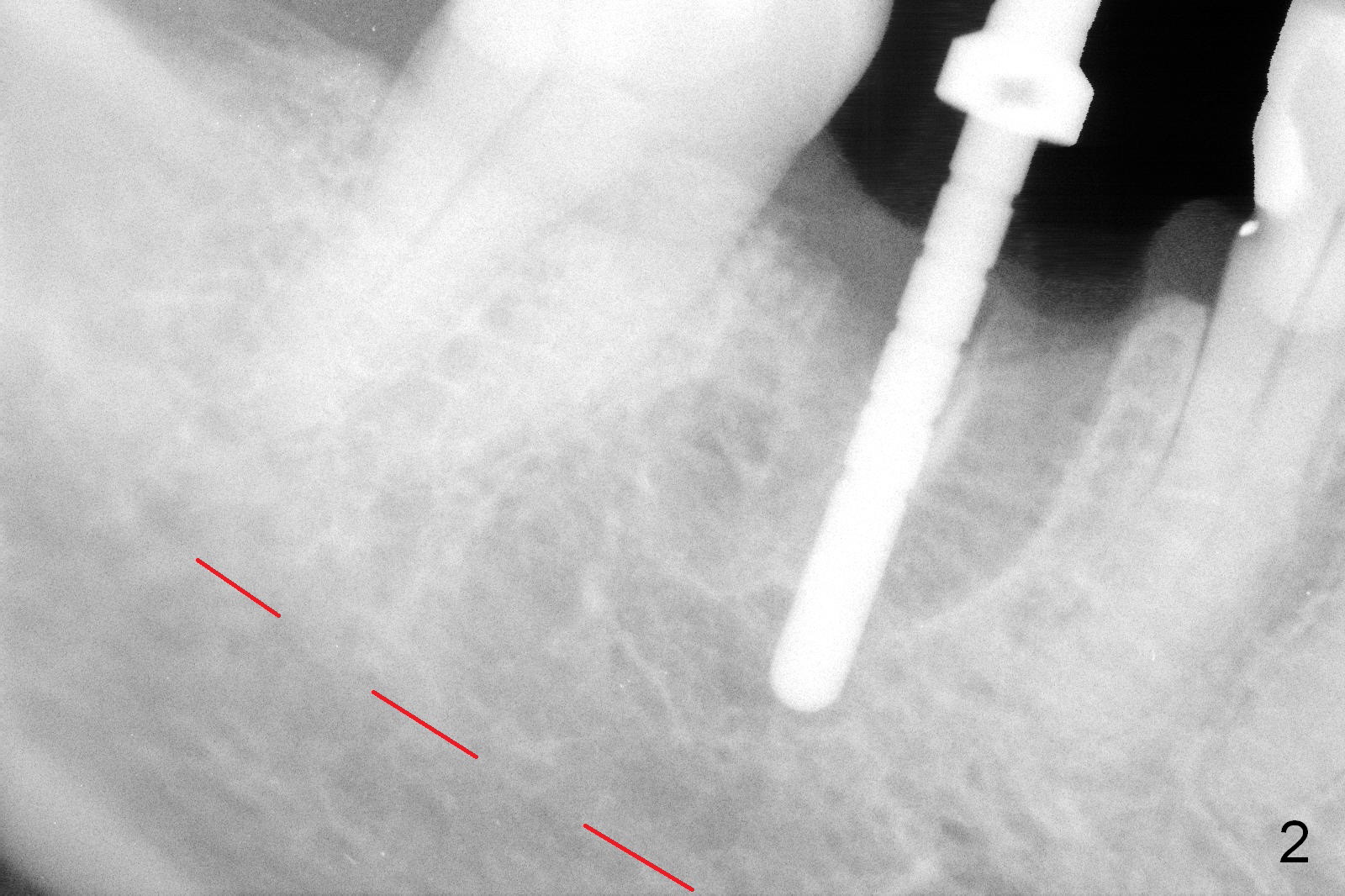
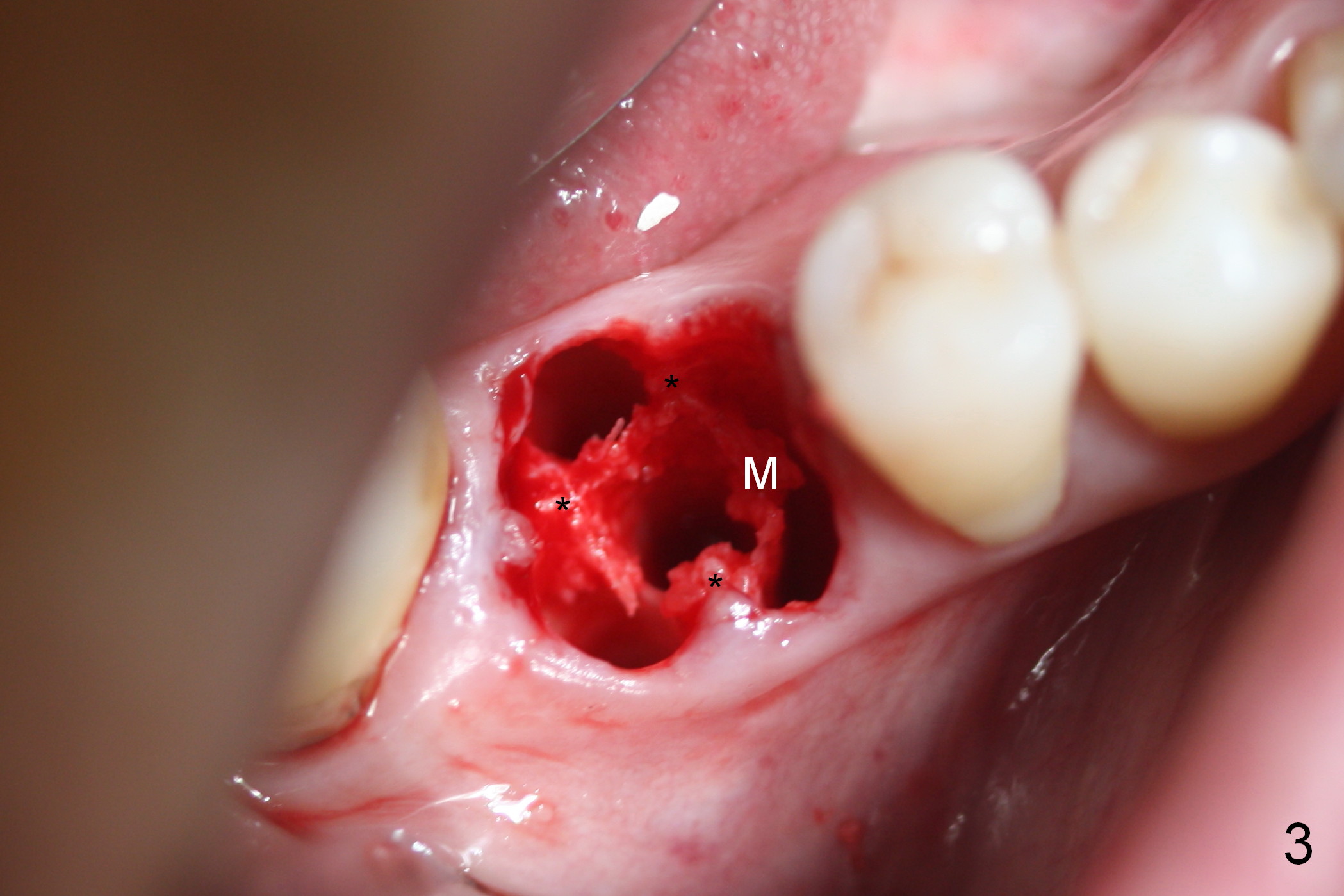
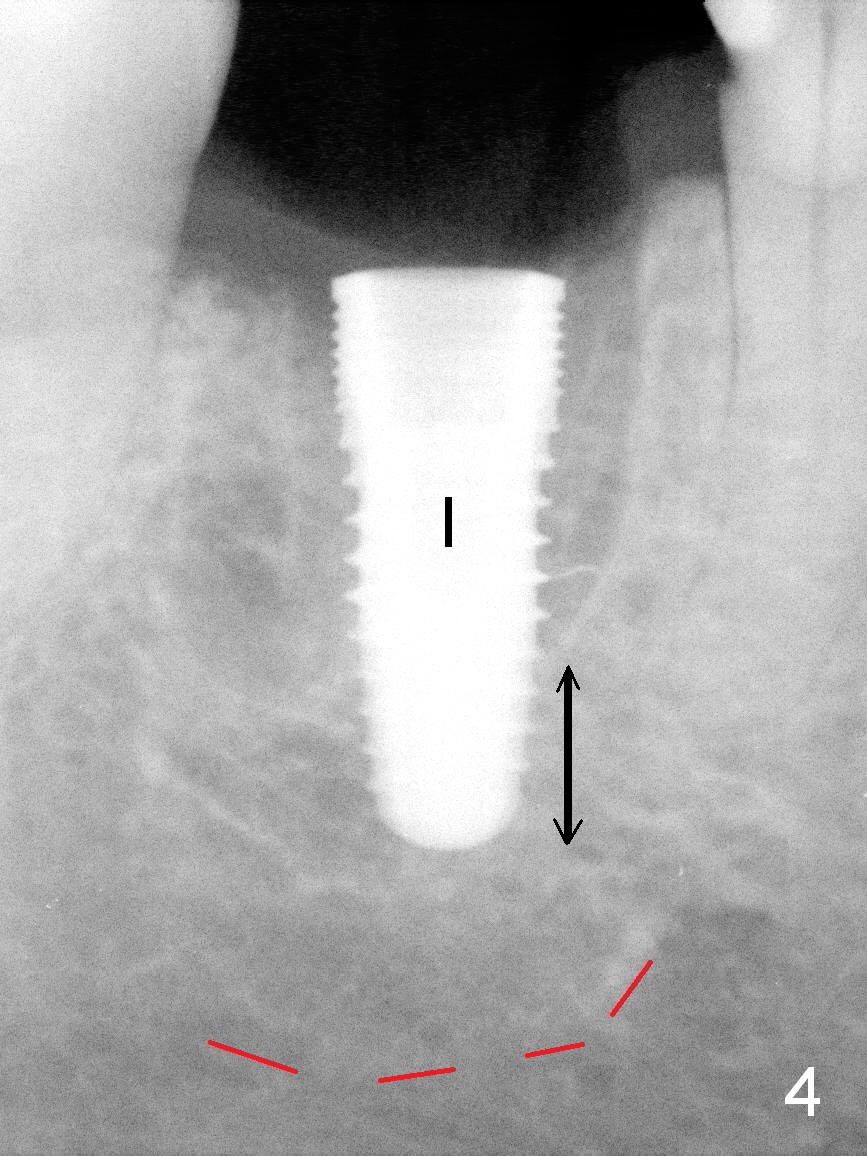
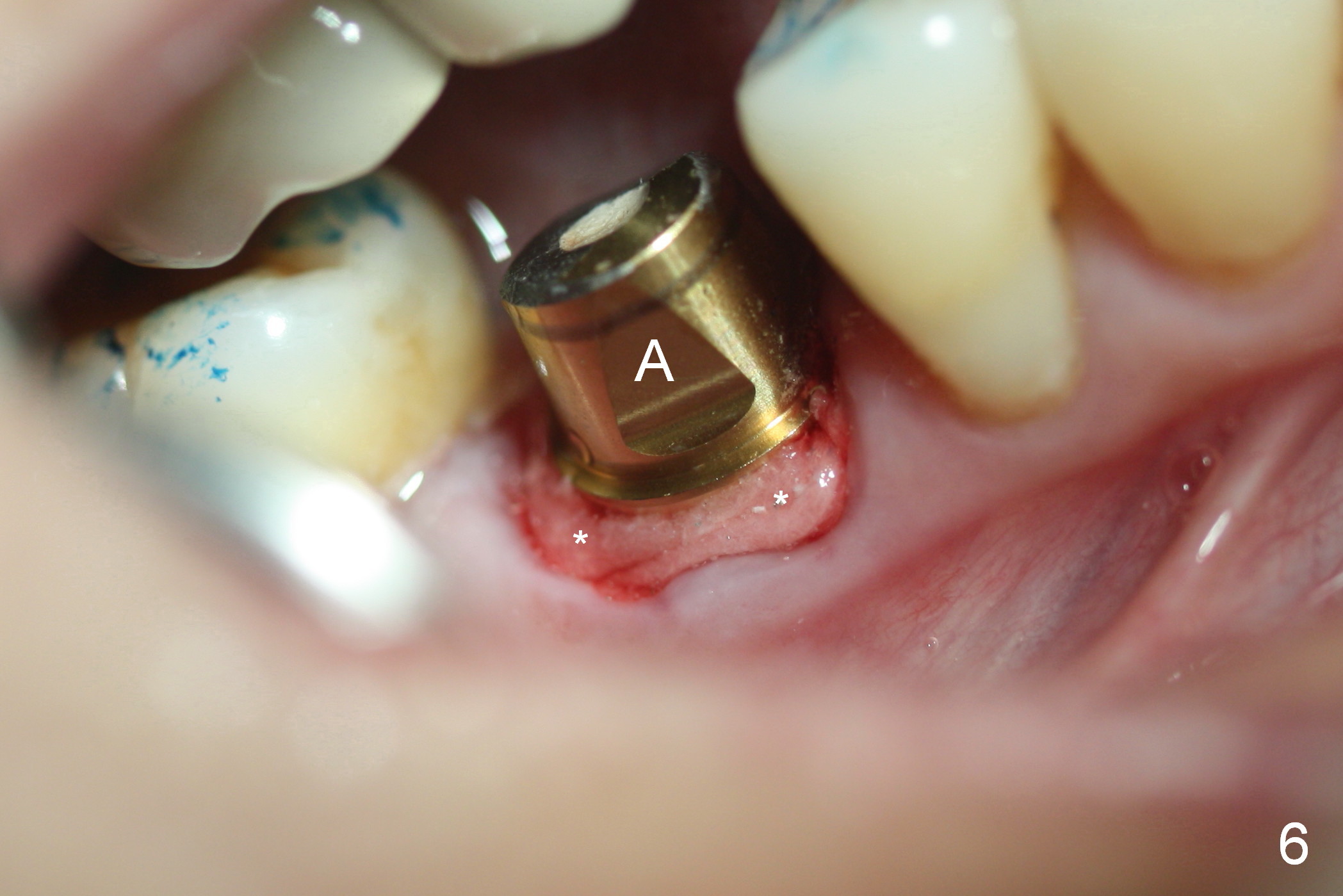
As planned, the fractured roots are removed by sectioning. The septum has 3 struts (tripod, Fig.1 black *). Osteotomy starts in the middle of the septum (white *). The 1st intraop PA is taken with a parallel pin after 2 mm pilot drill at 11 mm (Fig.2). Osteotomy is enlarged by 2.5 and 3 mm reamers at 12 mm, followed by 4.5 and 5 mm taps at ~ 11 mm. At this time, the mesial wall of the osteotomy has started breaking down (Fig.3 M). A 5x12 mm implant is placed (Fig.4 I); apically there is ~ 4 mm new bone (double arrows); coronally the implant is stabilized by the tripod septum (Fig.3 *). The insertion torque is approximately 55 Ncm; at the same time, there is enough clearance from the superior border of the Inferior Alveolar Canal (red dashed line). A 7.8x5(3) mm is placed immediately (Fig.5 A), followed by placement of bone graft (*). At the top of the latter is Collagen dressing (Fig.6 *), which is kept in place by an immediate provisional. To have primary stability, the implant does not need to be large or long. Anatomic structure (tripod septum in this instance) is critical; underprep is a must. A large abutment and an immediate provisional close the socket opening.
A month 10 days postop, the gingiva heals around the abutment when the immediate provisional is removed for trimming. The papillae are maintained (Fig.7 *, which does not happen when an implant is placed at healed site, #19 of the same patient). It appears that the abutment should change to one with cuff 1 mm shorter.
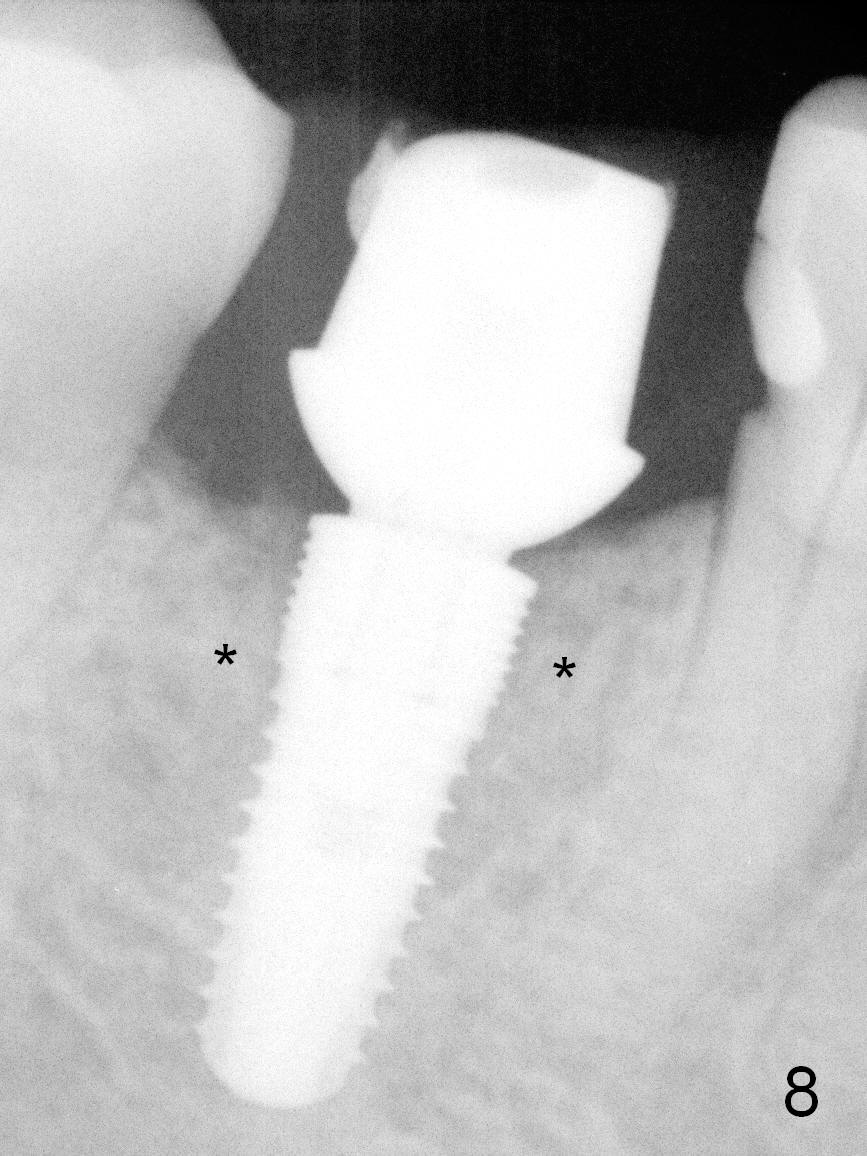
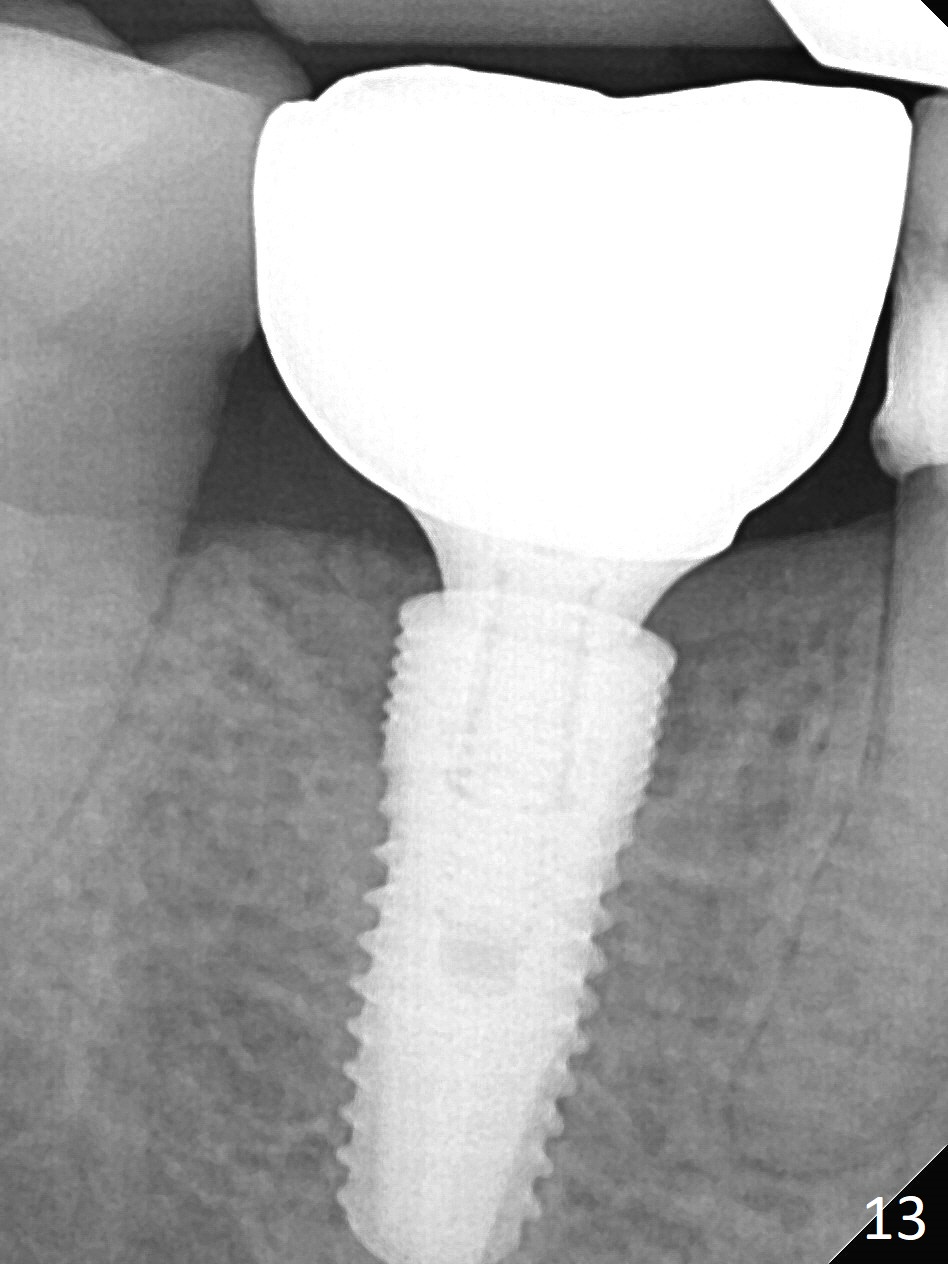
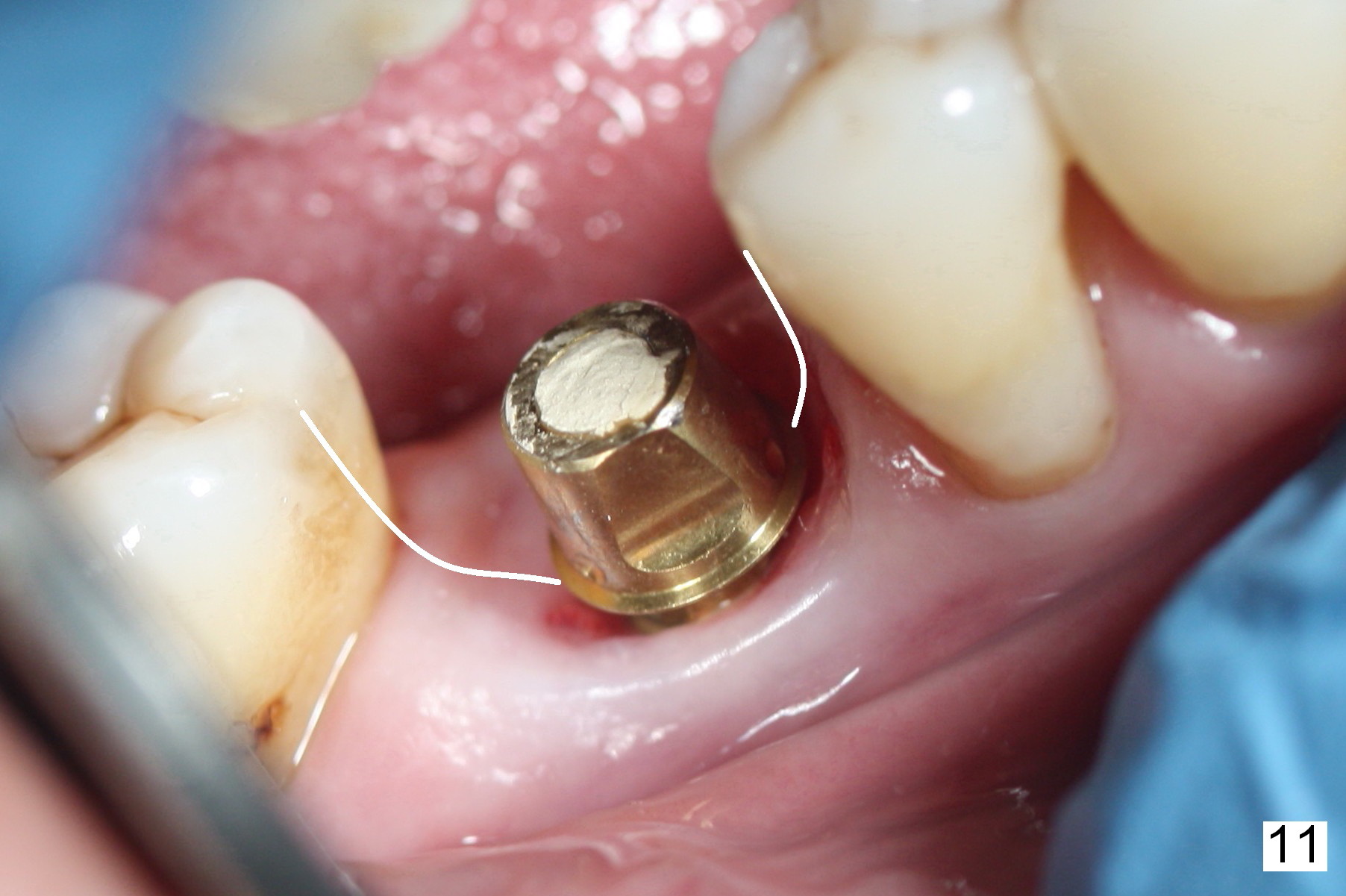
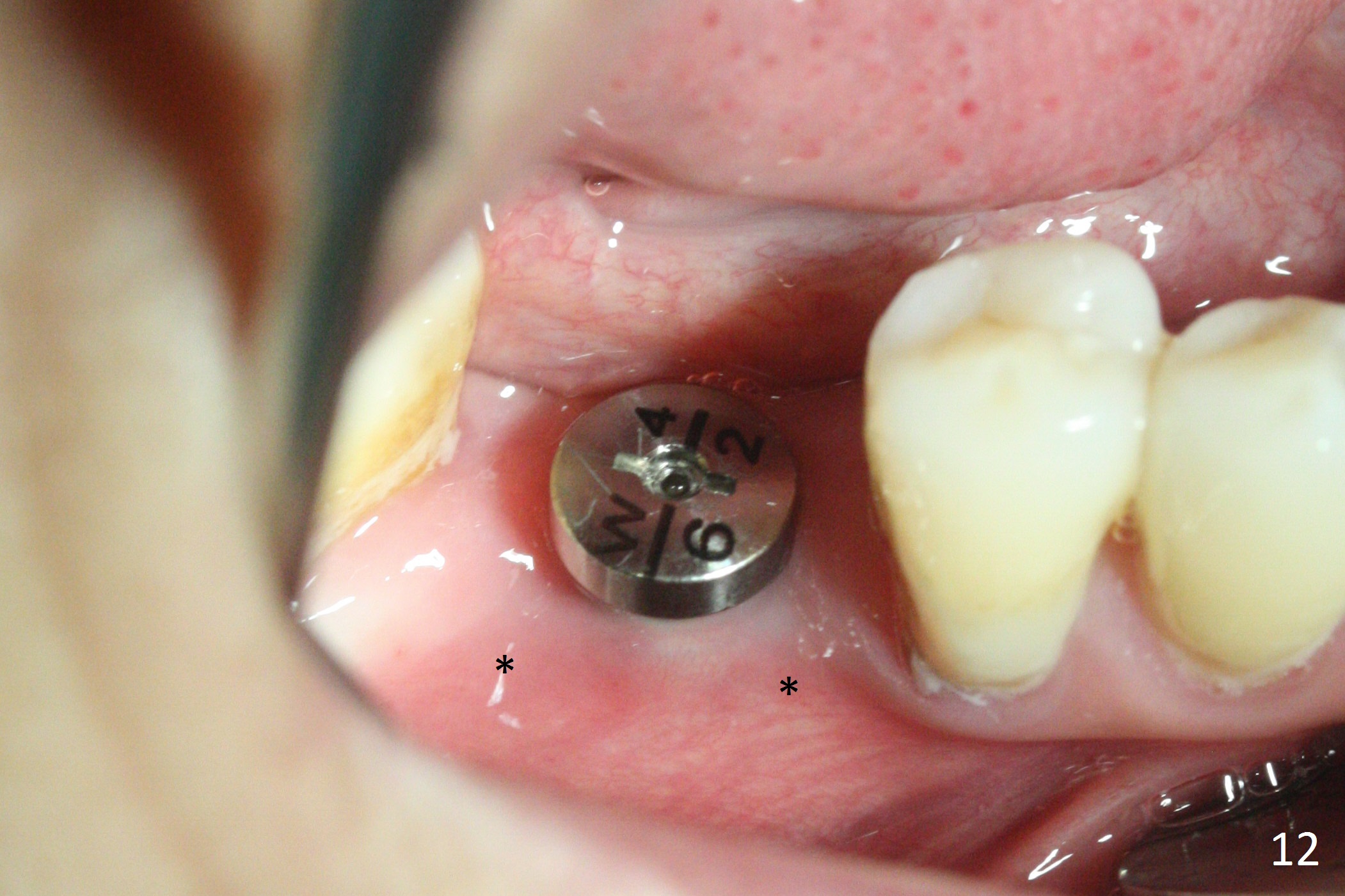
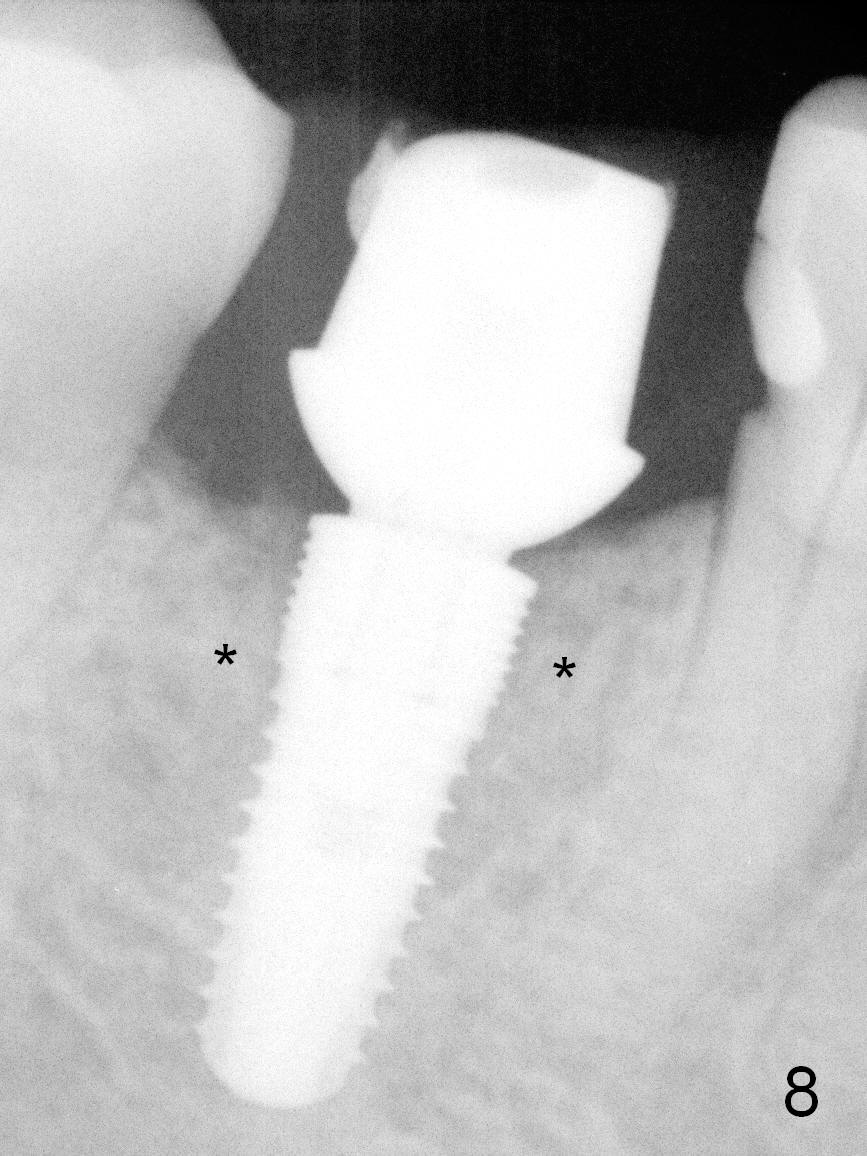
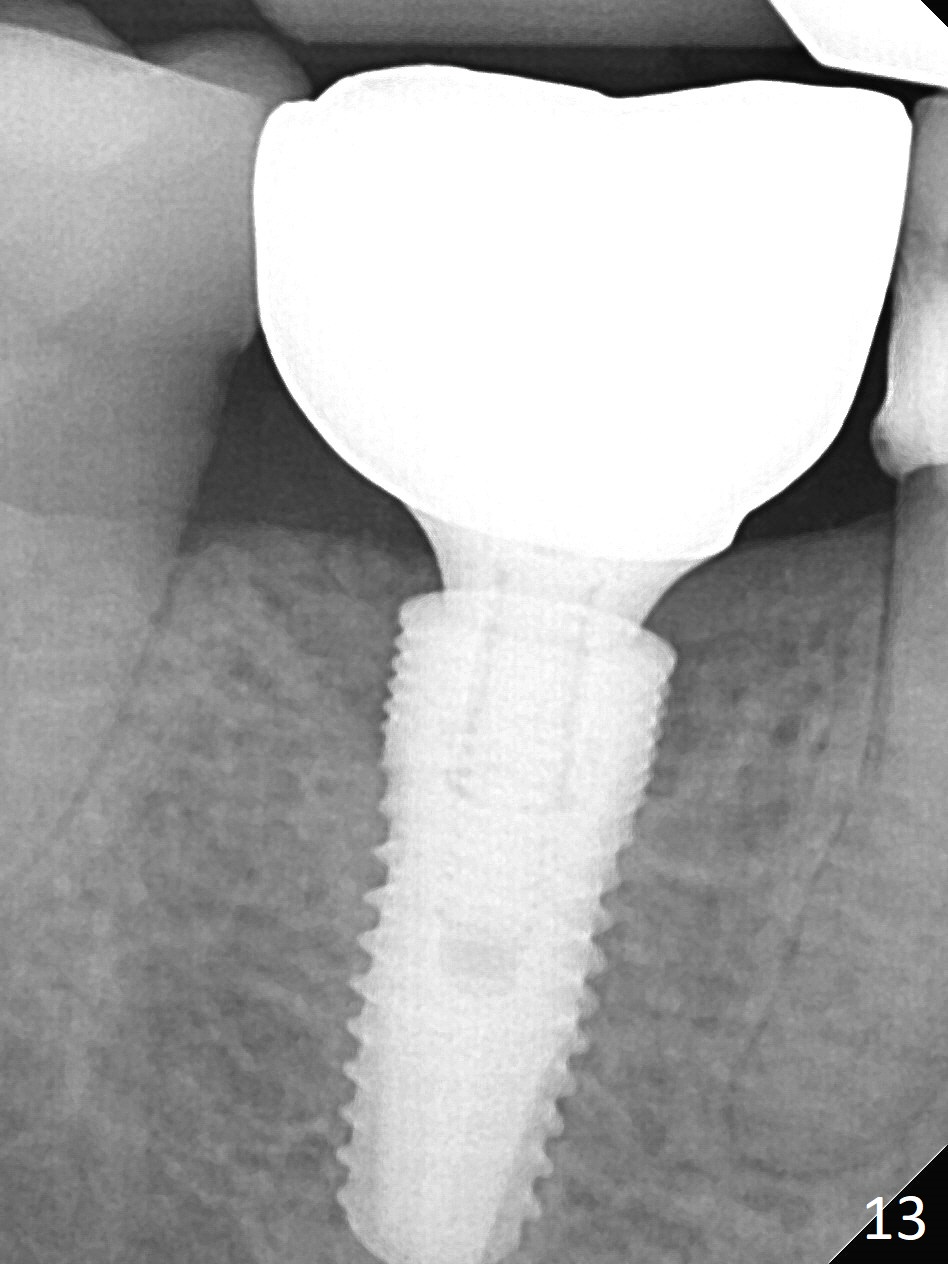
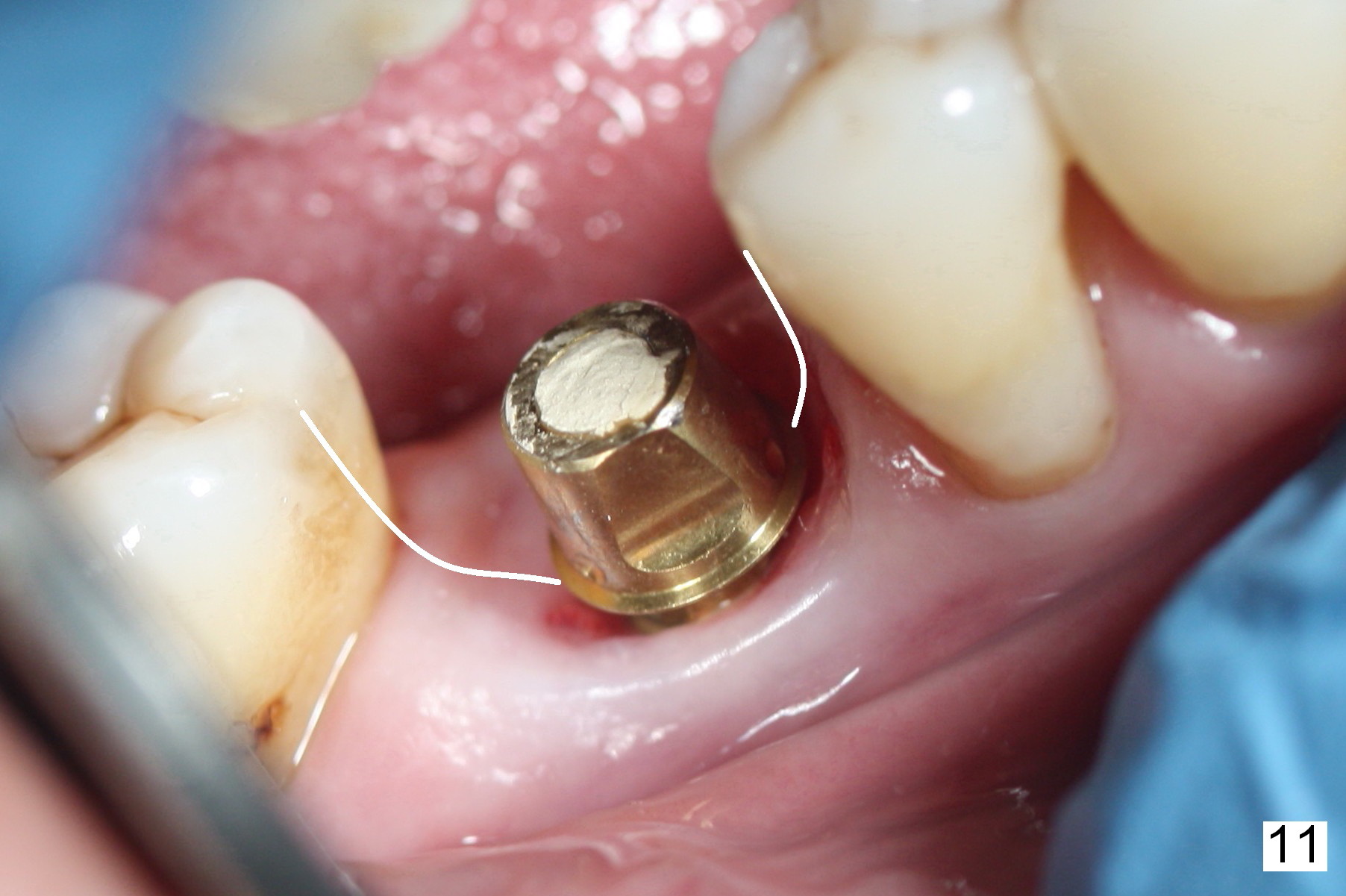
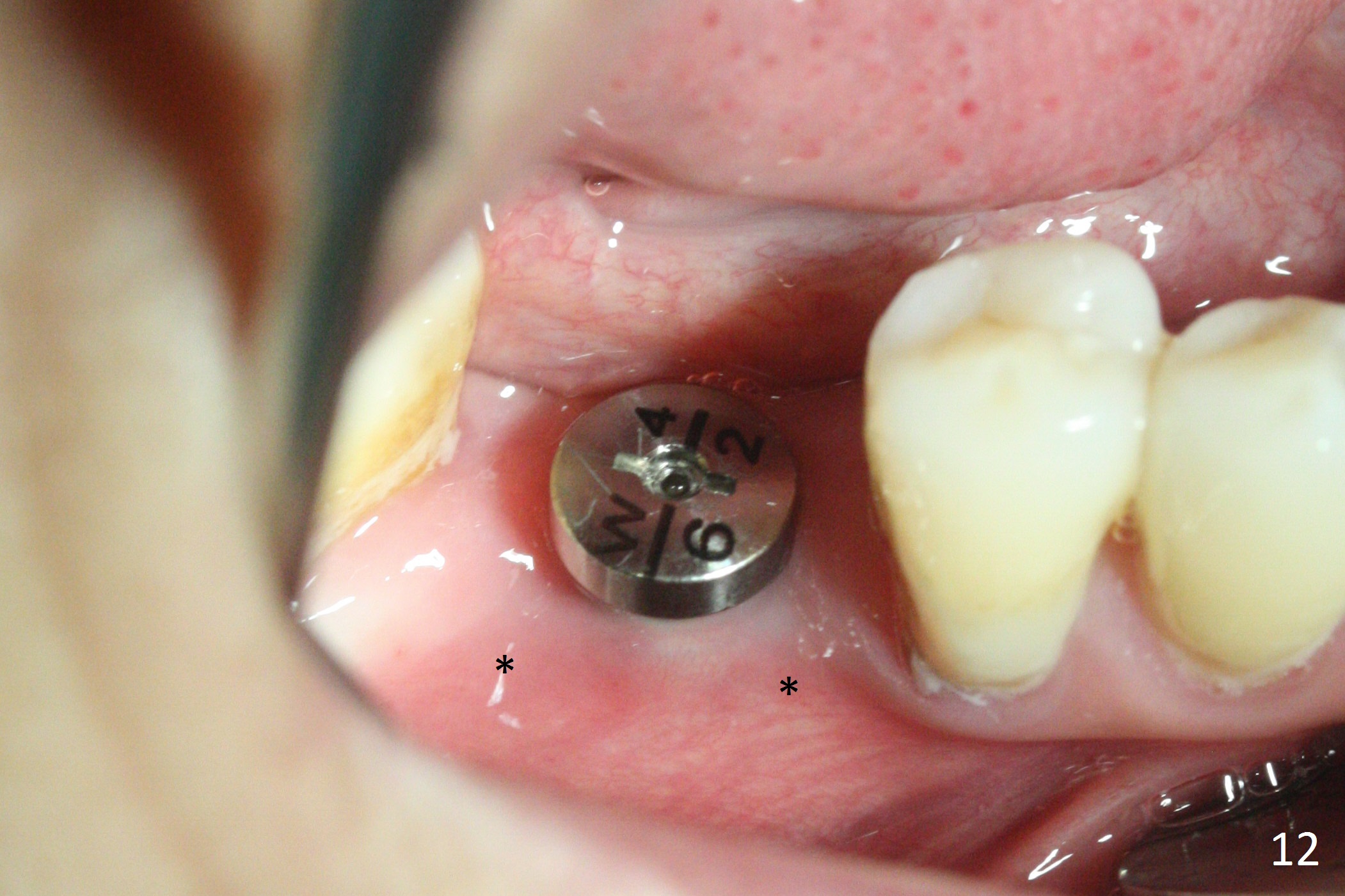
The patient returns for final restoration 2 months 20 days postop. Bone density in the former mesial and distal sockets increases (Fig.8). There is occlusal perforation of the provisional. She has started to chew on the right side 1 month post implant placement, because of treatment on the left. The buccodistal abutment margin is coronal to the gingival one (Fig.9). The abutment margin looks better when the abutment is changed from 7.8x5(3) to 5.8x4(2) mm (Fig.10). The apical end of the final crown should be bulky enough to close the gingival embrasure (Fig.11 white lines). The buccal gingival recession must be due to loss of the buccal plate post extraction. Therefore the implant should have been placed more lingually. The patient is not pleased with the buccal plate atrophy 1 year 9 months postop (1 year 2 months post cementation, Fig.12, when the crown is repaired due to loose proximal contacts). Probably the 5 mm implant is small for the site or bone graft was insufficient post extraction. Two years post cementation, there is bone loss at crest (Fig.13) with buccal thread exposure (Fig.14).
For redo or bone graft, prepare PRFx2 (sticky bone), 5/6 and 6/7 trephine burs and 4.5x13(4) mm Magicore. The implant will be placed lingual so that the trajectory will be not so good. Magicore has no tendency for screw loosening.
Return to Lower Molar Immediate Implant,
Posterior Immediate Provisional,
14,
#19 Healed Site,
Technicians,
Armaments
Trajectory II
Xin Wei, DDS, PhD, MS 1st edition 08/23/2015, last revision 08/27/2019